Year: 2001 Vol. 67 Ed. 5 - (21º)
Relato de Casos
Pages: 738 to 741
Nasal ameloblastoma. Literature review and report of two cases
Author(s):
Washington L. C. Almeida 1,
Alex C. Costa 2,
Carlos R. T. Góis 2,
Marcelo C. C. Almeida 1,
Milton P. C. Moura 1,
Achiléa A. L. Bittencourt 3
Keywords: ameloblastoma, nasal cavity, chronic sinusitis
Abstract:
Ameloblastoma is a very unusual tumor in the nasal cavity. It arises from the odontogenic epithelium and extends up to the maxillary sinus, orbits and skull base. We have presented two cases of ameloblastoma, both in the right nasal cavity, associated with nasal and sinusal symptoms, and reported the main surgical and clinical findings.
![]()
INTRODUCTION
Ameloblastoma is a benign tumor that originates from the odontogenic epithelium and it is normally presented at the mandible level2. The first confirmed case of ameloblastoma dates from 1811, reported by Petrus Koning. The first description that the tumor had a special maxilla-mandible cyst form was made in 1827 by Cuzack. The term ameloblastoma was introduced in 1930 by Churchill, because who thought that the formation of dental enamel was not present in the lesion. Currently, different names have been proposed, such as adamantinoma, adamantine cystadenoma, epithelial odontoma, embryoblastic odontoma, adamantinic epithelioma, and multilobular cyst2.
Generally speaking, ameloblastomas represent approximately 1% of the oral region tumors, and 80% of the cases are mandibular, predominantly located at the level of the mandibular angle, whereas the remaining 20% are found in 'the maxillary bone, especially at the level of the canine and molar teeth; the tumors may extend into the maxillary sinus, nasal cavity, orbit and skull base2,10,14,9.
The tumor may be present at any age range: there are descriptions of cases at two montlls of age up to 80 years, with predominance of the third and fourth decades of life. As to gender, there seems to be equal frequency, although some authors indicate a female predominance9,1,5. As to race, it is more frequently detected in Black people 2,17,9,8.
Ameloblastoma normally grows slowly and persistently, invading the bone marrow with pseudopodes in order to enable recurrence after inappropriate removal of the tumor9. Its differential diagnosis should be made with giant cell granuloma, odontogenic myxoma, multilobular follicular cyst and inverted papilloma2,12.
There are a number of histopathological types of ameloblastoma and they include varieties such as plexiform, follicular, unicystic, basal cell, granulous cells, clear cells, acanthomatous, vascular and desmoplastic tumors9,7.
We report below two cases of ameloblastoma whose paranasal sinuses computed tomography scans were essential to determine the origin, extension and intervention of the cases, whereas pathology confirmed the diagnosis. We discuss clinical, radiological and surgical findings, as well as different treatment approaches for this kind of tumor.
CASE REPORT
Case 1
FMO, male 51-year-old patient, a Black farmer, came to Clínica Otorrinos, in Feira de Santana /BA, presenting nasal obstruction on the right for approximately one year, associated with persistent purulent rhinorrhea and ipsilateral headache.
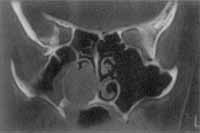
At ENT examination, we detected an irregular surface tumor, non-painful upon touch and non-bleeding, which occupied the whole right nasal cavity, filled with purulent secretion. There was also a slight bulging of the nasal dorsum on the same side. Paranasal sinuses CT scan showed an expansive lesion that occupied the whole maxillary sinus and right ethmoidal cells, with bone destruction of the lateral wall and ethmoidal trabecullae on the nasal cavity (Photos 1 and 2).
Photo 1. Computed Tomography - axial section (case 1).
Photo 2. Computed Tomography - coronal section (case 1).
The patient was submitted to previous biopsy of the lesion and later surgical intervention with degloving technique. Pathology showed formations of loose reticular cells, with small nuclei and scarce cytoplasm, surrounded by stratified cylindrical or pseudostratified epithelium. Nuclei of uniform volume with no areas of mitosis, arriving at the definite diagnosis of ameloblastoma (Photo 3).
Photo 3. Microscopic view (case 1).
Photo 4. Endoscopic view (case 2).
Case 2
DSS, female black 61-year-old patient, came to Clínica Otorrinos, in Feira de Santana/ BA, complaining of nasal bleeding on the right nasal fossa for approximately 3 months. She referred hypertension and use of propranolol and nifedipine. At ENT examination, we observed hard palate bulging on the right and presence of cystic tumor at the level of the inferior meatus on the same side (Photo 4). Paranasal sinuses x-ray showed mucosa edema on the right maxillary sinus. We ordered a facial CT scan and it showed that the mass occupied the right inferior meatus and projected into the hard palate on the same side (Photo 5).
We carried out surgical exeresis through post-labial incision. The tumor was adhered to the hard palate, destroying the bone by compression, followed by adherence to the mucosa of the right nasal fossa, which was partially resected, leaving the nasal wall semi-opened.
We applied nasal packing for 48 hours. Pathology classified the tumor as an acanthous ameloblatoma.
Six months after the surgery, the patient started to complain of bulging on the right jugal area. At physical examination, we observed a small tumor at the level of the right gum and oro-antral fistula on the same side. A new CT scan was made and we detected a recurrence of the tumor, which forced the hard palate on the right. We performed a resection through right hemimaxillectomy with Weber-Ferguson incision, followed by fitting of maxillary prosthesis.
One year after the second-surgery, the patient is still asymptomatic and with no signs of recurrences.
Discussion
It is generally accepted that 20% of ameloblastomas affect the maxilla, although some authors advocate that there is only 1% of the cases16 in this location.
Photo 5. Computed Tomography - coronal section (case 2).
Since maxillary ameloblastomas generally grow slowly and with no pain, because of lack of thick cortical layer, bone absorption and closeness to maxillary bone and nasal cavity, nasopharynx, paranasal sinuses, orbits and skull base, there is usually a delay in diagnosis, and invasion of these structures may serve as diagnostic evidence4. The most common symptom of maxillary ameloblastoma is non-painful bulging that involves part of the maxilla9. In our cases, the patients came to the Service of Otorhinolaryngology because they had nasal sinusal symptoms. The first patient's complaints were compatible with chronic sinusitis (nasal obstruction, purulent rhinorrhea for one year), and the second case initially had complaints of nasal bleeding. However, after the surgery for removal of cystic tumor masses on the right cavity, she experience recurrence of the tumor which was then manifested as an non-painful bulging on the homolateral jugal region.
Whereas some authors reported that ameloblastoma was more frequent in the 3rd and 4th decades of life and diagnosis was made in average after 5.8 years of evolution, in our two cases, patients were older (51 and 61 years), and diagnoses were made earlier, probably because they had nasal-sinusal symptomatology, which is not commonly found in these tumors.
In the two reported cases, the study of tumor extension and its relation with normal surrounding tissues was made through CT scan at coronal and axial sections. Similarly to Couto y Arcus and Gutierrez1, we believe that it is currently the preferred method to perform radiographic analysis of the function. In case 1, what attracted our attention was the fact that the lesion occupied the nasal cavity, the ethmoidal sinus and the maxillary sinus on the right, without compromising the lower bone wall, as we could expect from an ameloblastoma.
A number of therapeutic options have been proposed to treat ameloblastomas, such as wide excision, curettage, cryotherapy, cauterization, laser surgery, radiotherapy and chemotherapy18. Good results have been reported both with radical treatments and conservative methods, although enncleation and curettage have produced high rates of recurrence9. Thus, it seems that the best treatment method to ameloblastoma of maxillary bone is limited or wide excision of the tumor, with a 10-15mm-safety margin. In case 1, we chose a limited excision through the technique of degloving, since the lesion was confined to the nasal cavity and maxillary and ethmoidal sinuses. In Case 2, we initially chose a limited excision, but we were obliged to perform a hemimaxillectomy 12 months later, because of tumor recurrence. Both patients are currently asymptomatic, and the first one has been followed up for 2 years, whereas the 2nd one has one-year follow-up. According to Olaitan et al., about 80% of the recurrences take place within the 5 first years after the surgery, emphasizing the need to promote appropriate and intensive follow-up during this critical period11.
ACKNOWLEDGMENT
We would like to thank the Service of Pathology, Dr. Achiléa L. Bittencourt, at Hospital Martagão Gesteira, who has kindly provided the photos of the surgical piece slides.
REFERENCES
1. ADEKEYE, E.O. - Ameloblastoma of the jaws: a survey of 109 Nigerian patients. J. Oral Surg., 38:36-41, 1980.
2. ARCOS, F.C.; GUTIERREZ, A.O. L. - Diagnóstico radiológico del ameloblastoma. Rev. Mex. Radiol., 38:143-6, 1984.
3. BATSAKIS, J.G; HICKS, M. J.; FLAITZ, C.M. - Pathology consultation peripheral epithelial odontogenic tumors. Ann Otol. Rhinol. Laryngol., 102:322-4, 1993.
4. CRAWLEY, W.; LEVIN, L.S. - Treatment of the ameloblastoma. Cancer., 42:357-63, 1978.
5. GARDNER, A.F.; APTER M.B.; AXELROD, J.H. - A Study of Twenty-one instances of ameloblastoma, a turner of odontogenic origin. J. Oral Surg., 21:230-7, 1963.
6. HELTZANU, Y.; MENDELSOHN, D.B.; COREN, M.A. - Computed tomography of mandibular ameloblastoma. J. Comput. Assist. Tomogr, 8:220-3, 1984.
7. HUGHES, C.A.; WILSON, W.R.; OLDING, M. - Giant ameloblastoma: Report of an extreme case and description of its treatment. Ear Nose Throat J., 78.568-74, 1999.
8. IKEMURA, K.; TASHIRO, H.; FUJINO, H.; OHBU, D.; NAKAJIMA, K. - Ameloblastoma of the mandible with metastasis of the lungs and lymph nodes. Cancer, 29:930-40, 1974.
9. IORDANIDIS, S.; MAKOS, Ch.; DIMITRAKOPOULOS, J.; KARIKI, H. - Ameloblastoma of the maxilla. Case report. Austral. Lent. J., 44:51-5, 1999.
10. MINAMI, M.; KANEDA, T.; YAMAMOTO, H. et al - Ameloblastoma in the maxillomandibular region. MR imaging. Radiol., 184:389 93, 1992.
11.OLAITAN, A.A. ; AROLE, G.; ADEKEYE, E.O. -.Recurrent ameloblastoma of the jaws. A follow-up study. Int. J. OralMaxillofac Surg.;t 27.456-60, 1998.
12. PLASCENCIA, M.P.; MENDOZA, A.G.; SOSA, E.V. - Ameloblastoma del maxilar superior. Anales Soc. Mex. Otorrinolaringol., 30(1):19 22, 1985.
13. REDMAN, R.S.; KEEGAN, B.P.; SPECTOR, C. J.; PATTERSON, R.H. - Peripheral ameloblastoma with unusual mitotic activity and conflicting evidence regarding histogenesis. J. Oral Maxillofac. Surg., 52:192-7, 1994
14. ROBINSON, L.; MARTINEZ, M.G. - Unicystic ameloblastoma - a prognostically distinct entity. Cancer, 40:2278-85, 1977.
15. SAMPSON, D.E.; POGREL, M.A. - Management of mandibular ameloblastoma: the clinical basis for a treatment algorithm. J. Oral Maxillofac Surg., 57.1078-9, 1999.
16. SEABAUGH, J.L.; TEMPLER, J. W.; HAVEY, A.; GOODMAN, D. Ameloblastoma presenting as a nasopharyngeal tumor. Otolaryngol Head Neck Surg., 94:265-7, 1986.
17. SZEWKIS, D.; ASSAEL, A. - Ameloblastoma. Rev. Otorrinolaringol., 42:55-7, 1982.
18. UEDA, M.; KANEDA, T. - Combined chemotherapy and radiotherapy for advanced maxillary ameloblastoma. A case report. J. Craniomaxillofac Surg., 19:272-4, 1991.
1 Otorhinolaryngologist, Clínica Otorrinos.
2 Resident Physician in Otorhinolaryngology, Clínica Otorrinos.
3 Pathologist, Hospital Martagão Gesteira, Salvador /BA.
Study conducted at Clínica Otorrinos, Feira de Santana /BA
Study presented at 34° Congresso Brasileiro de Otorrinolaringologia, held on November 18 - 22, 1998, in Porto Alegre /RS.
Address correspondence to: Washington Luis de Cerqueira Almeida - Rua Barão de Cotegipe, 1141 - Centro - 44025-030 Feira de Santana /BA.
Tel: (55 75) 623-4455 - Fax: (55 75) 223-4117 - E-mail: otorrinos@gd.com.br
Article submitted on March 21, 2001. Article accepted on April 11, 2001.