Year: 2001 Vol. 67 Ed. 5 - (16º)
Artigos Originais
Pages: 707 to 714
Vocal reabilitation of patients with laringectomy using tracheoesofogeal proteses
Author(s):
Claudiney C. Costa 1,
Abrão Rapoport 2,
José Francisco S. Chagas 3,
Iara B. Oliveira 4,
Pedro de Castro 5,
Luiz Alberto Magna 6
Keywords: laryngectomy, voice rehabilitation, prosthesis
Abstract:
We studied the complications resulting from the placement and use of the vocal prosthesis, assessment of voice quality and speech intelligibility using perceptive-auditory parameters before and after speech therapy and the period needed for vocal rehabilitation. From February 1999 to June 2000, a study was conducted on 23 patients who underwent total laryngectomy and were given a tracheoesophageal prosthesis like the Blom-Singer Indwelling Low Pressure. Study design: Prospective clinical not randomized. Material and method: The study consisted of 22 males and their ages ranged from 40 years to 80 years. The follow up period varied between 150 days to 462 days. One patient with the posterior commissure affected was at stadium I; stadium II had one patient with a lesion in the subglottic region; stadium III had 13 patients; stadium IV had four patients. The prosthesis was placed in seven patients concomitantly with the laryngectomy, while the placement was secondary in the remaining group. Aim: We studied the complications resulting from the placement and use of the vocal prosthesis, assessment of voice quality and speech intelligibility using perceptive-auditory parameters before and after speech therapy and the period needed for vocal rehabilitation impossible. The success rating was 90% with 18 patients rehabilitated with the help of the prosthesis. The rehabilitation period varied between one day to 65 days. Conclusions: the complications resulted from placement and use of this prosthesis did not hamper its success; the average time taken for voice acquisition was seven days, vocal quality and intelligibility of speech showed improvement after the phonoterapy without significant statistics difference and the secondary placement through new surgical technique by digestive endoscopy is better than the conventional technique.
![]()
INTRODUCTION
Speech has a key role in human communication; in some occasions, due to adverse situations, the loss of speech makes men search for new alternatives to overcome the limitation. Laryngeal cancer is one of the main factors that cause loss of speech, threatening life and well being of people by interfering in the interpersonal relationships.
Laryngeal malignant tumors have a high incidence in Brazil and it is the sixth most common site of malignant tumors in males, amounting to 2,300 deaths recorded in 1996. According to the American Cancer Society, in 1999, 10,600 new cases of laryngeal and hypopharyngeal cancer were recorded in the United States, causing 4,200 deaths10.
The first total laryngectomy dates back to 1873, performed by Theodore Billroth and presented by his assistant Carl Gussenbauer at the Third Congress of Surgeons in Germany. It was named "The First Laryngectomy Performed in Humans by Theodore Billroth and the Use of Artificial Larynx". The first laryngectomy and vocal rehabilitation were created simultaneously8.
A new modality of rehabilitation for laryngectomees was developed by Singer and Blom, in 1980, through a prosthesis that allowed unidirectional passage of air driven by the lungs into the esophagus, putting into vibration the upper esophageal sphincter and the mucosa structures located above it to produce a voice of good quality, which required little time to learn19.
In Brazil, the use of tracheoesophageal prosthesis is not very common especially because of its high cost, lack of knowledge about surgical procedures and postoperative care, besides poor information about the advantages of a well indicated method3.
The purpose of the present study was to carry out vocal rehabilitation after total laryngectomy or pharyngobryngectomy with Blom-Singer tracheoesophageal prosthesis, considering: complications caused by placement and use of prosthesis, necessary time to acquire voice, perceptual-auditory analysis of vocal quality and speech intelligibility before and after speech therapy.
MATERIAL
We studied 23 patients submitted to total laryngectomy or pharyngolaryngectomy, with or without neck dissection and reconstruction of upper digestive tract with flaps, if necessary, because of laryngeal or hypopharyngeal cancer. Total laryngectomy was indicated in patients who presented aspiration pneumonia after hemiglossectomy and bucopharyngectomy. Patients were referred to the Service of Head and Neck Surgery at Hospital e Maternidade Celso Pierro, Pontifícia Universidade Católica de Campinas (HMCP/ PUC-CAMP) /SP. Vocally speaking, they were rehabilitated by placing the tracheoesophageal Blom-Singer Indwelling Low Pressure Voice Prosthesis, after explaining the advantages and disadvantages compared to other rehabilitation techniques. The patients were followed up by a team of speech therapists and physicians from the Service of Head and Neck Surgery at HMCP/PUC-CAMP, from February 1999 to June 2000, mean follow-up of 273 days, median of 230 days, ranging from 10 to 462 days, and 150 days was the minimum for a patient that had kept the prosthesis. The studied population comprised one female and 22 male patients.
As to age range, patients were divided into 4 groups of 10-year steps, and the youngest patient was 40 years old, whereas the oldest was 80 years, mean age of 57.6 years and median of 57 years.
Surgical procedures carried out in the groups were: total laryngectomy in 8 cases; total pharyngolaryngectomy with unilateral neck dissection in 6 cases; total pharyngolaryngectomy with bilateral neck dissection in 4 cases; total pharyngolaryngectomy with bilateral neck dissection and reconstruction of upper digestive tract, with rotation of isoperistaltic tube of the greater gastric curvature, in 3 cases; total pharyngolaryngectomy with bilateral neck dissection and reconstruction with rotation of myofascial flap of pectoralis major muscle in one case, and hemfglossectomy with unilateral neck dissection followed by a second surgical time of bucopharyngectomy, plus a third time of total laryngectomy, in one case. Ten patients were submitted to radiotherapy: six prior to placement of vocal prostheses and four, after it.
Among the 23 studied patients, 20 (87%) had advanced stages (III and IV); one (4.3%) had stage II, and one (4.3%) had stage I, according to the International Union Against Cancer, in 199711. The stage I patient presented primary lesion on the subglottic region, preventing a partial laryngectomy from being conducted.
METHOD
Methods for placement of prosthesis
For secondary placement of prosthesis, patients were hospitalized for 24 hours before the surgery and were discharged on the first postoperative day. For the secondary placement of prosthesis using the technique of upper digestive endoscopy, hospitalization was not necessary.
The patients from this study signed an informed Consent Term, approved by the Committee of Ethics on Research, at HMCP/PUC-CAMP, after being informed about prosthesis cost, other rehabilitation techniques (esophageal voice) and artificial larynx, and the advantages and disadvantages of tracheoesophageal prostheses.
In seven patients, we conducted primary placement, that is, together with laryngectomy or pharyngolaryngectomy. In 16 patients, placement took place after surgery, the so-called secondary placement.
Figure 1. Performance of tracheoesophageal fistula for primary placement of vocal prostheses.
Figure 2. Secondary placement of prosthesis using rigid esophagoscope; patient under general anesthesia.
For patients who received the prosthesis as secondary placement, we used the technique of upper digestive endoscopy in 11 cases. Placement of vocal prosthesis with rigid esophagoscope was conducted in 5 patients, and three of them had to be submitted later to upper digestive endoscopy for a new placement of prosthesis.
Primary placement was carried out under general anesthesia and after the removal of the larynx, with or without the associated procedure, according to the principles defined by Singer and Blom, in 198019 (Figure 1).
The secondary placement technique with rigid esophagoscope was also conducted under general anesthesia, followed by the classical technique proposed by Maves and Lingeman, in 198214 (Figure 2).
Secondary placement by upper digestive endoscopy was carried out with videogastroendoscope Fujinon Eve Series 400 and monitor Sony Triniton Color. Patients were sedated with 5mg intravenous midazolam and were discharged from the endoscopy room after recovering from the sedation caused by the drug (Figure 3).
Patients were instructed to clean the tracheoesophageal prosthesis with a solution of 3ml oral nistatin diluted in 10rril saline solution, instilled through the prosthesis lumen three times a day.
Speech therapy
Patients included in the present study were followed up by the speech therapists of the Service of Head and Neck Surgery at Hospital a Maternidade Celso Pierro, Pontifícia Universidade Católica de Campinas/SP, to exercise and evaluate vocal quality and speech intelligibility with the tracheoesophageal prosthesis through a perceptual-auditory analysis.
I - Procedure for data collection
We used a tape recorder brand Sanyo, with cassette tapes Basf CE II chrome extra and internal microphone placed 30cm from the patient's mouth. Patients were filmed with a JVC video camera.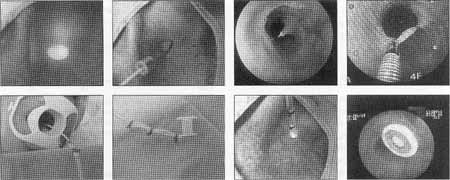
Figure 3. Placement of prosthesis by upper digestive endoscopy without the use of general anesthesia (sequence from left to right).
II - Vocal Training
There were four 30-minute sessions once a week to improve vocal production and articulation of patients. Sessions addressed the following aspects:
a) Respiration and articulation/digital coordinator for speech;
b) Exercises for respiration/articulation coordination;
c) Articulation and prosody exercises for connected speech;
d) Review of addressed aspects and recording of post-training speech sample.
III - Post-therapy assessment
Preparation of voice and speech samples for perceptual-auditory analysis.
In order to analyze speech before and after speech therapy, we used a method of perceptual-auditory analysis. Samples were analyzed by three speech therapists who scored the items as 3 (Good), 2 (Fair) and 1 (Poor).
Criteria for the analysis
Speech therapists used the protocol for vocal assessment in the 34 voice samples collected in the pre and post-therapy stages. The studied items were: Item I - Intonation and prosody - Subjects produced the same sentence with statement and question intonation and both forms were auditorily compared, based on three possibilities:
Good - clear distinction between statement and question.
Fair - inconsistent distinction between statement and question.
Poor - no distinction between the melodic curves of statement and question.
Item II - Analysis of speech intelligibility, considering the production of sentences:
Good- enough speech intelligibility.
Fair - moderate speech intelligibility.
Poor - difficult to understand intelligibility.
Item III - Analysis of spontaneous speech intelligibility (conversation):
Good - enough speech intelligibility in most situations.
Fair - understanding of part of the utterances, which did not compromise the general communication context.
Poor - compromise of most utterances.
Item IV - Analysis of melody in singing voice:
Good - singing with melody and rhythm close to normal.
Fair - singing with some variations of melody and rhythm.
Poor - singing in which melody and rhythm are not evident.
Quality of voice and speech were considered good if scores were between 10 and 12; fair, between 7 and 9, and poor, between 4 and 6. Therefore, for each items, subjects were scored for pre and post-therapy samples, which were compared to evaluate the efficacy of the speech therapy in patients rehabilitated with tracheoesophageal prosthesis.
Statistical method
Chi-square test was applied to study the statistical significance between the technique of prosthesis placement and vocal rehabilitation.
In the statistical analysis to determine significance of vocal quality levels, before and after speech therapy, we used chi-square test with two degrees of freedom.
The correlation between vocal quality after speech therapy and conduction of radiotherapy was studied with the application of Fisher's test.
RESULTS
In seven patients, vocal prostheses were placed at the same surgical time as laryngectomy, and among them, six developed speech within 5 to 65 days. The patient that took 65 days to use the prosthesis had a pharyngocutaneous fistula. He progressed to local tumor recurrence with loss of prosthesis use before speech therapy.
Secondary placement with rigid esophagoscope was used in 5 patients and two of them presented vocal production on the first and fourth day after the placement of the prostheses. One of the patients progressed with local cellulitis where the tracheoesophageal puncture had been made and resulted in partial extrusion of the prosthesis on the 6th postoperative day, which was replaced later with the technique of upper digestive endoscopy. In the other three patients, causes of failure were one episode of upper digestive hemorrhage at early postoperative period, with partial extrusion of the prosthesis, after passing of esophageal Singstalhen-Blacmore balloon, one case of bronchopneumonia with local infection on the tracheoesophageal puncture site, and one case of partial extrusion.
Placement of prosthesis through upper digestive endoscopy was carried out in 14 patients and among them, three had received a prosthesis by the secondary placement technique with rigid esophagoscope, with no success. Using the chi-square test, we found statistically significant difference when the prosthesis was placed by upper digestive endoscopy (Table 1).
The complications resulting from the surgical treatment for laryngeal and hypopharyngeal cancer were: five stenosis of tracheostome, three postoperative cutaneous fistulae, two tumor recurrence with loss of prosthesis, one pharyngoesophageal stenosis, one case of bronchopneumonia and CVA, leading to death.
Vocal quality of the 17 studied patients was evaluated before, and after speech therapy with statistically significant difference (Table 2).
In five patients, there was failure of vocal production with the tracheoesophageal prosthesis, and in only two cases the ending of the tracheoesophageal fistula was related to placement and use of the prosthesis. In three cases, closing of the fistula was a result of the therapeutic surgical procedure, represented by two cases of pharyngocutaneous fistulae with tumor recurrence and one death.
Twenty patients (90.9%) had advanced cancer (stages III and IV), according to UICC10, and all patients who did not manage to use the prosthesis for oral communication were stage IV cases. The remaining patient was submitted to laryngectomy because of repetitive aspiration pneumonia.Table 1. Relation between vocal rehabilitation and placement techniques of Blom Singer vocal prostheses in 23 patients.
p= 0.0236 x2=1.49 2 degrees of freedom
* Three of the patients were referred for placement with upper digestive endoscopy, amounting to 26 prostheses placed.
** EDA: upper digestive endoscopy
Table 2. Vocal quality related to speech therapy.
p= 0.1431 x2=3.89 2 degree of freedom
Table 3. Vocal quality related to radiotherapy.
p= 0.1534 Fisher's test
There was no statistically significant difference using Fischer's test for the correlation of vocal quality with tracheoesophageal fistula and radiotherapy (Table 3).
DISCUSSION
Total laryngectomy causes a serious impact on the lives of patients, leading to a sudden rupture of oral communication and interaction of the patient and other people, resulting in significant social, economic, family and psychological changes. Owing to that, vocal rehabilitation is very important to improve the quality of the laryngectomee. In recent years, a number of studies have demonstrated the efficacy of vocal rehabilitation with vocal prosthesis. Comparing with the rehabilitation rates for esophageal voice that range from 14 to 76%, success rates of vocal prosthesis exceed 80%4,9,15.
In pharynx and larynx stages III and IV tumors, although prognosis is severe, survival is frequently prolonged to justify an aggressive therapy to destroy the tumor and reconstruct the defects resultant from the intervention. Reconstruction should go beyond a simple tube that enables the passage of saliva, in order to allow vocal and swallowing rehabilitation as close to normal as the results of traditional laryngectomy with primary closure2.
Among our cases, 3 patients were submitted to total pharyngolaryngectomy with bilateral neck dissection and reconstruction of the upper digestive tract, after rotation of isoperistaltic greater gastric curvature.
In our study, closure of tracheoesophageal fistula was observed in 5 cases (21.7%), as follows: four stage IV cases, with pharyngocutaneous fistula and tumor recurrence in two cases (8.7%); upper digestive hemorrhage with partial extrusion of prosthesis in one case (4.4%); lack of motivation in one case (4.4%), and death caused by vascular cerebral accident and pulmonary causes in one patient (4.4%). These complications were noticed in patients who had been submitted to large procedures, requiring reconstruction of digestive tract through the rotation of the isoperistaltic tube of the greater gastric curvature and myocutaneous flap of pectoralis major muscle.
Speech rehabilitation failure due to lack of motivation was observed in one patient (4.4%) who was illiterate, lived in the rural area and had his life restricted to the family nucleus. The failure rate of vocal rehabilitation because of lack of motivation ranges from 6.9 to 9.2%6,17.
In only two patients the reasons for failure of vocal rehabilitation were related to the vocal prosthesis: lack of motivation and upper digestive hemorrhage with partial extrusion of prosthesis. In the other three patients, vocal rehabilitation did not succeed because of factors rather than the prosthesis, leading to a rehabilitation rate of 90% of the patients, that is to say, 18 out of 20 possible patients, compatible with the data provided by other authors6,9,14,19.
Complications found in the patients from this study related to the vocal prosthesis or its placement, were: three cases of valvular insufficiency of the prosthesis, two infections in the tracheoesophageal puncture site with partial extrusion, one granuloma around the prosthesis, two prosthesis colonized by fungi, one digestive hemorrhage with partial extrusion of the prosthesis, one case of bronchopneumonia with partial extrusion, a complete extrusion of the prosthesis. Similar complications were described by other authors5,6,7,12,13,17,18.
In our sample, complications with the use of the tracheoesophageal prosthesis were found normally in the first 6 months of follow-up, and out of the total of 23 patients, only six happened after this period. They were represented by leakage through the prostheses in three cases, fungi colonization in two patients and complete extrusion of prosthesis in one patient. All complications were related to wear of prosthesis and the solution found was to replace it for a new prosthesis.
Singer and Blom20 found an incidence of pharyngoesophageal spasm of 12% in their patients caused by narrowing of pharyngoesophageal lumen during the closure of the constrictive musculature of the pharynx. Maves and Lingeman14 recommended closure only of the mucosa and submucosa of the pharynx during laryngectomy in order to reduce the incidence of pharyngoesophageal stenosis. In the studied patients, there was no modification in the pharyngeal closure standardized by our service, which is conducted in two planes, mucosa and muscles, without myotomy of pharyngeal constrictors. Since we had only one patient with narrowing of pharyngoesophageal segment, there was no technical correlation between closure of pharynx and the incidence of the narrowing.
The importance of speech therapy in patients with vocal prosthesis was studied by Mendelsohn et al.16, who observed that during the occlusion of the tracheostome, there was contraction of the cervical muscles by extending or flexing the head and that the patient could experience pull force or increase of pressure in the vibration segment, affecting the flow and the tension of the air in the segment, compromising the final result of vocal quality. During the four speech therapy sessions, patients were instructed to improve the coordination of respiration, articulation and digital occlusion of the tracheostome (respiration/ articulation digital coordination), melody, intonation and reduction of cervical muscle tension.
As to vocal quality, when we compared our patients with and without radiotherapy, we did not find statistically significant differences. Silverman and Black18, studied vocal quality, in the 1st, 3rd, 6th, and 12th month after placement of Blom-Singer tracheoesophageal prosthesis in patients with and without radiotherapy and they observed that vocal quality produced with the prosthesis was worse in the first three months after radiotherapy, with no statistically significant difference in the 6th month post-radiotherapy. According to the authors, one of the parameters used for the indication of tracheoesophageal prosthesis use is age of the patients, that it, below 65 years. This criterion was not followed in our study and of the 17 patients submitted to therapy, 7 were older than 67 years and among them, 5 were aged between 72 and 80 years.
Duration of vocal rehabilitation after primary placement varied from 5 to 65 days, mean of 25 days. Maves and Lingeman14 presented a study in which they evaluated the time from the beginning of vocal rehabilitation, at primary placement, and they obtained intervals that ranged from 14 to 84 years after surgery, mean of 36.4 days. In the secondary placement carried out by us, rehabilitation started between the 1st and the 2nd days.
Placement through upper digestive endoscopy was performed in 14 patients and they were all rehabilitated on the first day, which seems to be the most efficient method. The short time between placement of prosthesis and vocal rehabilitation is an important factor for the motivation of patients and family members, facilitating the follow-up by the physician and the speech therapist. Similarly to Blom, Singer and Hamaker1, we believe that the main purpose of vocal rehabilitation is the restoration of the patient's social and economic status as close to presurgery as possible.
Vocal quality was considered poor in five patients after speech therapy and four of them had not been submitted to radiotherapy. Factors that seemed to have negatively interfered in vocal quality were advanced age of patient (76 years old), surgery for lip tumor resection in one patient, which affected speech articulation, difficulty to occlude the tracheostome in one patient, and stenosis of pharyngoesophageal segment in another.
In, this group of patients, we observed that the advantages of having vocal rehabilitation with tracheoesophageal prostheses were: non-compromise of oncological principles, since we did not modify the surgical technique necessary for the radical oncological treatment; compatibility with patients submitted or not to radiotherapy; success rate greater than 80%; short time needed for learning; use of the lungs as source of air for phonation, increasing maximum phonation time and producing longer sentences, closer to those produced by laryngeal voice; vocal volume louder than the one .obtained with other rehabilitation approaches2,4,9,15,19. As to disadvantages, we noticed: cost of the prosthesis, need to be followed up by a surgeon to maintain and replace the prosthesis, need to use the hands to occlude the tracheostome.
The surgeon who is willing to perform an aggressive procedure such as laryngectomy should be prepared to provide all the possible vocal rehabilitation alternatives, instructing in a simple acid direct way the advantages and disadvantages of each one, for the patients to make the decisions.
CONCLUSION
For patients with Blom-Singer prosthesis:
1. There is no compromise of oncological principles;
2. Compatible with patients submitted or not to radiotherapy;
3. Success rates greater than 80%;
4. Use of the lungs as source of air;
5. Complications resultant from placement and use of prosthesis do not compromise the success of the method;
6. The mean time it took to acquire voice was 7 days;
7. Vocal quality and speech intelligibility improved after speech therapy, with no statistically significant difference;
8. Placement of vocal prosthesis through upper digestive endoscopy, dispensing general anesthesia and patient's hospitalization, proved to be effective compared to traditional methods.
REFERENCES
1. BLOM, E.D.; SINGER, M.I.; HAMAKER, R.C. - A prospective study of tracheoesophageal speech. Arch. Otolaryngol. Head Neck Surg., 112:440-7, 1986.
2. BLOM, E.D. - Evolution of Tracheoesophageal Voice Prostheses In:______- Tracheoesophageal Voice Restoration Following Total Laryngectomy. 1.ed. San Diego, Singular Publishing Group, 1 8, 1998.
3. CECCON, F.P. - Contribuição ao estudo da voz alaringea: analise acústica, temporal a perceptiva da voz traqueoesofágica. São Paulo, 1997. (Tese - Mestrado - Apresentada a Universidade Federal de São Paulo Escola Paulista de Medicina, para obtenção do Titulo de Mestre em Otorrinolaringologia).
4. DELSUPEHE, K.; ZINK, L; LEJAEGERE, M.; DELAERE, P. - Prospective randomized comparative study of tracheoesophageal voice prosthesis: Blom-Singer versus Provox. Laryngoscope, 108:1561-5, 1998.
5. FUKUTAKE, T. & YAMASHITA, T. - Speech rehabilitation and complications of primary tracheoesophageal puncture. Acta Otolaryngol. 500:117-20, 1993.
6. GARTH, R.J.N.; McRAE,A.; EVANS, R. - Tracheo-oesophageal puncture: a review of problems and complications. J. Laryngol. Otol., 105:750 4, 1991.
7. GLUCKMAN, J.L., SILVER, F.M.; DONEGAN, J.O. - Operative complications of tracheoesophageal puncture. Laryngoscope, 95:1360 2, 1985.
8. GUSSENBAUER, C. - Über die erste durch Theod. von Billroth am Menschen Ausgefuhrte Kehlkopfextirpation. Arch. Klin. Chir, 17343, 1874.
9. HILGERS, F.J.M.; SCHOUWENBURG, P.F. - A new low-resistance, selfretaining prosthesis (Provox TM) for voice rehabilitation after total laryngectomy. Laryngoscope, 100:1202-7, 1990.
10. INCA; MINISTÉRIO DA SAÚDE; GOVERNO FEDERAL. - Estimativa da incidência a mortalidade por câncer no Brasil 2000. Rio de Janeiro, 2000.
11. INTERNATIONAL UNION AGAINST CANCER. - TNM classification of malignant tumors. New York, 5a. ed. Sobin & Ch. Wittekind, 1997.
12. LABRUNA, A.; HUO, J.; KLATSKY, L; WEISS, M.H. - Tracheoesophageal puncture in irradiated patients. Ann. Otol. Rhinol. Laryngol., 104:279 81, 1995.
13. LACCOURREYE, O.; MÉNARD, M.; CREVIER-BUCHMAN, L.; COULOIGNER, V.; BRASNU, D. - In situ lifetime, causes for replacement, and complications of the ProvoxTM voice prosthesis. Laryngoscope, 107: 527-30, 1997.
14. MAVES, M.D. & LINGEMAN, R.E. - Primary vocal rehabilitation using the Blom-Singer and Panje voice prostheses. Ann. Otol. Rhinol. Laryngol., 91:458-60, 1982.
15. MAX, L.; STEURS, W.; BRUYN, W. - Vocal capacities in esophageal and tracheoesophageal speakers. Laryngoscope, 106: 93-6, 1996.
16. MENDELSOHN, M.; MORRIS, M.; GALLAGHER, R. - A comparative study of speech. After total laryngectomy and total laryngopharyngectomy. Arch. Otolaryngol. Head Neck Surg., 119:508-10, 1993.
17. OLIAS, J.; MAGALHAES, M.; MONTALVAO, P.; ZAGALO, C.; FERREIRA, L.; ESCUDEIRO, C.; GONÇALVES, F.; SANTIAGO, N. - Implantes fonatórios - Revisão de 101 casos. Rev. Port. Otorrinol., 34:21-9, 1996.
18. SILVERMAN, A.H. & BLACK, M J. - Efficacy of primary tracheoesophageal puncture in laryngectomy rehabilitation. J. Otolaryngol., 23:370-8, 1994.
19. SINGER, M.I. & BLOM, E.D. - New endoscopic technique for restoration of voice after laryngectomy. Ann. Otol., 89:529-33, 1980.
20. SINGER, M.I. & BLOM, E.D. Selective myotomy for voice restoration after total laryngectomy. Arch. Otolaryngol., 107.670-3, 1981.
1 Surgeon, Head and Neck Surgery, Hospital a Maternidade Celso Pietro, Pontifícia Universidade Católica de Campinas. Master in Head and Neck Surgery, Complexo Hospitalar Heliópolis /SP.
2 Coordinator of the Post-Graduation Course on Head and Neck Surgery, Complexo Hospital Heliópolis /SP.
3 Head of the Service of Head and Neck Surgery, Hospital a Maternidade Celso Pietro, Pontíficia Universidade Católica de Campinas.
4 Speech Pathologist, Pontifícia Universidade Católica de Campinas.
5 Endoscopist, Endoscopy Service, Hospital a Maternidade Celso Pietro, Pontifícia Universidade Católica de Campinas.
6 Faculty Professor, Department of Medical Sciences - UNICAMP (Statistical analysis of the study). Affiliation: Head and Neck Surgery, Hospital a Matemidade Celso Pietro da PUC de Campinas and Complexo Hospitalar Heliópolis /SP.
Address correspondence to: Claudiney Candido Costa - Rua Antônio Rodrigues Moreira Nero, 106, Apt°. 11 - Jardim Paulicéia - 13060-063 Campinas /SP
Tel: (55 19) 227-5377 E-mail: claudineyorl@bestway.com.br
Master dissertation submitted to the Post-Graduation Course at Complexo Hospitalar Heliópolis de São Paulo/SP, on October 25, 2000.
Article submitted on April 18, 2001. Article accepted on Tune 18, 2001.