Year: 2002 Vol. 68 Ed. 5 - (2º)
Artigo Original
Pages: 615 to 618
Histological analysis of 24 pharyngeal tonsils from pacients submitted to adenoidectomy or adenoamigdalectomy
Author(s):
Adriana L. Alves 1,
Wanessa A. R. Scala 2,
Mirna D. Barros 3,
José E. L. Dolci 4
Keywords: pharyngeal tonsils, epithelium, histology
Abstract:
Introduction: The epithelium of pharyngeal tonsil is described mostly as a pseudostratified columnar ciliated epithelium with globet cells. Study design: Experimental. Objective: Description of the types of overlay epithelium of pharyngeal tonsils and the frequency of occurrence of these diferent types. Material and Method: Histological study of twenty-four pharyngeal tonsils from children three to seven years old to adenoidectomy or adenoamigdalectomy inthe Departament of Otorrinolaringology, Irmandade da Santa Casa de São Paulo. Results: Only 4,15% of the tonsils presented the pseudostratified columnar ciliated epithelium with globet cells like covering epithelium of exclusive occurrence; 4,15% presented exclusively stratified squamous nonkeratinized epithelium; 41,70% of all observeded tonsils showed predominance of pseudostratified columnar ciliated epithelium with globet cells with some areas of stratified squamous nonkeratinized epithelium; 50% of the observed sampleshowed predominance of stratified squamous nonkeratinized epithelium with some areas of pseudostratified columnar ciliated epithelium with globet cells. Conclusion: The studied pharyngeal tonsils presented the stratified squamous nonkeratinized epithelium with areas of pseudostratified columnar ciliated epithelium with globet cells as the most frequent epithelium of linining.
![]()
INTRODUCTION
Tonsils are incomplete encapsulated aggregates of lymphoid nodules, placed below and in contact with the epithelium of the initial portions of the digestive and respiratory tracts. According to the location, they can be named palatine, lingual or pharyngeal tonsils. Since they are placed in the way of aspirated or ingested antigens, they have an important role in immune response1.
Palatine tonsils are bilateral and located at the limit of the oral cavity and the oropharynx. The deepest area of each palatine tonsil is recovered by stratified non-keratinized pavement epithelium forming from 10 to 20 deep crypts that invaginate into the parenchyma, which consists of numerous lymphoid nucleus being that many of them have germination centers. The presence of centers indicates the formation of B lymphocytes2.
On the posterior-superior wall of the nasopharynx, we can identify a saliency also formed by lymphoid tissue, the pharyngeal tonsil (pharyngeal tonsil of Luschka). Especially during the first and second years of life, the pharyngeal tonsil can be hypertrophied in a considerable mass (adenoid hypertrophy), reaching the maximum size at the age of 4 to 7 years and starting its regression at the age of 12 to 13 years. On top of the pharyngeal tonsil, at the midline, there may be an irregular depression of mucosa, extending superiorly up to the basilar process of the occipital bone2.
From a histology perspective, pharyngeal tonsils are similar to palatine tonsils, but the capsule is incomplete and thinner. There are no crypts, but shallow longitudinal folds. The ducts of serous-mucous glands open to the base of these folds. The most superior surface of the pharyngeal tonsil is recovered by ciliated pseudostratified columnar epithelium, mixed with pavement stratified epithelium. The parenchyma consists of lymphoid nodules with occasional germination centers3.
As to the function of the pharyngeal tonsil epithelium, it is believed to have an affinity with the IgA producing cells and a secretory component that would be present only in this epithelium, and not in the palatine tonsil epithelium4.
Lingual tonsils, situated at the tongue base, are similar to the palatine tonsils, but they are not involved by a capsule3.
Palatine tonsils are formed from the second pair of pharyngeal pouches. Endoderm of the second pouch forms the epithelium that recovers the tonsils and the crypts. After week 20, the mesenchyma around the crypts is differentiated into lymphoid tissue, which is organized in lymphatic nodules of the tonsil5. Pharyngeal tonsils, in turn, are originated from an aggregate of lymph nodes on the wall of the nasopharynx 6.
In the literature, the recovering epithelium of the pharyngeal tonsil is described as the respiratory epithelium, that is, pseudostratified ciliated columnar with goblet cells1, 3.
The purpose of the present study was to conduct a morphological analysis of the recovering epithelium and the frequency of occurrence in the pharyngeal tonsils, removed from patients submitted to adenoidectomy and adenotonsillectomy.
MATERIAL AND METHOD
We analyzed the pharyngeal tonsils of 24 patients aged 3 to 7 years, submitted to adenoidectomy and adenotonsillectomy, at the Department of Otorhinolaryngology, Santa Casa de São Paulo, between August 2000 and May 2001. Of the total, there were 10 female and 14 male children.
The exeresis of pharyngeal tonsils was conducted by adenoidectomy with Beckman curette. Tonsils, right after removal, were placed in non-sterile vials with formol at 10%, being then sent for analysis at the Department of Morphology, Medical School, Santa Casa de São Paulo.
Pharyngeal tonsils were fixed in formol at 10% for 24 hours. After dehydration they were placed in paraffin, and we conducted serial sections that were 5mm thick. The deparaffined sections were stained with hematoxylin-eosin (HE) (Behmer et al., 1996)7 and observed under optical microscopy.
RESULTS
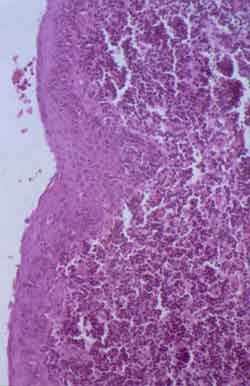
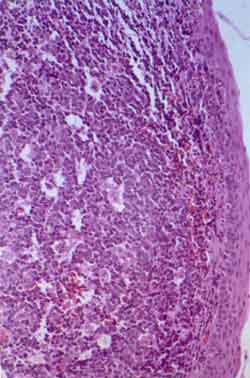
We observed two types of recovery epithelium in the studied pharyngeal tonsils: pseudostratified ciliated columnar with goblet cells (Figure 1a) and non-keratinized stratified pavement epithelium (Figure 1b).
Figure 1a. Histology sections of pharyngeal tonsil recovered by pseudostratified ciliated columnar with goblet cells - HE. 200 times magnification.
Figure 1b. Histology sections of pharyngeal tonsil recovered by non-keratinized stratified pavement epithelium - HE. 200 times magnification.
These types of epithelium were described in four groups presented in Table 1.
Both group A (pseudostratified ciliated columnar with goblet cells, exclusively) and group B (non-keratinized stratified pavement epithelium, exclusively) were present at similar percentages (4.15%). The main percentage was found (50%) for group D (predominance of non-keratinized stratified pavement epithelium) followed by the occurrence of group C (predominance of pseudostratified ciliated columnar with goblet cells) (41.7%) (Graph 1).
Graph 1. Percentage of different groups of pharyngeal tonsils concerning type of recovering epithelium.
Table 1. Different groups of pharyngeal tonsils concerning type and occurrence of recovering epithelium.
DISCUSSION
The data collected in the present study were not in accordance with the description in the literature about the pharyngeal tonsil epithelium, showing predominance of non-keratinized stratified pavement epithelium, differently from the expected pseudostratified ciliated columnar.
As to collection of the analyzed pharyngeal tonsils, we should bear in mind that patients submitted to adenoidectomy and adenotonsillectomy present clinical pictures that resulted in surgical indication, suffering from the action of factors such as repetitive infectious processes and other aggressions over the tonsil tissue, which may lead to abnormalities of the epithelium such as metaplasia.
The possibility of having aggressive factors triggering epithelial metaplasia has already been described for the epithelium of nasal turbinates8 and palatine tonsils4. The repetitive inflammation results in epithelium metaplasia of palatine tonsil crypts 4.
The nasal epithelium considered normal, that is, pseudostratified ciliated columnar with goblet cells, rarely remains normal owing to multiple aggressions, such as extreme temperature, infectious processes, different types of pollutants and traumas. These aggressions can take to reduced cilia where there is air impact, in addition to increasing the number of goblet cells and inflammatory cells. Squamous metaplasia found in these cases has its beginning in childhood and progresses, being a normal phenomenon as a protective response to external influence8.
Abnormalities of the nasal mucosa resulting from viral infections present more destruction of the cilia than abnormalities found in the cases of allergic rhinitis 8. In addition, the continuous air inhalation could lead to abnormal nasal epithelium, from pseudostratified ciliated columnar with goblet cells to cuboidal and later to stratified pavement8.
Inspiration nasal airflow, that is, the air that is not conditioned, is described as the probable determining factor in metaplastic abnormalities of the nasal respiratory epithelium, being that there is a direct correlation of age, pollution, infections and/or other aggressive factors and frequency and grades of metaplasia 9.
The nasal epithelium tends to be more respiratory in the posterior region of the nasal fossa 9. Therefore, the inspiration airflow would not be considered a causing factor of metaplasia found in the epithelium of the pharyngeal tonsil, since it would be in more of a posterior position than the nasal turbinates and, consequently, less exposed to airflow aggressions.
Thus, we can infer the importance of infections also in abnormalities of the pharyngeal tonsil epithelium of patients submitted to adenoidectomy.
It is important to point out how difficult it is to find studies in the literature that analyze the pharyngeal tonsil epithelium in a more comprehensive manner, showing the differences found in the daily practice concerning the classical description of the epithelium. It is even more difficult to find studies of the probable causes to justify the variation of epithelium found in the data presented in our study.
Future histology studies of pharyngeal tonsils of newborn patients with no infectious history or stillborn babies, which in addition to not having infectious impairment, do not have influence of the airflow passage over the pharyngeal tonsil epithelium, will be able to explain which original recovering epithelium is the most frequent one, the occurrence of metaplasia and the possible factors involved in the process.
CONCLUSION
Non-keratinized stratified pavement epithelium with areas of pseudostratified ciliated columnar with goblet cells is the epithelium most frequently detected in the analyzed pharyngeal tonsils, differently from the data reported in the literature.
REFERENCES
1. Gartner LP, Hiatt JL. Tratado de histologia em cores. 1ª ed., Rio de Janeiro: Guanabara Koogan S. A.; 1999. p. 234.
2. Lopes Filho O, Campos CH. Tratado de otorrinolaringologia. 1ª ed. São Paulo: Editora Roca; 1994.
3. Junqueira LC, Carneiro J. Histologia básica. 9ª ed. Rio de Janeiro: Guanabara Koogan S.A.; 1999. p. 242-243.
4. Freitas LPS. Análise de estudos sobre histologia e ultra-estrutura do epitélio da cripta tonsilar. São Paulo, 1997; p. 14. (Dissertação apresentada ao curso de pós-graduação da Faculdade de Ciências Médicas da Santa Casa de São Paulo para obtenção do título de mestre em Medicina).
5. Langman J. Embriologia médica. 3ª ed. São Paulo: Livraria Atheneu Editora; 1996. p. 231.
6. Moore KL. Embriologia clínica. 4ª ed. Rio de Janeiro: Guanabara Koogan S.A; 1996. p. 259.
7. Behmer OA, Tolosa EMC, Freitas AG de Neto. Manual de técnicas para histologia normal e patológica. São Paulo: EDART; 1976. p.239.
8. Dolci JEL. Modelo estrutural e ultra-estrutural do epitélio da mucosa da concha nasal inferior de pacientes portadores de rinite alérgica. São Paulo, 1994; p. 5-35 (Tese apresentada à Escola Paulista de Medicina para obtenção do título de doutor em Medicina).
9. Lopes Filho O, Bussoloti Filho I. Anatomofisiologia clínica e cirúrgica do nariz e cavidades paranasais. 1a ed. São Paulo: Fundo Editorial BYK; 1998. p. 19.
1 Post-graduation under course, Department of Otorhinolaryngology, Santa Casa de Misericórdia de São Paulo (I.S.C.M.S.P.).
2 Resident Physician, Department of Otorhinolaryngology, I.S.C.M.S.P.
3 Joint Professor, Department of Morphology, Medical School, Santa Casa de São Paulo (F.C.M.S.C.S.P.).
4 Assistant Professor, Department of Otorhinolaryngology, I.S.C.M.S.P.
Affiliation: Department of Otorhinolaryngology, I.S.C.M.S.P. and Department of Morphology, F.C.M.S.C.S.P.
Address correspondence to: Adriana L. Alves - Rua João Clímaco Pereira, 46 São Paulo SP 04532-070
Tel/Fax: (55 11) 3849.0543 - E-mail: adrialves@yahoo.com
Study presented at II Congresso Triológico de ORL, held in Goiânia/GO, in August 2001.
Article submitted on July 01, 2002. Article accepted on August 1, 2002