Year: 2013 Vol. 79 Ed. 1 - (17º)
Artigo Original
Pages: 100 to 105
A comparison of the Fujita classification of awake and drug-induced sleep endoscopy patients
Author(s):
Fabio Augusto Winckler Rabelo1; Daniel Salgado Küpper2; Heidi Haueisen Sander3; Vanier dos Santos Júnior4; Eric Thuler4; Regina Maria França Fernandes5; Fabiana Cardoso Pereira Valera6
DOI: 10.5935/1808-8694.20130017
Keywords: apnea; endoscopy; propofol; sleep apnea, obstructive; sleep apnea syndromes.
Abstract:
Only a few studies have compared the outcomes of patients kept awake during endoscopic examination and subjects submitted to drug-induced sleep endoscopy.
OBJECTIVE: This study aimed to compare the endoscopic findings of patients submitted to outpatient endoscopy and endoscopic examination with sedation by propofol based on the Fujita Classification.
METHOD: This cross-sectional cohort study enrolled 34 patients. The subjects underwent ENT examination, nasal endoscopy with Müler's maneuver, and drug-induced sleep endoscopy with propofol. The Fujita Classification was used to compare the two modes of endoscopic examination. The examinations were correlated to patient clinical data such as BMI, age, and OSAS severity.
RESULTS: There was no agreement between the two modes of endoscopic examination, whether for the group in general or for the analyzed subgroups.
CONCLUSION: There was no agreement between the endoscopic findings of endoscopic examinations done with the patient awake or in drug-induced sleep.
![]()
INTRODUCTION
The studies performed on obstructive sleep apnea syndrome (OSAS) have enhanced the understanding of symptoms, facilitated diagnosis, and demonstrated the effectiveness of positive airway pressure therapies1. Nonetheless, the difficulties inherent to complying with this mode of treatment have called the attention to other therapeutic possibilities - surgery in particular1.
The vast array of approaches and the scarce controlled randomized trials hinder the demonstration of surgery effectiveness. Reviews and meta-analyses aimed at assessing OSAS surgery have presented inconsistent results: Sher et al.2 and Sundaram et al.3 published meta-analyses on OSAS therapies and found inconsistent results for surgical treatments. Yet, the authors reported that the failure to observe all obstructed sites in the pharynx was the main reason for surgery unsatisfactory results, and that the determination of the site of obstruction should be the main focus of OSAS studies, given its strong correlation with treatment success. In 2010, the American Academy of Sleep Medicine published a review4 on various surgical treatments for OSAS and the authors concluded that future studies should focus on the standardization of preoperative evaluation and better patient selection.
In these three important reviews, the authors inferred that the main cause for surgery failure is inaccurate identification of the site of obstruction in the upper airway and, consequently, poor patient selection. The complexity of the upper airways and the multifactorial character of sleep apnea explain the difficulties related to this assessment. The following tests are currently available to aid in patient evaluation: cephalometric measurements, computerized tomography, magnetic resonance imaging, airway manometry, fiberoptic laryngoscopy using Müller's maneuver, and drug-induced sleep endoscopy (DISE).
DISE with propofol has been increasingly used, and is currently considered as the endoscopic examination mode that more closely resembles natural sleep and allows for better location of the site of obstruction in the upper airways. Recent studies have ranked highly the effectiveness of this examination in terms of accurately locating sites of obstruction5,6, outcome reproducibility7,8, and patient outcome9,10. Our group recently published a paper11 on the polysomnographic alterations introduced by propofol-induced sleep, adding to the reliability of this mode of examination.
However, only a few studies have compared the outcomes of patients kept awake during endoscopic examination and subjects submitted to drug-induced sleep endoscopy. This study is essential in the assessment of whether endoscopic examination under sedation is required.
This study aimed to compare the endoscopic findings of patients submitted to outpatient endoscopy and endoscopic examination with sedation by propofol based on the Fujita Classification.
METHOD
This is a multicentric study, with the following participating hospitals: University Hospital of the Medical School of Ribeirão Preto - University of São Paulo and the Samaritan Hospital between July of 2006 and January of 2010. All the enrolled patients were educated as to the nature of the study and signed an Informed Consent Form. The research protocol was assessed and approved by the hospital's Ethics Committee in Research with Humans (# 5620/2006).
The sample was made up of patients with a history of snoring and diurnal hypersomnia previously submitted to diagnostic nocturnal polysomnography at the hospital's Sleep Lab using a digital polygraph (Bio- Logic®) equipped with analytical software program Sleepscan Vision Analysis version 2.03.05. The following were recorded: electroencephalogram (F3-M2, F4-M1, C3-M2, C4-M1, O1-M2, O2-M1 as per the 10-20 International System), bilateral electrooculograms (E1-M2, E2-M1), electrocardiogram (modified V2), surface EMG of the mental and submental muscle, bilateral EMG of the anterior tibial muscle, synchronized digital video (infrared camera - Elbex IncTM), and body position (Netlink body sensor positionTM). Breathing was monitored as follows: a pressure transducer cannula recorded the flow of air through the nose (Ac Sleep 119, Biolink Medical Br®) in combination with a nasal and oral thermal air flow sensor (Pro-Tech thermal air flow sensorTM); respiratory inductance plethysmography belts were used to measure respiratory effort (Pro-Tech zRIP respiratory inductance plethysmographyTM); an oximeter (Netlink Head BoxTM) was used to assess blood oxygen saturation (O2 Sat) and a laryngeal microphone to record respiratory noises. All technical parameters were in accordance with the 2007 Manual of the AASM.
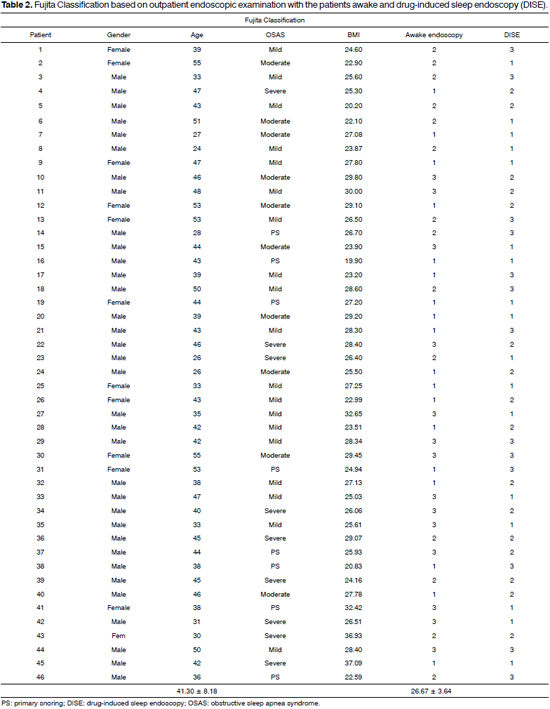
The study enrolled patients with sleep respiratory disorders willing to undergo the tests described below. Thirty-four males (73%) and 12 females (27%) with a mean age of 41.35 ± 7.96 years and a mean BMI of 26.82 ± 3.62 were included. Based on polysomnographic testing, eight patients (17.4%) snored but did not have apnea, 19 (41.3%) had mild OSAS, 10 (21.7%) had moderate OSAS, and nine (19.6%) had severe OSAS.
The exclusion criteria were: age under 18 and above 60 years and patients with cardiorespiratory comorbidities that increased the risk of sedation: previous AMI, congestive heart failure (CHF), severe chronic obstructive pulmonary disease (COPD), etc.
The Fujita Classification was described in 1987 by Fujita and Simmons, and has since been widely utilized in the topographic description of upper airway obstruction. Type I includes isolated oropharyngeal obstruction (and the palatal region); type II features obstruction of the oropharynx and hypopharynx; and type III describes isolated hypopharynx obstruction.
As a routine, during admission patients are submitted to physical and ENT examination, undergo awake fiberoptic laryngoscopy, and are assigned Mallampati and Friedman scores. Radiological examination data (cephalometric measurements, CT and MRI scans) were compiled from the patients' charts. Patients were kept in a seated position during fiberoptic laryngoscopy; the fiberscope was inserted in the nasal cavity after the application of topical vasoconstrictors. Two regions were assessed: nasopharynx/oropharynx and hypopharynx, at rest and with the patient in Müller's maneuver. At this time, the patients were staged based on the Fujita Classification12.
Anesthesia induction with propofol during DISE was carried out by an anesthesiologist. Cardiorespiratory parameters were monitored throughout the examination, and materials for intubation, airway access, and emergency medication were available in the operating room.
Propofol was intravenously administered with the aid of a target controlled infusion pump (Diprifusor® TCI, AstraZeneca) as described in the literature11. The estimated mean concentration of propofol on the effector site was 2.34 ± 0.6 mcg/ml.
All DISE procedures were carried out by the same ENT, who used 3.4 mm fiberscopes made by Olympus® or Scad®. The following parameters were described for each individual during the examination: velopharyngeal vibration, anteroposterior narrowing of the velopharyngeal lumen, circumferential narrowing of the velopharyngeal lumen, laterolateral narrowing of the oropharyngeal lumen, narrowing of the hypopharynx on the base of the tongue, laterolateral narrowing of the hypopharynx, and narrowing of the hypopharynx on the epiglottis. The patients were then staged based on the Fujita Classification. Obstructions greater than 50% of each level were considered positive.
All the tests described above (polysomnography, awake endoscopic examination, and DISE) were carried out within 90 days.
Weighted Kappa was used to compare the Fujita Classification subject scores on awake endoscopy and DISE and determine the level of agreement between the scores in both circumstances. The impact parameters such as BMI, age, and OSAS severity had upon the level of agreement between the examinations was assessed through ANOVA, Fisher's exact test, and weighted Kappa.
RESULTS
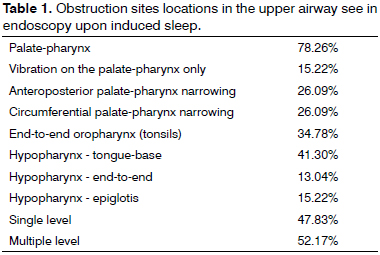
Findings on velopharyngeal vibration and/or upper airway narrowing during DISE are described on Table 1. Velopharyngeal involvement was seen in 78.26% of the cases, oropharyngeal narrowing in 34.78% of the subjects, and hypopharyngeal narrowing in 54.34% of the subjects. One-level obstruction were seen in 47.83% of the patients, whereas 52.17% of them had multiple levels involved (Table 1).
The Fujita Classification, based on clinical assessment and DISE, is shown on Table 2. Agreement in the given classifications was observed only in 14 individuals (30.43%).
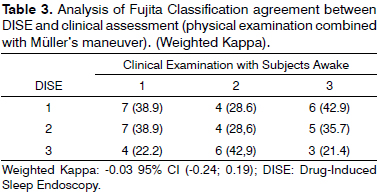
Table 3 shows the statistical analysis used to assess the level of agreement between the classifications given during both endoscopic examinations. A level of -0.03 was verified, i.e., there was no agreement between the two examinations performed on the same patients. When the groups were subdivided for clinical parameters, the Kappa value was still low (0.01 for patients above 45 years of age; -0.01 for patients under 45; -0.25 for patients with a BMI under 25; 0.08 for patients with a BMI above 25; -0.10 for patients with mild OSAS; 0.10 for patients with moderate or severe OSAS). Therefore, clinical parameters had no impact upon the disagreement seen between the two endoscopic examinations.
DISCUSSION
Consensus states that the better and more accurate the characterization of the site of obstruction in patients with sleep-disordered breathing (SDB), the better the therapy and its results. The reviews cited in this paper have shown that outpatient endoscopy is not enough to properly stratify patients, as indicated by the inconsistent success rates reported for the analyzed surgical procedures2. With this in mind, our group carried out a study to assess the success rates of uvulopalatopharyngoplasty (UPPP) based on clinical, outpatient endoscopic, and polysomnographic criteria, only to observe that 28 (44%) of the 64 patients enrolled in the study recovered completely13. This finding reinforces the fact that the approach currently in place -based on outpatient endoscopic criteria and the Friedman Classification - does not adequately select the ideal candidates for palatal surgery.
Drug-induced sleep endoscopy (DISE) has been considered by a number of recent studies as the examination that more closely resembles natural sleep, in addition to enabling dynamic, three-dimensional evaluation of the upper airways as the subject snores or suffers from episodes of apnea7,8. According to these authors, the detailed description of the sites of upper airway obstruction allowed by DISE has facilitated the choice of therapy and led to the wider use of this endoscopic examination in OSAS care centers. Two classification models have been proposed to rate DISE findings: the VOTE8 and the NOHL14 scales. These schemes enable the observation of collapses in traditionally uninvolved structures in outpatient endoscopic examination, as is the case of collapsed epiglottis seen in 15.22% of our cases. Thus, comparisons by the exact site of obstruction between awake endoscopy and DISE are inherently flawed. This is why we opted to use a simpler and more basic classification system to make this comparison based on the topographic level of obstruction (Fujita Classification).
There was no agreement in the Fujita Classification assigned to patients in awake and sleep-induced endoscopy (Kappa = -0.03). This disagreement may have occurred due to the lack of consideration given to specific conditions and characteristics of sleep, neuromuscular alterations, respiratory and postural patterns in deciding upon a therapy.
Our findings are similar to those reported by Campanini et al.15. After assessing 250 patients, these authors found similar classifications in only 25% of the cases, with greater disagreements in obstructions of the hypopharynx. The authors also stressed that in 33% of the cases the examination allowed the observation of relevant laryngeal obstructions that were missed in the examination done with the subjects awake. Gregorio et al.16 reported that more retrolingual collapses were seen with DISE than with Müller's maneuver in a group of eight patients, and concluded that outpatient assessment alone may lead to underdiagnosis.
Another important finding as we analyze patients with agreeing or disagreeing Fujita Classifications and compare them for BMI, age, or OSAS severity, is that there is no clinical criteria to support the use of DISE. The lack of a correlation or pattern of obstruction reinforces the idea that each patient must be analyzed in an individualized fashion.
The lack of agreement between the examinations proves that there is a marked neuromuscular component in the obstruction of the airways of subjects in their sleep, and that we are probably underestimating these findings when we base ourselves only on the endoscopic findings of awake patients.
More studies are required to confirm the importance of DISE in the assessment of OSAS patients. However, this study has confirmed that the same endoscopic examination, when performed at different times, may yield conflicting results.
CONCLUSION
The assessment derived from drug-induced sleep endoscopy differs from the evaluation produced from the endoscopic examination of awake subjects.
REFERENCES
1. Kakkar RK, Berry RB. Positive airway pressure treatment for obstructive sleep apnea. Chest. 2007;32(3):1057-72.
2. Sher AE, Schechtman KB, Piccirillo JF. The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep. 1996;19(2):156-77.
3. Sundaram S, Bridgman SA, Lim J, Lasserson TJ. Surgery for obstructive sleep apnoea. Cochrane Database Syst Rev. 2005;19(4):CD001004.
4. Caples SM, Rowley JA, Prinsell JR, Pallanch JF, Elamin MB, Katz SG, et al. Surgical modifications of the upper airway for obstructive sleep apnea in adults: a systematic review and meta-analysis. Sleep. 2010;33(10):1396-407.
5. Kotecha BT, Hannan SA, Khalil HM, Georgalas C, Bailey P. Sleep nasoendoscopy: a 10-year retrospective audit study. Eur Arch Otorhinolaryngol. 2007;264(11):1361-7.
6. Bachar G, Feinmesser R, Shpitzer T, Yaniv E, Nageris B, Eidelman L. Laryngeal and hypopharyngeal obstruction in sleep disordered breathing patients, evaluated by sleep endoscopy. Eur Arch Otorhinolaryngol. 2008;265(11):1397-402.
7. Rodriguez-Bruno K, Goldberg AN, McCulloch CE, Kezirian EJ. Test-retest reliability of drug-induced sleep endoscopy. Otolaryngol Head Neck Surg. 2009;140(5):646-51.
8. Kezirian EJ, White DP, Malhotra A, Ma W, McCulloch CE, Goldberg AN. Interrater reliability of drug-induced sleep endoscopy. Arch Otolaryngol Head Neck Surg. 2010;136(4):393-7.
9. Camilleri AE, Ramamurthy L, Jones PH. Sleep nasoendoscopy: what benefit to the management of snorers? J Laryngol Otol. 1995;109(12):1163-5.
10. Hessel NS, de Vries N. Results of uvulopalatopharyngoplasty after diagnostic workup with polysomnography and sleep endoscopy: a report of 136 snoring patients. Eur Arch Otorhinolaryngol. 2003;260(2):91-5.
11. Rabelo FA, Braga A, Küpper DS, De Oliveira JA. Lopes FM, de Lima Mattos PL, et al. Propofol-induced sleep: polysomnographic evaluation of patients with obstructive sleep apnea and controls. Otolaryngol Head Neck Surg. 2010;142(2):218-24.
12. Fujita S. Pharyngeal surgery for obstructive sleep apnea and snoring. In: Fairbanks DNF, Fujita S. Ikematsu T, Simmons FB, editors. Snoring and obstructive sleep apnea. New York: Raven Press; 1987. p.101-28.
13. Braga A, Carboni LH, do Lago T, Küpper DS, Eckeli A, Valera FC. Is uvulopalatipharyngoplasty still an option for the treatment of obstructive sleep apnea? Eur Arch Otorhinolaryngol. 2012. [Epub Ahead of Print].
14. Vicini C, De Vito A, Benazzo M, Frassineti S, Campanini A, Frasconi P, et al. The nose oropharynx hypopharynx and larynx (NOHL) classification: a new system of diagnostic standardized examination for OSAHS patients. Eur Arch Otorhinolaryngol. 2012;269(4):1297-300.
15. Campanini A, Canzi P, De Vito A, Dallan I, Montevecchi F, Vicini C. Awake versus sleep endoscopy: personal experience in 250 OSAHS patients. Acta Otorhinolaryngol Ital. 2010;30(2):73-7.
16. Gregório MG, Jacomelli M, Figueiredo AC, Cahali MB, Pedreira Jr WL, Lorenzi Filho G. Evaluation of airway obstruction by nasopharyngoscopy: comparison of the Müller maneuver versus induced sleep. Braz J Otorhinolaryngol. 2007;73(5):618-22.
1. PhD in ENT by FMRP-USP (MD, ENT).
2. MSc in ENT by FMRP-USP (Assistant Physician in the ENT Service of HC-FMRP-USP).
3. PhD in Neurology by FMRP-USP (Assistant Physician in the Neurology Service of HC-FMRP-USP).
4. MD, ENT (MD, ENT).
5. PhD in Neurology by FMRP-USP (Professor of Neurology at FMRP - USP).
6. Post-doctoral degree holder (Professor at FMRP - USP).
Medical School of Ribeirão Preto - University of São Paulo.
Send correspondence to:
Fabiana Cardoso Pereira Valera
Faculdade de Medicina de Ribeirão Preto - Universidade de São Paulo
Av. Bandeirantes, nº 3900, 12º andar
Ribeirão Preto - SP. Brazil. CEP: 14049-900
Tel: (16) 36022862. Fax: (16) 36022860
E-mai: facpvalera@fmrp.usp.br
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on July 24, 2012.
Accepted on November 4, 2012. cod. 9473.
Funding provided by FAPESP (process 2008/03771-0).