Year: 2012 Vol. 78 Ed. 1 - (23º)
Relato de Caso
Pages: 141 to 141
Catheterization of Stenon's duct for surgical excision of oral fibroepithelial hyperplasia
Author(s): Deygles Cristiane Barbosa1; Rui Medeiros Júnior2; Elaine Judite Amorim Carvalho3; Alessandra Albuquerque Tavares de Carvalho4
DOI: 111/1111111.20120033
Keywords: hyperplasia, mouth mucosa, salivary ducts.
![]()
INTRODUCTION
Hyperplasias are the most frequent exophytic lesions in the mouth, which develop mainly as a consequence of mucosal tissue irritation by several types of trauma. Injured tissues respond with proliferation of fibroblasts followed by collagen fibrinogenesis1.
Fibroepithelial hyperplasia (FH) is the most common non-malignant soft tissue tumor in the mouth; its prevalence is similar in both sexes and there is no racial preference2. Its usual site is the jugal mucosa along the occlusion line; it presents as a well-defined smooth pink sessile or pediculated nodule. These tumors are usually asymptomatic except when injured secondarily3.
The treatment is surgical excision and elimination of local irritative factors. The purpose of this study was to describe a surgical technique for removing oral FH and preserving Stenon's duct.
CASE REPORT
A male patient aged 36 years presented with an enlarged mass in the right jugal mucosa. The tumor had developed over about 13 years; it was painless at first, but the patient had started to feel pain when applying pressure over the nodule or during chewing.
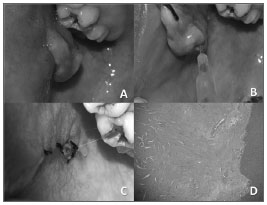
Examination of the mouth showed a hyperplasic pediculated fibrous pinkish smooth surfaced tumor measuring about 2.0 x 1.8 cm, located on the right jugal mucosa close to the exit site of Stenon's duct (Fig. 1A). Because of its close anatomical relation with the parotid duct, surgical removal would have to preserve this structure.
Figure 1. A) Clinical image of the tumor, showing its site next to the parotid duct exit point. B) Site of Stenon's duct - Jelco number 20. C) Final aspect after removal of the tumor; note the anterior portion of the Jelco in the exit point of the duct. D) Microscopy of the tumor showing fibroblasts dispersed within a collagen matrix and lined by squamous epithelium.
The treatment consisted of catheterizing the parotid duct with a Jelco number 20 catheter (Fig. 1B), followed by an elliptic incision of the tissue, dissection, removal of the tumor, and simple closure (Fig. 1C).
Histology revealed dense fibrous connective tissue with fusiform fibroblasts dispersed within a mature collagen matrix. There were many congested vascular spaces and mild chronic inflammation. The tumor was lined with hyperplasic epithelial squamous tissue (Fig. 1D).
The catheter was kept in place for seven days to activate salivary drainage; there were no postoperative complications or recurrences in the first year of follow-up.
DISCUSSION
Lewkowicz at al.4 also reported catheterizing Stenon's duct when repairing trauma in the parotid region; these authors used a pediatric intravenous catheter, which makes it possible to locate where the duct courses and thereby avoid injury to the duct.
Parotid duct injury may result in sialoceles, cutaneous fistulae, or salivary duct cysts. The most common causes of duct injury are trauma by cutting, pointed, and blunt objects, as well as surgical trauma5.
Several treatment approaches have been described in the literature; the choice depends on the duration of injury, the site of the gland, the mechanism of trauma, and the surgeon's experience. Ideally parotid duct injury should be treated as soon as possible; in some cases (significant loss of tissues or polytraumatized patients) a delayed procedure may be done intentionally6.
Conservative approaches are repeated percutaneous needle aspiration, compressive dressings, and antisialagogue medication. A few authors also recommend parenteral nutrition to reduce autonomous salivary stimulation of the parotid7.
A more aggressive approach is needed if these measures are unsuccessful. These maneuvers include placing tubes in the site to create a new salivary duct path, radiotherapy, partial or total parotidectomy, tympanic neurectomy, and others8.
In the present case, after the duct was located and the tumor was removed, the anterior portion of the Jelco catheter was left in place during a week to facilitate salivary drainage and to avoid the sublingual caruncule closure and duct stenosis during the healing process.
The treatment for FH is surgery, taking care to remove the entire tumor and to avoid irritative factors to prevent recurrence9.
FINAL COMMENTS
FH is one of the most common tumors in the mouth; it deserves attention when treated, as an adequate surgical technique is essential to avoid recurrences. Adjacent anatomical structures should be preserved as much as possible to avoid injury and future complications.
REFERENCES
1. Silverman S, Eversole LR, Truelove EL. Tumefaçăo e tumores da cavidade oral e da face. Em: Silverman S, Eversole LR, Truelove EL. Fundamentos de medicina oral. 2ed. Rio de Janeiro: Editora Guanabara; 2004. p.226-242.
2. Ceballos A. Tumores benignos de la mucosa oral. In: Bagán JV, Ceballos A, Bermejo A, Aguirre JM, Peńarrocha M, eds. Medicina Oral. Barcelona: Masson; 1995. p. 177-185.
3. Anneroth G, Sigurdson A. Hyperplastic lesions of the gingiva and alveolar mucosa: a study of 175 cases. Acta Odontol Scand. 1983;41:75-86.
4. Lewkowicz AA, Hasson O, Nahlieli O. Traumatic injuries to the parotid gland and duct. J Oral Maxillofac Surg. 2002;60:676-80.
5. Neuhaus RW, Baylis HI. Parotid duct injury as a complication of differential seventh nerve ablation. Am J Ophthalmol. 1982;93(1):124-5.
6. Steinberg MJ, Herréra AF. Management of parotid duct injuries. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:136-41.
7. Haller JR. Trauma to the salivary glands. Otolaryngol Clin North Am. 1999;32(5):907-18.
8. Vargas H, Galati LT, Parnes SM. A pilot study evaluating treatment of postparotidectomy sialoceles with botulinum toxin type A. Arch Otolaryngol Head Neck Surg. 2000;126:421-4.
9. Hemenway WG, Bergstrom L. Parotid duct fistula: a review. South Med J. 1971;64(8):912-8.
1. Specialist. Dental surgeon.
2. Specialist in oral and maxillofacial surgery and traumatology. Oral and maxillofacial surgeon.
3. Doctoral degree in oral pathology. Assistant professor of oral pathology, UFPE.
4. Doctoral degree in stomatology. Assistant professor of stomatology, UFPE.
Pernambuco Federal University (Universidade Federal de Pernambuco or UFPE).
Send correspondence to:
Deygles Cristiane Barbosa
Rua Estevăo de Sá, 782; Várzea
CEP: 50740-270. Recife - PE
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on May 14, 2010.
Accepted on August 16, 2010. cod. 7089
All rights reserved - 1933 /
2026
© - Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico Facial