Year: 2011 Vol. 77 Ed. 6 - (3º)
Artigo Original
Pages: 691 to 699
Dizziness in community-dewelling older adults: a population-based study
Author(s): Suzana Albuquerque de Moraes1; Wuber Jefferson de Souza Soares2; Rosilene Andrade Silva Rodrigues3; Waléria Christiane Rezende Fett4; Eduardo Ferriolli5;Monica Rodrigues Perracini6
Keywords: aged, dizziness, health of the elderly, vertigo.
Abstract:
Dizziness is a common complaint among older adults. Aim: To identify the prevalence of dizziness and its related factors in a sample of community-dwelling older adults. Methods: A prospective population-based study with a representative sample of older adults aged 65 years and over. A multidimensional questionnaire and a battery of measures were used for assessing physical function. Results: The prevalence of dizziness was 45%. Vertigo was found in 70.4% of older adults with dizziness and 43.8% of them referred vertigo crises along life. A significant association was found between dizziness and female gender (p=0.004), memory difficulties complaints (p=0.015), bad health perception (p=0.001), depression (p<0.0001), five or more comorbidities (p=0.021), self-reported fatigue (p<0.0001), recurrent falls (p=0.001), excessive sleepiness (p=0.003), fear of falling (p<0.0001), left leg unipedal stance (p=0.002) and Short Performance Physical Battery score (p=0.009). Conclusion: Dizziness is a common complaint among older adults and it is associated with limiting clinical conditions, such as depression, fatigue, excessive sleepiness and impaired memory. It is highlighted the association between dizziness and recurrent falls, fear of falling and lower performance in physical function tests, which can restrict independence. These data suggest the importance of a multifactorial approach to dizziness in older adults.
![]()
INTRODUCTION
Dizziness is a frequent complaint in the elderly population, and its prevalence increases significantly with age1-5. Recent population studies have reported a prevalence ranging from 11.0% to 32.5%6-8. A longitudinal study of elderly patients aged 65 years and over found that the prevalence of dizziness within the past six months among subjects aged 70 years was 27%, and that among patients aged 90 years or more it was 54%4. The incidence was 83.3 per 1,000 inhabitants among elderly patients monitored in primary care; it was 67.8 per 1,000 inhabitants among elderly patients aged from 65 to 74 years, and increased to 108.4 per 1,000 inhabitants among patients aged 85 years or more9. The prevalence of dizziness is higher is women than men (the male/female incidence in one year is 1:2.7)2. Dizziness and vertigo are associated with an increased risk of falls and loss of function, which may results in a substantial loss of independence and worse quality of life in this population group1,10-12.
The rate of falls within the past year in elderly patients with vestibular disease is significantly higher - about 50% - compared to the reported rate in community-dwelling elderly patients (about 30%)13. Falls within the past three months were reported by 31% of elderly subjects with dizziness compared to 15% in elderly subjects not complaining of dizziness5. The risk of falls is increased in adults and elderly persons with vestibular dysfunction1. The chance of falling was about three times higher among subjects with dizziness compared to those without this complaint in a two-year follow-up of community-dwelling elderly subjects (OR - 3.24; CI - 95%, 2.11-4.99)4. Dizziness and vertigo are risk factors for falls and severe injury such as fractures14,15. Vestibular dysfunction limits postural control, leading to instability and misaligned posture; this explains why dizziness may be a predisposing factor for falls16.
Elderly individuals with vestibular dysfunction may find it difficult to perform activities of daily life that require rapid head movements17. Dizziness can make it difficult for patients with vestibular dysfunction to carry out activities of daily life even while symptoms regress18. Among elderly patients with chronic vestibular dysfunction, 49% reported difficulties in carrying out seven of more activities, 26% in one to three activities, and 19% in four to six activities; only 7% said that they could carry out activities of daily life without any difficulties. The activities that discriminated elderly individuals with more limitations were walking close to home, taking a shower, and shopping, which require coordinated head and eye movements and demand more of the vestibular system12.
There is an association between chronic dizziness and symptoms of depression, self-reported poor health, and restriction in social activities19,20. About 56% of elderly patients with vestibular diseases and 42% of elderly individuals with complaints of dizziness score positively for symptoms of depression5,21. Associated factors are female gender, memory and concentration disorders, insomnia, hypoacusis, and poor vision21. Dizziness in elderly subjects is also associated with lack of physical activity and poor emotional and physical quality of life. There is a strong association between depression and poor quality of life in elderly individuals with dizziness; there is evidence in the literature that neuro-otologic dysfunction is related with anxiety and psychological problems, which in turn may increase the intensity of dizziness5.
Dizziness has been characterized as a geriatric symptom, a multifactor condition resulting from the cumulative effect of losses in several systems, which increase the vulnerability of elderly individuals10. A few medical conditions have been associated with dizziness, such as anxiety, depression, impaired hearing, using five or more medications, postural hypotension, disordered body balance, and a history of acute myocardial infarction10. A two-year longitudinal follow-up study revealed that the main predictors of dizziness as a complaint in elderly individuals were: age, female gender, cardiovascular disease, osteoporosis, depression, disordered sleep, memory disorders, poor vision, urinary incontinence, three or more co-morbidities, use of four or more medications, poor perception of health, falls, and mobility issues4. Several sensations associated with dizziness as a complaint have been reported in the literature, such as loss of balance (64.5%), near syncope (11.4%), turning around (41%), and its manifestation as single or multiple conditions daily or weekly in 68% of cases4,20.
Because the elderly population has increased, it has been estimated that the number of elderly individuals with dizziness and vertigo has also increased. Identifying the profile of elderly patients with dizziness as a complaint will help plan specific interventions for this age group. The purpose of this study was to investigate the prevalence of dizziness as a complaint and its associated factors in a population of community-dwelling elderly individuals, and to characterize dizziness in terms of its course, duration, sensation of falling, unbalance, periodicity, intensity, associated symptoms, and triggering functional activities and movements.
MATERIAL AND METHODS
An exploratory cross-sectional epidemiological study was carried out as a sub-project of the Study Network on the Frailty of Brazilian Elderly Individuals (Rede de Estudos de Fragilidade de Idosos Brasileiros or Rede FIBRA - FIBRA network), which is a multicenter multidisciplinary population based network that aims to study the features and prevalence of the biological frailty syndrome according to Fried et al.'s22 proposed phenotype. It encompasses 17 Brazilian sites selected by quota sampling based on human development indices.
The sample comprised 391 elderly subjects of both sexes aged 65 years or more that resided in the city of Cuiaba, MT, who were assessed from March 2009 to March 2010.
The exclusion criteria consisted of Ferrucci et al's23 recommendations: 1) presence of memory, attention, spatial and time orientation, and communication deficits suggesting severe cognitive disorders as assessed by the Mini-Mental State test24-26 according to the following scores25 - 17 for illiterates, 22 for elderly subjects with 1 to 4 years schooling, 23 for elderly subjects with 5 to 8 years schooling, and 26 for subjects with more than 9 years schooling, less a standard deviation; 2) permanent or temporary inability to walk - walking sticks or walkers are allowed, but not wheelchairs; 3) localized loss of strength and aphasia because of a stroke; 4) severe loss of movement, speech, or affect associated with severe or unstable Parkinson's disease; 5) severe hearing loss and visual deficits that make it difficult to communicate; 6) terminal stage patients.
Fifteen census regions were visited in Cuiaba - 513 elderly individuals were enrolled. Twenty-eight subjects were excluded based on the exclusion criteria. Ninety-four individuals quit after the questionnaires were applied.
Figure 1 (below) shows the study sample flowchart.
Figure 1. Study sample flowchart.
Subjects were informed about the purpose and procedures of the study and signed a free informed consent form. The approval protocol number of the institutional review board of the Ribeirão Preto Clinic Hospital was 5018/2007.
Elderly subjects were evaluated in two steps, as follows: the first consisted of a semi-structured interview - common to all participating centers of the FIBRA network - carried out by trained interviewers in a 40 to 120 minute session at the subject's household; the second step consisted of a data-gathering session by trained personnel on the physical and functional status, lasting 20 to 30 minutes, comprising a battery of ten standard function tests and anthropometric data, carried out in public schools, community centers, and city health centers close to the households of subjects.
The following variables were included: age, gender, whether living alone, education level, self-reported diseases (heart conditions, arterial hypertension, stroke, diabetes, depression), obesity27, number of diseases and medications, hospital stays within the past year, subjective perception of vision and hearing, smoking, memory and sleep disorders, functional performance as assessed by Lawton's instrumental activities of daily living (IADL)28 and advanced activities of daily living (AADL)29, self-efficacy for falls (Falls Efficacy Scale International or FESI)30,31, symptoms of depression as assessed by the Geriatric Depression Scale (GDS-15)32,33, self-reported fatigue (Center for Epidemiological Studies Depression Scale or CES-D)34, a subjective perception of health, and the extended inquiry about falls, sleepiness (Epworth sleepiness scale)35, and dizziness.
Dizziness was investigated based on a self-reported presence of this symptom within the past year; the question was: "Did you feel dizziness in the past year?" Elderly subjects were asked to think of dizziness as any sensation of rotating, gyrating, feeling emptiness or weight in the head, dizziness itself, and fluctuation. The question for vertigo was: "When you feel dizziness, do you feel your body or head going round, or what is around you going round?"
The question for characterizing dizziness was: progression time, duration, presence of falling sensation, unbalance or instability while walking, periodicity, presence of dizziness in 14 situations and/or activities: standing from decubitus, turning the head, turning the body from a sitting or standing position, standing from a sitting position, walking, while anxious, head in specific positions, sitting still, changing position on the bed, while exercising, laying on a side, when nervous, after eating, not having breakfast, and associated symptoms (tinnitus, headache, memory and concentration deficits, hypersensitivity to sounds, nausea, vomiting, sweating, anxiety, feeling imminent syncope, pressure, fear, insomnia, oscillopsy, or hearing loss).
The physical-functional tests were: timed up and go test36,37, five step test38, right and left one-leg balance time39, short physical performance battery (SPPB)40-43, and habitual gait velocity.
A descriptive analysis comprised simple frequency and central tendency measures, with a 95% confidence interval. The Kolmorogov-Smirnov test was applied to check compliance with a normal distribution. The chi-square test or Fisher's exact test for categorical variables and the "t" test or the Mann-Whitney test for quantitative variables were applied to compare the groups with or without a complaint of dizziness; the significance level was α<0.05. The SPSS® version 13.0 for Windows software was used for the statistics.
RESULTS
The prevalence of dizziness was 45.0% (N=176). Of these, 31.7% reported dizziness within the past two months. Rotating dizziness was reported by 70.4% of elderly subjects; 43.8% of subjects reported past vertigo crises at some point in their lives.
The mean age of elderly subjects with dizziness was 72.26 ± 5.97 years; it was 72.55 ± 6.16 years in subjects not reporting dizziness. This difference was not statistically significant (p=0.686). About 70% of subjects complaining of dizziness were aged from 65 to 74 years.
Women were 71.6% of the sample with dizziness; men were 28.4% (p=0.002). Elderly subjects with a complaint of dizziness had a higher rate of more than five co-morbidities compared to those not complaining of dizziness (60.9% vs 39.1%); they also scored positively in depression screening (62.7% vs 37.3%), excessive sleepiness (60.5% vs 39.5%), fatigue (60.8% vs 39.2%), poorer perception of health (53.3% vs 46.7%), memory disorders (51.6% vs 48.4%), and recurrent falls within the past year (64.1% vs 35.9%) (Table 1).
Most elderly subjects (68.7%) reported dizziness progressing for more than one year; of these 24.4% reported a complaint of dizziness for more than 5 years. Dizziness was constant in 2.8% of subjects; it lasted several days in 4.5% of subjects. It lasted less than one minute in 54.0% of subjects, and from one minute to two hours in 30.7% of the sample.
About 70% of subjects with dizziness reported a falling sensation, and half reported unbalance or instability while walking.
Dizziness was sporadic in 71.6% of subjects, monthly in 11.4% of subjects, and daily in 13.1% of subjects.
The dizziness intensity score on a visual analog scale was less than 5 points in 51.8% of the sample; the score was above 5 points in 18.7% of the sample. The intensity score was equal to or higher than 7 in 13.6% of subjects.
Half of the elderly subjects with dizziness said that standing from a lying position was the initiating cause of dizziness; 48.3% reported turning the head as the triggering factor, and 38.1% mentioned standing from a sitting position. The most frequent associated symptoms was tinnitus (18.7%), followed by sweating, pallor and tachycardia (16.6%), feeling anxiety (16.4%), a sensation of blocked ear (15.6%), and headache (14.8%). Table 2 shows the feature of dizziness relative to the positions, triggering activities and associated symptoms.
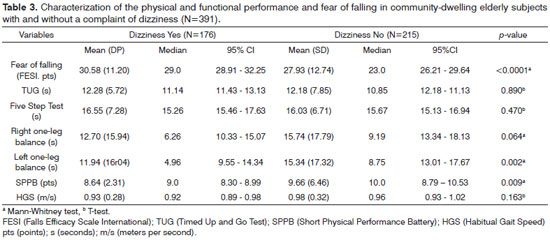
Table 3 shows gait and movement-related physical and functional performance tests, and fear of falling in elderly subjects with and without a complaint of dizziness. Subjects with dizziness, compared to those that do not complain of dizziness, have a poorer sensation of self-efficacy to avoid falls (p<0.001), are more concerned about the possibility of falls, lower left one-leg balance time (p=0.002), and poorer lower limb functional performance (p=0.009) as assessed in the SPPB.
DISCUSSION
In this study, the prevalence of dizziness as a complaint within the last year was 45%; 70.4% of these reported rotating dizziness. Most published studies have reported a prevalence around 30%6,10,44. Gasmman & Rupprecht4 reported 29.2% in a longitudinal cohort study of 620 elderly individuals aged 65 years or more. Tamber et al.45 reported a prevalence of 36.2% at age 75 years in a cross-sectional cohort study of 3,352 elderly subjects (the Oslo Health Study), which was similar to Gopinath et al.'s46 findings in a study of 2,751 subjects aged 50 years and above in the Blue Mountains Hearing Study. Cabral et al.47 evaluated dizziness as a complaint in elderly individuals that were monitored at a primary care center and found that the prevalence was 47%. Only one study reported a low prevalence (11.1%); an explanation was the question posed to participants: "With what frequency do you have dizziness when walking over a flat surface?" - this restricts other sensations and activities related to dizziness. Dizziness is an important symptom among the elderly. The term, however, is considered non-specific because it describes a wide range of sensations, such as feeling the head empty, fluctuation, stunning, dizziness, and others. There is no consensus on the definition of dizziness for population and epidemiological studies4,45. It is considered a wide range of sensations related to bodily orientation in space. Vertigo is considered a subtype of dizziness; it is defined as an illusion of movement, commonly a rotating sensation10,46. Dizziness as a complaint is approached from several angles in questionnaires - face to face interviews, mail, or telephone4,6,10,44-46. Questions routinely used in published studies are: "Do you have any problem such as vertigo, dizziness, poor balance, or instability in general?44 "Have you experienced any sensation of dizziness or instability within the past year?"46 "Have you had dizziness within the past six months?"4 "Below is a list of issues. Have you experienced any of them within the past week?" (one of the 10 issues was dizziness)46; "Within the past two months have you felt giddy, unstable, or as if you were rotating or moving, with your head empty, or fainting?"10 Interviewers in the present study were trained to ask about dizziness in more detail by describing to the interviewees several sensations which could be characterized as dizziness; the goal was to avoid sub-reports due to lack of knowledge or information. We also believe that face to face interviews may have helped the elderly subjects to clarify their sensations and to define whether they were in the category of dizziness.
The most common functional activities or movements associated with dizziness were (Hurvitz, 2000 #93): standing from a lying position, turning the head, and standing from a sitting position. The first two were also the most frequent in Tinetti et al.'s10 study. Standing from a lying position and walking were more frequent in Gassmann & Rupprecht's4 study. A study that assessed elderly patients with vestibular diseases found that turning the head and keeping the head in a specific position were the most common movements or positions associated with dizziness20.
The complaint of dizziness was more common in females compared to males (50.6% vs. 35.2%), which is supported by several studies4,9,10,13,20,21,46,48. Some studies suggest a correlation between age and dizziness, with a higher prevalence in older age groups4,9. Other, as in the present study, found no independent association between age and a complaint of dizziness8,10. Stevens et al.8 found no significant age difference in elderly patients with and without dizziness in the English Longitudinal Study of Aging (ELSA); there was an independent relationship between age and disordered body balance.
As expected, there was a significant association between number of diseases and dizziness. Although a nonspecific symptom in some cases, dizziness is largely related to vestibular system dysfunction, which is often multifactorial in the elderly.4 Subjects reporting dizziness or vertigo in a study involving of 2,751 subjects to clarify the etiology of dizziness revealed that 27.7% were of vestibular origin, 39.3% of non-vestibular origin, and 33.0% were inconclusive46. A Dutch study found that 39% of elderly subjects aged 65 or older who sought their family physicians because of dizziness were diagnosed as having dizziness of unknown causes - after examinations, tests and consultation with specialists. In several other studies, the prevalence of dizziness was higher in elderly patients that presented more co-morbidities9,10,45.
The most relevant clinical findings were depression, excessive sleepiness, exhaustion fatigue, memory disorders, and recurring falls. Depression has been associated with dizziness in several papers4,8,10. Tinetti et al.10 found that elderly individuals with more symptoms of depression in the CES-D tool had 1.36 times more chances of presenting dizziness (95% CI; 1.02-1.80) compared to those with fewer symptoms. Similarly, Gassmann & Rupprecht4 indicated a 3.89 higher chance (95% CI; 2.07-7.30), and Stevens et al.8 found a 2.17 times higher chance (95% CI; 1.56-3.01). The relationship between depression, symptoms of depression, and the effects of antidepressant use is complex. The complaint of fatigue was measured in this study by asking the following questions taken from the CES-D tool ("Did you feel you had to make an effort to deal with habitual tasks?"and "Have you left aside many of your interests and activities?"). Also, reports of memory disorders and excessive sleepiness may correlate both with dizziness and depression. Although these factors were independently associated with dizziness in the present study, our statistical analysis did not provide any estimate of the weight of these associations. A study of 120 elderly individuals with chronic vestibular syndrome suggested - in a linear regression model - that having more symptoms of depressions was associated with memory and concentration disorders, among other factors21.
Poor perception of health was independently associated with dizziness, which concurs with other population-based studies4,46. Elderly subjects that considered their health as poor and very poor had 4.19 times the chance (CI 95%; 2.77-6.33) of complaining of dizziness compared to those without these complaints.
In the present study, 51.4% of elderly subjects that had falls reported dizziness, and 64.1% of elderly individuals with recurring galls reported dizziness. Stevens et al.8 argued that dizziness was strongly associated with falls, even after adjusting for gender (odds ratio - 2.11 95%; CI 1.69-2.64). Gassmann & Rupprecht4 found that elderly subjects reporting falls within the past six months had a 3.24 chance of manifesting dizziness compared to elderly individuals that did not fall. Stability and postural orientation mechanisms should work adequately to avoid falls. Most disorders involving dizziness interfere with that control, and may increase the susceptibility of elderly individuals to falls. Furthermore, elderly subjects with dizziness in the present study had a poorer perception of self-efficacy in avoiding falls; they were more fearful of falls compared to elderly individuals without dizziness. A study of 200 elderly individuals aged 60 year or more that were monitored at a geriatrics outpatient clinic showed that patients with chronic dizziness had a 4.9 higher chance of manifesting fear of falling (CI 95%; 2.2-11.1) compared to elderly individuals without dizziness48.
Among the physical and functional tests, there was an association between dizziness and left one-leg balance time and the SPPB score, showing that elderly patients with dizziness scored significantly worse than subjects without dizziness. The leg balance test places a high demand on musculoskeletal system control and mid-lateral body stability, and has been used to identify older adults at a higher risk of falling49. The SPPB consists of a test battery for static equilibrium with a progressive decrease of support, usual gait speed, sitting and standing sub-test. Other studies have reported a significant association between dizziness and poor performance on static equilibrium tests similar to those used in this study8,10.
This population-based and epidemiological study was carried out using a representative sample of community-dwelling elderly subjects, and was based on a multidimensional assessment tool. The findings, therefore, are highly relevant for establishing the profile of elderly individuals presenting dizziness within the past year. Due to its cross-sectional design, however, no causal relationships could be established.
It is important to highlight the importance of screening for dizziness in the elderly community, due to its high prevalence and impact on health and function in the elderly. Dizziness is sometimes overlooked because of its complex and multifactorial etiology. However, a correct diagnosis and treatment may avoid loss of health in this population.
CONCLUSION
Dizziness is a common complaint in elderly individuals. It is most frequently characterized as being sporadically present for at least one year and lasting a few seconds. The main reported triggering activities for dizziness are standing from a lying or sitting position and turning the head. Significantly associated factors were female gender, depression, memory disorders, poor perception of health, co-morbidities, fatigue, excessive sleepiness, fear of falling, and poor performance in physical/functional tests of body balance. These data suggest that a multifactorial approach of dizziness in elderly individuals and interventions for improving the functional capacity and preventing falls are important.
REFERENCES
1. Agrawal Y, Carey JP, Della Santina CC, Schubert MC, Minor LB. Disorders of balance and vestibular function in US adults: data from the National Health and Nutrition Examination Survey, 2001-2004. Arch Intern Med. 2009;169(10):938-44.
2. Neuhauser HK. Epidemiology of vertigo. Curr Opin Neurol. 2007;20(1):40-6.
3. Ricci NA, Aratani MC, Dona F, Macedo C, Caovilla HH, Gananca FF. A systematic review about the effects of the vestibular rehabilitation in middle-age and older adults. Rev Bras Fisioter. 2010;14(5):361-71.
4. Gassmann KG, Rupprecht R. Dizziness in an older community dwelling population: a multifactorial syndrome. J Nutr Health Aging. 2009;13(3):278-82.
5. Ekwall A, Lindberg A, Magnusson M. Dizzy - why not take a walk? Low level physical activity improves quality of life among elderly with dizziness. Gerontology. 2009;55(6):652-9.
6. Colledge NR, Wilson JA, Macintyre CC, MacLennan WJ. The prevalence and characteristics of dizziness in an elderly community. Age Ageing. 1994;23(2):117-20.
7. Nazareth I, Landau S, Yardley L, Luxon L. Patterns of presentations of dizziness in primary care--a cross-sectional cluster analysis study. J Psychosom Res. 2006;60(4):395-401.
8. Stevens KN, Lang IA, Guralnik JM, Melzer D. Epidemiology of balance and dizziness in a national population: findings from the English Longitudinal Study of Ageing. Age Ageing. 2008;37(3):300-5.
9. Maarsingh OR, Dros J, Schellevis FG, van Weert HC, Bindels PJ, Horst HE. Dizziness reported by elderly patients in family practice: prevalence, incidence, and clinical characteristics. BMC Fam Pract. 2010;11:2.
10. Tinetti ME, Williams CS, Gill TM. Dizziness among older adults: a possible geriatric syndrome. Ann Intern Med. 2000;132(5):337-44.
11. Aratani MC, Gazzola JM, Perracini MR, Ganança FF. Quais atividades diárias provocam maior dificuldade para idosos vestibulopatas crônicos. Acta ORL. 2006;25:18-24.
12. Aratani MC, Perracini MR, Caovilla HH, Gazzola JM, Gananca MM, Gananca FF. Disability rank in vestibular older adults. Geriatr Gerontol Int. 2011;11(1):50-4.
13. Gazzola JM, Gananca FF, Aratani MC, Perracini MR, Gananca MM. Circumstances and consequences of falls in elderly people with vestibular disorder. Braz J Otorhinolaryngol. 2006;72(3):388-92.
14. Tinetti ME, Doucette J, Claus E, Marottoli R. Risk factors for serious injury during falls by older persons in the community. J Am Geriatr Soc. 1995;43(11):1214-21.
15. Nguyen ND, Pongchaiyakul C, Center JR, Eisman JA, Nguyen TV. Identification of high-risk individuals for hip fracture: a 14-year prospective study. J Bone Miner Res. 2005;20(11):1921-8.
16. Herdman SJ, Blatt P, Schubert MC, Tusa RJ. Falls in patients with vestibular deficits. Am J Otol. 2000;21(6):847-51.
17. Cohen H. Vestibular rehabilitation improves daily life function. Am J Occup Ther. 1994;48(10):919-25.
18. Jacobson GP, Newman CW. The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg. 1990;116(4):424-7.
19. Tinetti ME, Williams CS, Gill TM. Health, functional, and psychological outcomes among older persons with chronic dizziness. J Am Geriatr Soc. 2000;48(4):417-21.
20. Gazzola JM, Gananca FF, Aratani MC, Perracini MR, Gananca MM. Clinical evaluation of elderly people with chronic vestibular disorder. Braz J Otorhinolaryngol. 2006;72(4):515-22.
21. Gazzola JM, Aratani MC, Dona F, Macedo C, Fukujima MM, Gananca MM, et al. Factors relating to depressive symptoms among elderly people with chronic vestibular dysfunction. Arq Neuropsiquiatr. 2009;67(2B):416-22.
22. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146-56.
23. Ferrucci L, Guralnik JM, Studenski S, Fried LP, Cutler GB, Jr., Walston JD. Designing randomized, controlled trials aimed at preventing or delaying functional decline and disability in frail, older persons: a consensus report. J Am Geriatr Soc. 2004;52(4):625-34.
24. Bertolucci PHF, Brucki SMD, Campacci SR, Juliano Y. O mini-exame do estado mental em uma população geral: impacto da escolaridade. Arq Neuropsiquiatr. 1994;52(1):1-7.
25. Brucki SMD, Nitrini RPC, Bertolucci PHF, Okamoto IO. Sugestões para o uso do mini-exame do estado mental no Brasil. Arq Neuropsiquiatr. 2003;61(3B):777-81.
26. Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189-98.
27. Lipschitz DA. Screening for nutritional status in the elderly. Prim Care. 1994;21(1):55-67.
28. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179-86.
29. Reuben DB, Laliberte L, Hiris J, Mor V. A hierarchical exercise scale to measure function at the Advanced Activities of Daily Living (AADL) level. J Am Geriatr Soc. 1990;38(8):855-61.
30. Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing. 2005;34(6):614-9.
31. Camargos FF, Dias RC, Dias JM, Freire MT. Cross-cultural adaptation and evaluation of the psychometric properties of the Falls Efficacy Scale-International Among Elderly Brazilians (FES-I-BRAZIL). Rev Bras Fisioter. 2010;14(3):237-43.
32. Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17(1):37-49.
33. Paradela EM, Lourenco RA, Veras RP. Validation of geriatric depression scale in a general outpatient clinic. Rev Saúde Públ. 2005;39(6):918-23.
34. Batistoni SST, Neri AL, Cupertino APFB. Validity of the Center for Epidemiological Studies Depression Scale among Brazilian elderly. Rev Saúde Públ. 2007;41(4):598-605.
35. Bertolazi AN, Fagondes SC, Hoff LS, Pedro VD, Barreto SSM, Johns MW. Validação da escala de sonolência de Epworth em português para uso no Brasil. J Bras Pneumol. 2009;35(9):877-83.
36. Podsiadlo D, Richardson S. The timed "Up & Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142-8.
37. Van Iersel MB, Munneke M, Esselink RA, Benraad CE, Olde Rikkert MG. Gait velocity and the Timed-Up-and-Go test were sensitive to changes in mobility in frail elderly patients. J Clin Epidemiol. 2008;61(2):186-91.
38. Murphy MA, Olson SL, Protas EJ, Overby AR. Screening for Falls in Community-Dwelling Elderly. J Aging Phys Act. 2003;11:66-80.
39. Vellas BJ, Wayne SJ, Romero L, Baumgartner RN, Rubenstein LZ, Garry PJ. One-leg balance is an important predictor of injurious falls in older persons. J Am Geriatr Soc. 1997;45(6):735-8.
40. Cesari M, Onder G, Russo A, Zamboni V, Barillaro C, Ferrucci L, et al. Comorbidity and physical function: results from the aging and longevity study in the Sirente geographic area (ilSIRENTE study). Gerontology. 2006;52(1):24-32.
41. Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85-94.
42. Studenski S, Perera S, Wallace D, Chandler JM, Duncan PW, Rooney E, et al. Physical performance measures in the clinical setting. J Am Geriatr Soc. 2003;51(3):314-22.
43. Nakano MM. Versão Brasileira da Short Physical Performance Battery - SPPB: adaptação cultural e estudo de confiabilidade. [Dissertação]. Campinas: Universidade Estadual de Campinas; 2007.
44. Jonsson R, Sixt E, Landahl S, Rosenhall U. Prevalence of dizziness and vertigo in an urban elderly population. J Vestib Res. 2004;14(1):47-52.
45. Tamber AL, Bruusgaard D. Self-reported faintness or dizziness -- comorbidity and use of medicines. An epidemiological study. Scand J Public Health. 2009;37(6):613-20.
46. Gopinath B, McMahon CM, Rochtchina E, Mitchell P. Dizziness and vertigo in an older population: the Blue Mountains prospective cross-sectional study. Clin Otolaryngol. 2009;34(6):552-6.
47. Cabral GTR, Correa LB, Silveira SR, Lopes RP. Interferência da queixa de tontura na qualidade de vida dos idosos cadastrados na UBS do bairro Araçás, Vila Velha/ES. Acta ORL. 2009;27(2):58-63.
48. Perez-Jara J, Enguix A, Fernandez-Quintas JM, Gomez-Salvador B, Baz R, Olmos P, et al. Fear of falling among elderly patients with dizziness and syncope in a tilt setting. Can J Aging. 2009;28(2):157-63.
49. Hurvitz EA, Richardson JK, Werner RA, Ruhl AM, Dixon MR. Unipedal stance testing as an indicator of fall risk among older outpatients. Arch Phys Med Rehabil. 2000;81(5):587-91.
1. Physical therapist, specialist, master's degree student in physical therapy, São Paulo City University (Universidade Cidade de São Paulo, UNICID).
2. Physical therapist, master's degree in physical therapy, São Paulo City University (UNICID). Higher education level technician of the Health Secretariat of Mato Grosso state.
3. Physical therapist, master's degree student, Mato Grosso Federal University (UFMT).
4. Physical educator, doctoral degree in medical science, Ribeirão Preto Medical School, Sao Paulo University (Faculdade de Medicina de Ribeirão Preto, USP). Faculty member of the Physical Education School, UFMT.
5. Physician, doctoral degree in medicine, São Paulo University (USP). Faculty member of the Internal Medicine Department, Ribeirão Preto Medical School, USP.
6. Doctoral degree in science, Sao Paulo Federal University (Universidade Federal de São Paulo, UNIFESP). Faculty member of the Master's Degree Program in Physical Therapy, UNICID.
São Paulo City University (Universidade Cidade de São Paulo, UNICID). Mato Grosso Federal University (Universidade Federal do Mato Grosso). Ribeirão Preto Medical School, São Paulo University (USP).
Send correspondence to:
Monica R Perracini
Rua Cesáreo Galeno, 448, Tatuapé
São Paulo - SP. CEP: 03071-000
E-mail: mrperracini@cidadesp.edu.br
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on March 4, 2011.
Accepted on June 21, 2011. cod. 7619.
CNPq Edict 17/2006 - "Rede Fibra Auxílio a Projeto de Pesquisa" in the name of Monica R Perracini - FAPEMAT no.002.0174/2007