Year: 2010 Vol. 76 Ed. 6 - (17º)
Artigo Original
Pages: 776 to 782
Polymorphism of Methylenetetrahydrofolate Reductase (MTHFR) gene and risk of head and neck squamous cell carcinoma
Author(s): Juliana Olsen Rodrigues1; Ana Lívia Silva Galbiatti2; Mariangela Torreglosa Ruiz3; Luiz Sergio Raposo4; José Victor Maniglia5; Érika Cristina Pavarino-Bertelli6; Eny Maria Goloni-Bertollo7
Keywords: genes, head and neck neoplasms, polymorphism.
Abstract:
Methylenetetrahydrofolate reductase gene (MTHFR) C677T polymorphism may be a risk factor for head and neck squamous cell carcinoma due to changes in folate levels that can induce disorders in the methylation pathway, which results in carcinogenesis. Aim: To evaluate MTHFR C677T polymorphism in patients with head and neck squamous cell carcinoma and in individuals with no history of cancer, and to assess the association of this disease with clinical histopathological parameters. Series and Methods: A retrospective study that assessed gender, age, tobacco, alcohol consumption and clinical histopathological parameters in 200 patients (100 with disease and 100 with no history of cancer). PCR-RFLP molecular analysis was carried out and the chi-square test and multiple logistic regression were applied for the statistical analysis. Results: There was no association between MTHFR C677T polymorphism and head and neck cancer (p = 0.50). Significant differences between the study and control groups were observed at age over 50 years, tobacco use, and male gender (p <0.001). There was no association of disease with clinical-histopathological parameters. Conclusion: No association between the MTHFR C677T polymorphism and head and neck squamous cell carcinoma was possible in this study.
![]()
INTRODUCTION
Head and neck squamous cell carcinoma is one of the five most common types of cancer worldwide. It is sixth in cancer mortality and comprises cancers of the mouth (40%), pharynx (15%), and larynx (25%).1
Head and neck squamous cell carcinoma patients are generally diagnosed at a late stage of the disease; about 75% of cases are diagnoses in stages III or IV. The situation is worse in developing countries, such as India, Thailand and Brazil,3 where this cancer is more common.4 The mean survival rate in these patients is 5 years.5 The 5-year life expectancy is about 50% when there are lymph node metastases.6,7 No significant increase in survival rates had occurred in the last few decades in spite of new surgical techniques, radiotherapy and concomitant chemotherapy.4,5,6,8
Epidemiologic studies have suggested a multifactor etiology for this cancer; these predisposing factors include smoking, alcohol use, human papilloma virus (HPV) infection, and genetic factors.1,4,7,9,10
Genetic polymorphisms leading to folate deficiency appear to facilitate the onset and growth of head and neck squamous cell carcinoma and other types of cancer. Folate is part of DNA methylation, in which methyl groups (CH3) are transferred to the 5' position of cytosine residues on cytosine-guanine (CpG) dinucleotides in reactions catalyzed by proteins (DNA methyltransferases).11 This epigenetic modification of DNA has several functions, such as controlling gene expression, stabilizing the chromatin structure, and maintaining genomic stability.11-22
C677T polymorphism of the methyenetetrahydrofolate reductase (MTHFR) gene appears to be related with cancer susceptibility because the activity of the MTHFR enzyme (which is part of folate metabolism) is reduced; this may cause uncontrolled gene expression, genomic instability, and induce carcinogenesis.23,24
Because of the significant ethnic and geographic variation in the frequency of the C677T variant of the MTHFR gene, researchers have evaluated the Hardy-Weinberg equilibrium of this gene in different populations to study whether allele frequencies remain unaltered across generations. Jim et al.'s meta-analysis (2009)25 investigated five Asian and five European or American ethnic populations and confirmed that the genotype distribution in the control group in two studies did not abide by the Hardy-Weinberg principle. Studies by Suzuki et al. (2007),15 Solomon et al. (2008),26 and Kruszyna et al. (2009),27 respectively in Asian, Polish and Indian populations, found that genotype frequencies were in Hardy-Weinberg equilibrium.
Based on current evidence, the purpose of this study was to identify MTHFR C677T polymorphism in patients with head and neck squamous cell carcinoma and in subjects with no history of cancer, and to investigate associations between this polymorphism, clinical findings, demographic data (age and gender) and risk factors (smoking habits and alcohol consumption) in this disease.
SERIES AND METHODS
The institutional review board of the institution approved this study (number 5566/2005).
There were 200 subjects in this study; 100 (84 male and 16 female; mean age - 59.05 ± 10.4 years) were patients with a histopathologic diagnosis of head and neck squamous cell carcinoma, seen at a university hospital in the Northeastern part of São Paulo state, and 100 other subjects (76 male and 24 female; mean age - 43.61 ± 2.2 years) that had no medical history of cancer. Subjects were included in the study after signing a free informed consent form.
The control group included individuals from the blood bank of São José de Rio Preto, with no diagnosis of cancer according to the blood donor protocol that assesses 20 diseases (http://www.hemonline.com.br/portarias/rdc153/indexframe.htm). Another inclusion criterion was age over 40 years; exclusion criteria were a family history of cancer and the presence of any disease in the blood donor protocol. The study group consisted of patients with a diagnosis of head and neck carcinoma based on pathology specimens from biopsies or total excision. The inclusion criterion was patients with the squamous cell histological type; previously treated patients were excluded.
The study variables were age, gender, exposure to risk factors (alcohol consumption and cigarette smoking), and tumor-related clinical parameters. Smokers were defined here as subjects that had smoked about 100 cigarettes in their lives, and alcohol consumers were subjects that drank more than four drinks a week.28,29 The clinical parameters included the primary sites of tumors (mouth, pharynx and larynx); tumors were classified according to the parameters issued by the Union International Control Cancer (IUCC), 2002, and the American Joint Committee for Cancer (AJCC), 2002, as follows: tumor size (T), and presence of involved regional lymph nodes (N). Clinical and pathology data were gathered from medical registries.
Extracted genomic DNA, according to Miller et al. (1998), modified,30 was PCR-amplified, according to Yi et al., 2002.31 The amplification product was digested with the Hinf I restriction enzyme according to the manufacturer's instructions, to detect the polymorphic site (MTHFR 677T).
The multiple logistic regression model was applied to evaluate the effect of variables and the genotype distribution among groups. The model included the following variables: age (reference: age below the median in both groups), gender (reference: female sex), smoking habits (reference: non-smokers); alcohol consumption (reference: non-drinkers).
Multiple logistic regression was also applied to analyze the clinical features and pathology. The T classification was the same in small (T1, T2) and large tumors (T3, T4). The N classification was separated into negative (N0) and positive lymph node involvement (N1, N2, N3).
Results are presented as odds ratio (OR) and 95% confidence intervals (CI - 95%). The significance level was 5% (p=0.05). The Bioestat and Instat software packages were used in the statistical analysis.
RESULTS
Table 1 presents the social and demographic data of 100 patients with head and neck squamous cell head and neck squamous cell carcinoma and of 100 subjects with no history of cancer. There were significant differences between the study and control groups at ages over 50 years, smoking habits, and male gender (p < 0.001). There were 160 male subjects (80%; 84 patients and 76 controls) and 40 female subjects (20%; 16 patients and 24 controls). Smokers comprised 88% of the study group, compared to 43% in the control group. Alcohol consumers were 77% of the study group and 49% of controls. There was no significant difference between these groups (p=0.06).
The Hardy-Weinberg equilibrium showed that genotype distributions were similar to those expected among patients (X2 = 1.18; p = 0.23) and in controls (X2 = 0.23; p = 0.63). The genotype CC, CT and CC frequencies of the C677T polymorphism were respectively 44%, 43% and 13% for patients, and 46%, 40% and 14% in controls. There were no significant differences in genotype distribution between groups (p= 0.92).
The allele frequencies for head and neck cancer patients were respectively, C=0.65 and T=0.35, and for controls C=0.66 and T=0.34. There were no statistically significant differences between groups (p=1.00).
The multiple logistic regression test was applied to evaluate the effect of variables on disease progression (genotypes, age, gender, smoking and alcohol consumption) (see Table 1). Age over 50 years (OR = 20.81; CI= 9.01 to 48,09; p < 0.0001) and smoking (OR= 5.03; CI =1.93 to 13.15; p < 0.001) were predictors of disease.
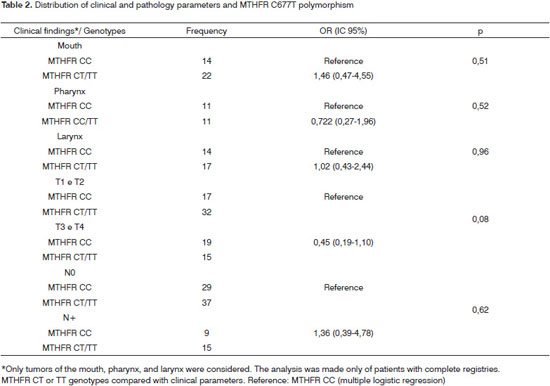
Polymorphism was not associated with primary tumor sites (mouth, pharynx and larynx), tumor extension, and lymph node involvement. Primary sites were the mouth (34% of patients), the larynx (31%), and the larynx (22%). The remaining sites were unknown. The TNM classification was stages T1 or T2 in 59% of patients - of which 34,6% had the CC wild genotype, and 65.4% had at least one mutated allele (CT or TT genotypes). The remaining patients (41%) were stages T3 or T4, of which 55% had the CC wild genotype, and 45% had at least one mutated allele (CT or TT genotypes). Lymph nodes were involved (N+) in 26.6% of patients (37.5% with the CC genotype, and 62.5% with at least one mutated allele - CT or TT genotypes).
DISCUSSION
This study showed that head and neck squamous cell carcinoma is more frequent in smokers aged over 50 years. Published results have also shown that this cancer is more frequent after the fifth decade of life and in smokers.32-34
No relationship between alcohol consumption and head and neck squamous cell carcinoma was found, such as in the study by Boccia et al. (2009).35 Animal studies have suggested that alcohol is not genotoxic, but that it may act as a solvent for the entry of carcinogens. Acetaldehyde, the primary metabolite of alcohol, is highly reactive and binds to proteins, cells substrates, and DNA, forming DNA adducts.36-38 Excessive alcohol consumption may also lead to nutritional deficiencies because of impaired intestinal absorption and altered metabolic pathways.39 The results of a multicenter study have suggested that in the absence of smoking, the association between alcohol consumption and head and neck carcinoma is insignificant; alcohol appears to be carcinogenic only at high doses.40
We found no association between gender and this disease in our series; other studies, however, have found this association and have suggested that the incidence of this disease in females has increased in the past few decades. Males are still more affected by this type of tumor.41,42
MTHFR C677T polymorphism has been studied as a risk factor for cancer susceptibility because of its effect on cell methylation reactions and DNA synthesis. Global genome hypomethylation occurs with greater frequency in tumors compared to normal cells; it is thought that increased oncogene expression by result from hypomethylation. On the other hand, hypermethylation of CpG islands located in gene promoting regions has been associated with altered gene expression, resulting in tumor suppressing gene silencing.43
The genotype frequencies in our study were in Hardy-Weinberg equilibrium. The polymorphic genotype (MTHFR 677TT) was found in 14% of controls and 13% of patients with head and neck squamous cell carcinoma. There is considerable ethnic and geographic variation in the frequency of the C677T variant of the MTHFR gene. The prevalence of the MTHFR 677TT genotype ranges from 1% in blacks (US, Africa and South America) to over 20% in Europeans, Colombians, and American Indians; 12% of Japanese were TT homozygotes.44 Because of the ample mixture of races in the Brazilian population, no analysis of ethnic prevalence were made in our series.
We found no association between MTHFR C677T polymorphism and head and neck carcinoma in our series. Other studies have shown an association between this polymorphism and several cancers, such as those of the lung45,35 liver (hepatocellular carcinoma),46 a few leukemias,47 prostate cancer,48 breast,49 colon,49 endometrium, esophagus, stomach, pancreas, and bladder.46 A meta-analysis of nine head and neck carcinoma studies found no association between this polymorphism and this disease, which concurs with our results.32 However, Reljic et al. (2007)50 and Solomon et al. (2008)26 found that head and neck carcinoma and the MTHFR C677T polymorphism were associated in Croat and Indian populations.
Reljic et al. (2007)50 studied 81 patients with head and neck carcinoma and 102 controls, and found a statistically significant difference in the genotype distribution of both groups, which provides evidence of a possible association between MTHFR C677T polymorphism and head and neck carcinoma. This analysis revealed that the 677CT genotype reduces the risk of this disease by 2.8 times. Solomon et al. (2008)26 studied 126 Indian subjects with mouth carcinoma (33 were alcohol consumers, 56 were moderate alcohol consumers, and 37 did not consume alcohol) and showed that alcohol consumers with the MTHFR 677TT genotype were at a higher risk for developing mouth carcinoma (OR - 3.0; 95% CI = 2.02-4.0) and that the TT genotype protected only non-alcohol and moderate alcohol consumers.
There are no published studies describing abnormalities of the gene above and head and neck squamous cell carcinoma in Brazil; although our results were not statistically significant, it is interesting to study these abnormalities because of contradictory results and the paucity of studies.
The most frequent tumor site was the mouth - 40% of head and neck cancers.51,52 In the TNM classification, 19% of cases were stage T1, 30% were stage T2, 17% were stage T3, and 17% were stage T4. Lymph nodes were not involved in 73.4% of patients, and there were no metastases in 99% of cases. A retrospective Brazilian study revealed a high frequency of this disease at advanced stages.53 This discrepancy with our findings appears to reflect the type of study population; in our case, monitored patients.
MTHFR C677T polymorphism was not associated with the clinical parameters of this study (primary tumor sites, tumor extension, and lymph node involvement). Capaccio et al.54 (20050 studied the presence of this polymorphism in several oropharyngeal anatomical sites and found no association among the abovementioned variables. There was no association between this polymorphism and disease extension (T stage) and tumor staging in the three regions of the head and neck (mouth, pharynx, and larynx) when analyzing tumor aggressiveness, which concurs with Vairaktaris et al.'s (2006) study.55
CONCLUSION
To conclude, no associations were found between MTHFR C677T polymorphism and head and neck squamous cell carcinoma. Our data showed that the frequency of this disease is higher after the fifth decade of life and in smokers. Clarifying any association between this polymorphism and head and neck carcinoma - and the association of this cancer type with other risk factors - will help understand the neoplastic mechanisms underlying this disease, as well as prevention and control measures.
REFERENCES
1. Gallì P, Cadoni G, Volante MM, Feo ED, Amore R, Giorgio et al.. A case-control study on the combined effects of p53 and p73 polymorphisms on head and neck cancer risk in an Italian population. BMC Cancer. 2009; 9:137.
2. Alvarenga LM, Ruiz M T, Bertelli ECP, Ruback MJC, Maniglia JV, Bertollo E MG. Epidemiologic evaluation of head and neck patients in a university hospital of Northwestern São Paulo State. Braz J Otorhinolaryngol. 2008; 74(1):68-73.
3. Awada A, Junior GC. Head and neck cancer emerging strategies: advances and new challenges. Curr Opin Oncol. 2009; 21(3):191-3.
4. Farshadpour F, Hordijk GJ, Koole R, Slootweg PJ. Head and neck squamous cell carcinoma in non-smoking and non-drinking patients with multiple tumors: etiologic significance of p53 and Ki-67 in non-tumorous epithelium. J Oral Pathol Med. 2008; 37: 549-54.
5. Escher A, Piotet E, Waridel F, Iggo R, Monnier P. p53 mutation in histologically normal mucosa of the aero-digestive tract is not a marker of increased risk for second primary carcinoma in head and neck cancer patients. Eur Arch Otorhinolaryngol. 2009; 266(4):547-51.
6. Tachezy R, Klozar J, Rubenstein L, Smith E, Sala'kova' M, S mahelova' J et al.. Demographic and Risk Factors in Patients With Head and Neck Tumors. J Med Virol. 2009; 81:878-87.
7. Gold KA, Kim ES. Role of molecular markers and gene profiling in head and neck cancers. Curr Opin Oncol. 2009; 21:206-11.
8. Mitani T, Hoshikawa H, Mori T, Hosokawa T, Tsukamoto I, Yamaguchi F et al.. Growth inhibition of head and neck carcinomas by d-allose. Head Neck. 2009; 31(8):1049-55.
9. Poeta M L, Manola J, Goldwasser MA, Forastiere A, Benoit N, Califano JA et al.. TP53 Mutations and Survival in Squamous-Cell Carcinoma of the Head and Neck. N Engl J Med. 2007; 20; 357(25): 2552-61.
10. Kumar B, Cordell K G, Lee J S, Worden F P, Prince M E, Tran H H et al.. EGFR, p16, HPV Titer, Bcl-xL and p53, Sex, and Smoking As Indicators of Response to Therapy and Survival in Oropharyngeal Cancer. J Clin Oncol. 2008; 26:3128-37.
11. DAlessio AC, Szyf M. Epigenetic tête-à-tête: the bilateral relationship between chromatin modifications and DNA methylation. Biochem Cell Biol. 2006; 84(4):463-76.
12. Ehrlich M. The ICF syndrome, a DNA methyltransferase 3B deficiency and immunodeficiency disease.Clinical Immunology.2003; 109: 17-28.
13. Tuck-Muller CM, Narayan A, Tsien F, Smeets DF, Sawyer J, Fiala ES, et al. DNA hypomethylation and unusual chromosome instability in cell lines from ICF syndrome patients. Cytogenet Cell Genet. 2000; 89(1-2):121-8.
14. Zhang Z, Shi Q, Liu Z, Sturgis EM, Spitz MR, WeiQ. Polymorphisms of Methionine Synthase and Methionine Synthase Reductase and Risk of Squamous Cell Carcinoma of the Head and Neck: A Case-Control Analysis. Cancer Epidemiol Biomarkers Prev. 2005; 14(5) 1188-93.
15. Suzuki T, Matsuo K, Hasegawa Y, Hiraki A, Wakai K, Hirose K, et al.. One-carbon metabolism-related gene polymorphisms and risk of head and neck squamous cell carcinoma: Case-control study. Cancer Sci. 2007; 98(9):1439-46.
16. Pande M, Chen J, Amos CI, Lynch PM, Broaddus R, Frazier ML. Influence of Methylenetetrahydrofolate Reductase Gene Polymorphisms C677T and A1298C on Age-Associated Risk for Colorectal Cancer in a Caucasian Lynch Syndrome Population. Cancer Epidemiol Biomarkers Prev. 2007; 16:1753-9.
17. Kim DH. The interactive effect of methyl-group diet and polymorphism of methylenetetrahydrofolate reductase on the risk of colorectal cancer. Mutat Res. 2007; 622: 14-8.
18. Ouerhani S, Oliveira E, Marrakchi R, Ben Slama MR, Sfaxi M, Ayed M et al.. Methylenetetrahydrofolate reductase and methionine synthase polymorphisms and risk of bladder cancer in a Tunisian population. Cancer Genet Cytogenet. 2007; 176(1):48-53.
19. Mu LN, Cao W, Zhang ZF, Yu SZ, Jiang QW, You NC et al.. Polymorphisms of 5,10-methylenetetralydrofolate reductase (MTHFR), fruit and vegetable intake, and the risk of stomach. Biomarkers. 2007; 12: 61-75.
20. Ott N, Geddert H, Sarbia M. Polymorphisms in methionine synthase (A2756G) and cystathionine beta-synthase (844ins68) and susceptibility to carcinomas of the upper gastrointestinal tract. J Cancer Res Clin Oncol. 2008; 134:405-10.
21. Galván-Portillo MV, Oñate-Ocaña LF, Pérez-Pérez GI, Chen J, Herrera-Goepfert R, Chihu-Amparan L et al.. Dietary folate and vitamin B12 intake before diagnosis decreases gastric cancer mortality risk among susceptible MTHFR 677TT carriers. Nutrition. 2009. [no prelo]
22. Gao CM, Tang JH, Cao HX, Ding JH, Wu JZ, Wang J et al.. MTHFR polymorphisms, dietary folate intake and breast cancer risk in Chinese women. J Hum Genet. 2009; 54(7):414-8.
23. Duthie SJ. Folic acid deficiency and cancer: mechanisms of DNA instability. Br Med Bull. 1999; 55(3):578-92.
24. Ames BN. DNA damage from micronutrient deficiencies is likely to be a major cause of cancer. Mutat Res. 2001; 475:7 - 20.
25. Jin F, Qu LS e Shen XZ. Association between the methylenetetrahydrofolate reductase C677T polymorphism and hepatocellular carcinoma risk: a meta-analysis. Diagn Pathol. 2009, 4:39.
26. Solomon PR, Selvan GS, Shanmugam G. Polymorphism in ADH and MTHFR genes in oral squamous cell carcinoma of Indians. Oral Dis. 2008; 14: 633-9.
27. Kruszyna L, Lianeri M, Rydzanicz M, Gajecka M, Szyfter K, Jagodzinski PP. Polymorphic variants of folate metabolism genes and the risk of laryngeal cancer. Mol Biol Rep. 2010; 37: 241-7.
28. Ahrendt SA, Chown JT, Yang SC, Wu L, Zhang MJ, Jen J et al.. Alcohol consumption and cigarette smoking increase the frequency of p53 mutations in non-small cell lung cancer. Cancer Res. 2000; 60:3155-9.
29. Kjaerhein K, Gaard M, Andersen A. The role of alcohol, tobacco, and dietary factors in upper aerogastric tract cancer: a prospective study of 10.900 Norwegian men. Cancer Causes Control. 1998; 9: 99-108.
30. Miller SA, Dikes DD e Polesky HF. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Research. 1988; 16: 1215.
31. Yi P, Pogribny IP, James SJ. Multiplex: PCR for simultaneous detection of 677 C-T and 1298 A - C polymorphisms in methylenetetrahydrofolate reductase gene for population studies of cancer risk. Cancer Letters. 2002; 181:209-13.
32. Kreimer AR, Clifford GM, Boyle P, Franceschi S. Human papillomavirus types in head and neck squamous cell carcinomas worldwide: a systematic review. Cancer Epidemiol Biomarkers Prev. 2005;14:465-75.
33. Psyrri A, DiMaio D. Human papillomavirus in cervical and head-and-neck cancer. Nat Clin Pract Oncol. 2006; 5: 24-31.
34. Guha N, Boffetta P, Wünsch Filho V, Eluf Neto J, Shangina O, Zaridze D et al.. Oral health and risk of squamous cell carcinoma of the head and neck and esophagus: results of two multicentric case-control studies. Am J Epidemiol. 2007;166:1159-73.
35. Boccia S, Boffetta P, Brennan P, Ricciardi G, Gianfagna F, Matsuo K et al.. Meta-analyses of the methylenetetrahydrofolate reductase C677T and A1298C polymorphisms and risk of head and neck and lung cancer. Cancer Letters. 2009; 273 55-61.
36. Hashibe M, Brennan P, Benhamou S, Castellsague X, Chen C, Curado MP et al.. Alcohol drinking in never users of tobacco, cigarette smoking in never drinkers, and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. J Natl Cancer Inst. 2007; 99: 777 - 89.
37. Boffetta P, Hashibe M. Alcohol and cancer. Lancet Oncol. 2006; 7:149-56.
38. Warnakulasuriya S, Parkkila S, Nagao T, Preedy VR, Pasanen M, Koivisto H et al.. Demonstration of ethanol-induced protein adducts in oral leukoplakia (pre-cancer) and cancer. J Oral Pathol Med.2008; 37: 157-65.
39. Lee YC, Boffetta P, Sturgis EM, Wei Q, Zhang ZF, Muscat J et al.. Involuntary smoking and head and neck cancer risk: pooled analysis in the international head and neck cancer epidemiology consortium. Cancer Epidemiol Biomarkers Prev. 2008; 17:1974-81.
40. Hashibe M, Brennan P, Benhamou S, Castellsague X, Chen C, Curado MP et al.. Alcohol drinking in never users of tobacco, cigarette smoking in never drinkers, and the risk of head and neck cancer: pooled analysis in the International Head and Neck. J Natl Cancer Inst. 2007; 99(10):777-89.
41. Vaezi MF, Sepi M, Qadeer MA, Lopez R, Colabianchi N. Laryngeal cancer and gastroesophageal reflux disease: a case-control study. Am J Med. 2006; 119:768-76.
42. Qadeer MA, Colabianchi N, Strome M, Vaezi MF. Gastroesophageal reflux and laryngeal cancer: causation or association? A critical review. Am J Otolaryngol. 2006; 27:119- 28.
43. Beier V, Mund C, Hoheisel JD. Monitoring methylation changes in cancer. Adv Biochem Eng Biotechnol. 2007;104:1-11.
44. Botto LD, Yang Q. 5,10-Methylenetetrahydrofolate reductase gene variants and congenital anomalies: a HuGE review. Am J Epidemiol. 2000; 151(9):862-77.
45. Jeng YL, Wu MH, Huang HB, Lin WY, You SL, Chu TY et al.. The methylenetetrahydrofolate reductase 677C-->T polymorphism and lung cancer risk in a Chinese population. Anticancer Res. 2003; 23: 5149-52.
46. Sohn K J, Jang H, Campan M, Weisenberger DJ, Dickhout J, Wang YC et al.. The methylenetetrahydrofolate reductase C677T mutation induces cell-specific changes in genomic DNA methylation and uracil misincorporation: A possible molecular basis for the site-specific cancer risk modification. Int J Cancer. 2009; 124, 1999-2005.
47. Krajinovic M, Lamothe S, Labuda D, Lemieux-Blanchard E, Theore TY, Moghrabi A et al.. Role of MTHFR genetic polymorphisms in the susceptibility to childhood acute lymphoblastic leukemia. Am Soc Hematol. 2004; 103:252-7.
48. Marchal C, Redondo M, Reyes-Engel A, Perea-Milla E, Gaitan MJ, Machuca J et al.. Association between polymorphisms of folate-metabolizing enzymes and risk of prostate cancer. Eur J Surg Oncol. 2008; 34:805-10.
49. Sohn KJ, Croxford R, Yates Z, Lucock M, Kim YI. Effect of the methylenetetrahydrofolate reductase C677T polymorphism on chemosensitivity of colon and breast cancer cells to 5-fluorouracil and methotrexate. J Natl Cancer Inst. 2004; 96:134-44.
50. Reljic A, Simundic AM, Topic E, Nikolac N, Justinic D, Stefanovic M. The methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism and cancer risk: The Croatian case-control study. Clinic Bioch. 2007; 40: 981- 5.
51. Dedivitis RA, França CM, Mafra ACB, Guimarães FT, Guimarães AV. Características clínicoepidemiológicas no carcinoma espinocelular de boca e orofaringe. Rev Bras Otorrinolaringol. 2004; 70: 35-40.
52. Döbrossy L. Epidemiology of head and neck cancer: magnitude of the problem. Cancer Metastasis Rev. 2005; 17: 24-9.
53. Wusch-Filho V. The epidemiology of oral and pharynx cancer in Brazil. Oral Oncol. 2002; 38:737-46.
54. Capaccio P, Ottaviani F, Cuccarini V, Cenzuales S, Cesana BM, Pignataro L. Association between methylenetetrahydrofolate reductase polymorphisms, alcoholintake and oropharyngolaryngeal carcinoma in northern Italy. J Laryngol Otol. 2005; 119(5):371-6.
55. Vairaktaris E, Yapijakis C, Kessler P, Vylliotis A, Ries J, Wiltfang J et al.. Methylenetetrahydrofolate reductase polymorphism and minor increase of risk for oral cancer. J Cancer Res Clin Oncol. 2006; 132(4):219-22.
FAMERP - Faculdade de Medicina (medical school) de São José do Rio Preto
Send correspondence to:
Faculdade de Medicina de São José do Rio Preto - FAMERP
Av. Brigadeiro Faria Lima 5416
São José do Rio Preto SP 15090-000
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on January 7, 2010;
and accepted on May 23, 2010. cod. 6868
Centro Nacional de Desenvolvimento Científico e Tecnológico (CNPq) Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (Capes)