Year: 2002 Vol. 68 Ed. 2 - (20º)
Relato de Caso
Pages: 280 to 283
Abducens paralysis as a complication of acute otitis media
Author(s):
Beatrice M. J. Neves 1,
Luc L. M. Weckx 2
Keywords: abducens paralysis, otitis media
Abstract:
The abducens paralysis is a rare complication of otitis media. In this paper, the authors reviewed the literature concerning otitis media complication and report one case of abducens paralysis and acute otitis media.
![]()
INTRODUCTION
Acute otitis media is a relatively severe disease owing to the possibility of having complications. As a result of routine use of antibiotics for acute otitis media and improvement in surgical techniques of the temporal bone, there has been a significant reduction in the incidence of complications associated to acute otitis media and in morbidity and mortality associated to these complications.
In a study conducted before the advent of antibiotics, Kafka1 analyzed 3,225 cases of mastoiditis (2,100 cases of acute mastoiditis and 1,125 cases of chronic mastoiditis). In cases of acute mastoiditis, 16.66% progressed with intracranial complications and mortality reached 71.45% in this group. Of the chronic cases, 13.55% progressed to intracranial complications and mortality rate in the group was 75%. Before the use of antibiotics, Profant2 documented three cases of petrositis that progressed to death; upon reviewing the literature at that time, out of 19 cases of petrositis, 5 of them progressed to death.
Although the incidence of otitis media complications has reduced after the advent of large spectrum antibiotics, mortality and morbidity are still high, especially in underdeveloped countries, as shown by the sample of the study conducted by Kangsanarak et al3 in Thailand. They retrospectively analyzed 102 cases of acute otitis media complications, divided into intracranial and extracranial. The prevalence of intracranial complications was 0.24% and of extracranial, 0.45%. In the group of extracranial complications, morbidity was 14.13% and mortality was 0%, whereas in the group of intracranial complications, morbidity was 27.9% and mortality was 18.6%.
Goycoolea and Jung4 classified otitis media complications into intratemporal and extratemporal (Table 1).
Table 1. Complication of Otitis Media.
Albers5, in his study, analyzed retrospectively 23 patients with intracranial or intratemporal complications of otitis media. The author found 28 complications, being that the most common intracranial complication was meningitis (12 patients) and the most common intratemporal one was facial paralysis (3 patients). Meningitis used to be the most common cause before the use of antibiotics, as shown by Kafka1 in his study, in which meningitis was detected in 36 patients of the 83 who had intracranial complications. Farrior6 analyzed retrospectively 135 cases of chronic otitis media complications in pediatric patients. The most common one was tympanic membrane perforation (57 cases), followed by cholesteatoma (54 cases).
Paralysis of abducent nerve, a consequence of petrositis, is a rare complication of acute otitis media. In Gradenigo's syndrome, one of the clinical expressions of petrositis, in addition to abducent nerve paralysis, there is also compromise of trigeminal nerve and otitis media.
The purpose of the present study was to show that despite being rare, acute otitis media complications are still present, by presenting a case of Gradenigo's syndrome.
case report
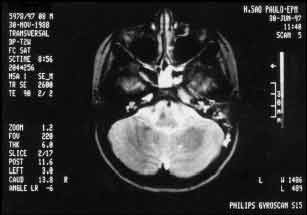
A female 8-year-old patient came to the emergency service of Otorhinolaryngology, UNIFESP-EPM, on June 26, 1997. She complained of frontal left headache and intermittent eye pain on the same side for seven days, which improved with common analgesics. After 4 days of headache, she started to have left ear suppuration without fever or otalgia. Five days after onset of symptoms, she experienced compromise of left eye motricity. She had used amoxicillin (3rd day) with no apparent response. Upon physical examination, she presented paresis of left lateral rectus muscle, diplopia in eye primary position and in all positions on the left, presence of purulent secretion on the external acoustic canal, with tympanic perforation on the anterior-inferior quadrant. Laboratory complementary tests: HS rate: 105, MRI: signs of mastoiditis on the left and inflammation of the temporal lobe apex on the left, probable thrombosis of the cavernous sinus on the left, and sphenoid sinusitis. After diagnosing the condition as Gradenigo's syndrome, the patient was admitted into the hospital and treated with ceftriaxone, metronidazole and dexamethasone. One week after, otoscopy was normal and we performed audiometry that revealed mild sensorineural hearing loss in 6kHz and moderate in 8kHz on the left ear and tympanometry showed type C curve on the left. Total recovery of ocular mobility was seen two months later. MRI performed after 4 months did not show any abnormalities.
Figure 1. (A) Patient on the first day of visit and (B) after 2 months, showing complete regression of clinical presentation.
Figure 2. Magnetic resonance imaging conducted on June 30, 1997, showing impairment of sphenoid sinus, signs of mastoiditis on the left, temporal lobe apex inflammation on the left and probable cavernous sinus thrombosis on the same side.
COMMENTS
The clinical case previously reported was caused by petrositis, which is a rare complication of otitis media, either chronic or acute. If acute, there is extension of the infectious process into the middle ear and mastoid to the aired cells of the petrous portion of the temporal bone. The condition, similarly to acute otitis media, is generally self-limited. If there is obstruction of the drainage of purulent secretion contained in the aired cells, the infectious process disseminates into the bone, causing the petrous osteomyelitis. The chronic form occurs as a complication of chronic otitis media and it is more common than the acute form. There is no need to have pneumatization of the petrous portion, since the infection occurs by thrombophlebitis leading to local osteomyelitis.
Bacteriology of acute petrositis is the same as for acute otitis, S. pneumoniae, H. influenzae. Similarly, the chronic form is the same as for chronic otitis media P. aeruginosa, Proteus.
The clinical picture of petrositis is characterized by retrocular pain, otalgia, purulent otorrhea and diplopia.
Ocular pain occurs by impairment of the major superficial petrous nerve or the ophthalmic branch of the trigeminal nerve. Less commonly, the maxillary branch and/or the mandibular branch may be affected, leading to pain in the teeth and mandible. Glasscock7 pointed out that retrocular pain in patients with otitis media is a warning sign, differently from otalgia, which may also affect otitis media patients without complications or post-radical mastoidectomy.
Abundant otorrhea, as in the reported case, is more common in acute petrositis and it may be even absent in chronic cases. Persistent otorrhea, even after mastoidectomy (simple or radical) performed by an experienced surgeon, is a strong indication of temporal bone petrous portion compromise, as observed in the studies conducted by Chole and Donald8 and by Glasscock7.
Diplopia is a result of abducent nerve paralysis caused by compression of the nerve when it passes through Dorelo's canal, owing to the edema present in the petrous apex region.
Petrositis may manifest a wide range of symptoms. In their study, Chole and Donald8 analyzed 8 cases of petrositis. The most common symptom was hearing loss (5 cases), followed by severe pain (facial or auricular - 4 cases). Abducent nerve paralysis was present in two cases and meningitis, in two cases. Seven patients presented affection of other cranial nerves (7th, 8th, 9th and 10th). In the three cases studied by Glasscock7, severe pain (auricular, facial and ocular) was constant. In the case reported by the present paper, the triad of symptoms otorrhea, retrocular pain and abducent nerve paralysis corresponded to Gradenigo's syndrome. It is important to emphasize that petrositis is not a synonym of Gradenigo's syndrome, since the classical syndrome is not common.
The most popular imaging technique is computed tomography, but simple x-ray can also bring a lot of information to the case.
Treatment of petrositis is antibiotic therapy and/or surgery. The acute form may be treated clinically, with or without simple mastoidectomy, if the infection is restricted to aired cells. If there is further compromise of the temporal bone, a more aggressive surgical approach is necessary to allow good drainage of secretion. A number of techniques have been described for the complete exerentation of the cells of the petrous apex: translabyrinthic access, or middle fossa access in order to preserve the labyrinth function and hearing, facial nerve and carotid artery.
In view of a case of petrositis, in addition to otitis media, we should consider the following diagnoses: sphenoid sinusitis, mastoiditis, infectious labyrinthitis, congenital cholesteatoma of the petrous portion, neoplasia, cavernous sinus thrombosis, fractures, hematomas and aneurysms.
The radiological analysis of the patient reported here showed sphenoid sinusitis and signs of cavernous sinus thrombosis. We can think of two possibilities for the development of abducent nerve paralysis:
1. Extension of the infectious process from the middle ear into the petrous apex;
2. Sphenoid sinusitis leading to upper orbital fissure syndrome or to cavernous sinus thrombosis. Both can progress to abducent nerve paralysis.
Despite the existence of cavernous sinus thrombosis, the patient presented good general health and responded well to clinical treatment, leading us to choose conservative treatment.
We should always face otitis media as a potentially severe disease owing to its serious complications. In view of a patient with otitis media and ocular or temporal-parietal pain, or a patient that has undergone surgery and still presents otorrhea, we should always consider the possibility of complicated otitis media.
It is essential that pediatricians, general practitioners and otorhinolaryngologists are attentive to diagnose complications of otitis media, because although incidence has decreased, morbidity and mortality are still high.
REFERENCES
1. Kafka MM - Mortality of mastoiditis and cerebral complications with review of 3225 cases of mastoiditis with complications. Laryngoscope, 1935;45:790-822.
2. Profant HJ. - Gradenigo's Syndrome. With a consideration of petrositis. Arch. Otolaryngol., 1931;13:347-76.
3. Kangsanarak J, Fooanant S, Ruckphaopunt K, Navacharoen N, Teotrakul S. Extracranial and intracranial complications of suppurative otitis media. Report of 102 cases. J. Laryngol. Otol., 1993;107:999-1004.
4. Goycoolea MV, Jung TTK. In Paparela MM, Shumrick DA, Gluckman JL, Meyerhoff WL. 3ª edição, Filadélfia. W.B. Saunders, 1991;1381-92.
5. Albers FWJ. Complications of otitis media. The importance of early recognition. Am. J. Otol., 1999;20:9-12.
6. Farrior J. Complication of otitis media in children. South. Med. J., 1990;83:645-8.
7. Glasscock ME. Chronic petrositis. Diagnosis and treatment. Ann. Otol. Rhinol. Laryngol., 1972;81:677-84.
8. Chole R, Donald PJ. Petrous apicitis. Clinical considerations. Ann. Otol. Rhinol. Laryngol., 1983;92:544-51.
1 Master degree, Discipline of Pediatric Otorhinolaryngology, Federal University of São Paulo, UNIFESP-EPM.
2 Full Professor, Head of the Discipline of Pediatric Otorhinolaryngology, UNIFESP-EPM.
Discipline of Pediatric Otorhinolaryngology, Department of Otorhinolaryngology and Human Communication Disorders, UNIFESP-EPM.
Address correspondence to: Rua dos Otonis, nº 684, V. Clementino - 04025-001 - São Paulo - SP
Tel/fax: (55 11) 5576-4395 - E-mail: beaneves@terra.com.br
Study presented at the 12a Reunião da Sociedade Brasileira de Otologia, held in November 1997 in Rio de Janeiro.
Article submitted on August 23, 2001. Article accepted on October 29, 2001
All rights reserved - 1933 /
2025
© - Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico Facial