Year: 2010 Vol. 76 Ed. 1 - (22º)
Relato de Caso
Pages: 136 to 136
Chronic sialadenitis caused by sarcoidosis: A Case Report
Author(s): Jose Castro Lima Geraldes Filho1, Helenimarie Schaer Barbosa2, Delano O. Souza3, Alisio A. Prates4
Keywords: submandibular gland, granulomatous, sarcoidosis.
![]()
INTRODUCTION
Sarcoidosis is a systemic granulomatous, non-infectious multifocal disorder of unknown etiology, characterized by the presence of non-caseous epithelioid granuloma in the tissue1,2. About 20 to 40% of the patients are symptom-free and their disease is found through routine radiographic tests1. The hypothetical causal agents include environmental and autoantigen aspects1,3. The goal is to report a rare case4 of chronic sialoadenitis having sarcoidosis as the cause.
CASE REPORT
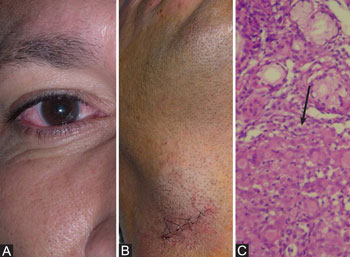
Male patient, 41 years old, had a face swelling, reduced salivation, red eyes and dysphagia for months. He had a uniform and bilateral enlargement of the parotid and submandibular gland (Fig. B) - painless, firm, smooth and mobile; with hyperemia of the ocular conjunctiva (Fig. A). During routine exams, the chest x-ray showed an image suggesting the presence of a peribronchovascular infiltrate, without clinical significance. The patient was referred to incisional biopsy of the right submandibular gland and smaller salivary gland of the lower lip. Histopathology reported Chronic Granulomatous Sialoadenitis, a matching diagnosis of sarcoidosis. The patient returned to the ward with a history of past use of non-hormonal anti-inflammatory agent (without medical instruction), with total remission of signs and symptoms.
Figure 1. Sarcoidosis - Figure A- conjunctiva hyperemia; Figure B - biopsied mandibular hypertrophy; Figure C - salivary gland with granulomas made up of epithelioid cells and multinucleated gigantic cells (arrow).
DISCUSSION
Sarcoidosis is usually acute in onset, with more common clinical symptoms of dyspnea, dry cough, chest pain, fever, malaise, fatigue, arthralgia and weight loss1 and, about 20% of the patients are assymptomatic1. The lungs, lymph nodes, skin, eyes and salivary glands are the most affected organs1,2. Skin lesions such as plaques and nodules, nasal mucosa and liver granulomas may also be present2.
The lymphoid tissue is affected in almost all the cases and the salivary gland swelling, xerostomia and eye involvement may combine and mirror Sjögren Syndrome6, which led us to do the lower lip salivary gland biopsy.
The respiratory system is usually the one most involved, and 90% of the patients have an abnormal chest x-ray1,5,3. The most common symptoms are dyspnea, fever, fatigue and dry cough1,2, which did not happen to our patient.
Eye lesions are seen in approximately 25%1. Inflammation on the anterior uveal interval is the most common eye lesion. The patients complain of visual alteration and photophobia. The lesions are chronic and can progress to blindness1,2.
It rarely involves the oral cavity, more frequently appearing as an isolate submucosal mass or area of granularity1,6. The facial is the most affected cranial nerve and it can also involve the inferior alveolar nerve1. Our patient complained of dysphagia; however, we believe it was a symptom related to reduced salivation.
Histopathology helps in the diagnosis, which was fundamental in our case. There were no morphological aspects suggesting Miculicz/Sjögren syndrome diseases and both fungi (Grocott) and mycobacterium (Ziehl-Neelsen) tests turned out negative. In figure C we notice granulomas made up of epithelioid and gigantic multinucleated cells.
Diagnosis is based on clinical history, radiographic characteristics, histological evidence and ruling out other diseases capable of producing similar clinical or histological manifestations1. Some laboratorial abnormalities such as hypercalcemia and hypercalcinuria may be present. The serum levels of the Angiogenesis Converting Enzyme may be elevated in 60% and, are useful in monitoring disease development and remission. A skin test for sarcoidosis, the Kveim test can be performed1,2; however, it is rarely used.
A 3 to 12 months observation period is usually recommended to establish disease course1,6. Treatment is usually indicated for severe eye involvement; symptomatic lungs; neurological, renal, cardiac and skin manifestations which affect the face and cause spleen enlargement1,6. The treatment of choice for sarcoidosis is steroids.
We believe that the use of nonhormonal anti-inflammatory agents by our patient for less than ten days are not the cause for disease remission, but rather a spontaneous resolution.
FINAL REMARKS
Histopathological test, radiographic tests and clinical manifestations are fundamental for the diagnosis. Treatment is based on steroids or observation only.
REFERENCES
1. Batal H, Chou LL, Cottrell DA. Sarcoidosis: medical and dental implications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88(4):386-90.
2. Júnior HLA, Jannke HÁ. Sarcoidose em cicatrizes prévias. An Bras Dermatol. 2004;79(1):79-82.
3. Fortuna FP, Fischer GB. Sarcoidose pediátrica: relato de caso. J Pneumol. 2000;26(5):259-62.
4. Lobo LM, Donadussi M, Nakata TS, Gonçalves MCF, Caldana G. Sarcoidose cutânea:relato de caso. Rev Méd HSE Med. 2001 Jul;35(3-4):tema oral nº 13.
5. Fatahzadeh JR. Diagnosis of systemic sarcoidosis based on oral manifestations. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97(4):457.
6. Souza PRM, Duquia RP, Vetoratto G, Júnior HLA:Lesões sobre cicatrizes, uma das manifestações da sarcoidose. J Bras Pneumol. 2004;30(6):585-7.
1. ENT Specialist - Hosp. Santa Casa/SSA-BA. MSc in Head and Neck Surgery - Hospital Heliópolis-SP, Assistant Physician - Head and Neck Department - Hospital Aristides Maltez-SSA/BA.
2. Adjunct Professor - Federal University of Bahia Medical School - UFBA, Assistant Physician - Pathology Department - Hospital Aristides Maltez SSA/BA.
3. Resident physician in traumatology and maxillofacial surgery - Hospital Santo Antonio-SSA/BA.
4. Dentistry student - UFBA.
Serviço de Cirurgia de Cabeça e Pescoço do Hospital Aristides Maltez.
Send correspondence to:
José Castro Lima Geraldes Filho
R. Agnelo de Brito 90 4°andar ED. Garibalde Memorial - Garibaldi
Paper submitted to the BJORL- SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on July 19, 2007;
and accepted on March 20, 2008. cod. 4674 Braz J Otorhinolaryngol.
All rights reserved - 1933 /
2025
© - Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico Facial