Year: 2003 Vol. 69 Ed. 1 - (9º)
Artigo Original
Pages: 48 to 52
Endoscopic ligature of the sphenopalatine artery for severe posterior epistaxis
Author(s):
Richard L. Voegels,
Daniela C. Thomé,
Patsy Priscilla V. Iturralde,
Ossamu Butugan
Keywords: epixtasis, endoscopic ligature of the sphenopalatine artery, treatment.
Abstract:
Objective: To present our experience with endoscopic ligature of the sphenopalatine artery in the treatment of severe posterior epistaxis. Methods: During a 56 month-period, 31 patients with severe posterior epistaxis, who were treated using na endoscopic ligature of the sphenopalatine artery were reviewed. Results: Nineteen (61,3%) patients were male and 12 (38,7%) female, with ages ranging from 15 to 80 years, with an average age of 44,7 years. The endoscopic ligature of the sphenopalatine artery was performed unilaterally in 29 patients and bilaterally in 2 cases, with a total of 33 ligatures. It was possible to identify the sphenopalatine artery in all cases with successful outcome using this surgical technique alone. Conclusions: Endonasal endoscopic ligature of the sphenopalatine artery has been an effective and safe surgical technique for treating severe posterior epistaxis.
![]()
Introduction
Severe epistaxis, in general coming from the posterior nasal fossa region, is one of the main emergencies in Otorhinolaryngology and requires special care1. Surgical treatment of epistaxis, involving cauterization via microscopy or endoscopy, arterial ligature and embolization, is normally reserved to patients that present refractory bleeding to conservative maneuvers1, 2. However, depending on the severity of the picture, the surgical approach can be the first option of treatment.
Sphenopalatine artery ligature through microsurgery was introduced by Prades3 in 1970. Sulsenti et al.4, in 1987, used the Prades' bivalve speculum and the microscope to proceed the sphenopalatine artery ligature in the middle fossa, whereas Budrovich and Saetti5, in 1992, were the first ones to report the use of the endoscope to conduct the procedure. The objective of the ligature is to interrupt the nasal irrigation in a point distal enough to prevent direct, retrograde and anastomotic flow of the ipsilateral and contralateral carotid systems and represents an excellent surgical option to handle posterior severe epistaxis.
The present study aimed at presenting the experience of the Department of Otorhinolaryngology, HC-FMUSP, in sphenopalatine artery ligature via endonasal endoscopic access in severe posterior epistaxis management.
MATERIAL AND METHOD
We conducted a retrospective study in patients submitted to sphenopalatine artery ligature via endoscopic endonasal access in the Department of Otorhinolaryngology, HC-FMUSP in the period of November 1996 to July 2001 (56 months). The ligature was conducted in a total of 31 patients, 19 (61.3%) were male and 12 (38.7%) were female subjects, ages ranging from 15 to 80 years (mean age of 44.7 years). All patients were submitted, before surgery, to conservative treatment with no success (anterior packing and/or anterior-posterior packing). Through review of medical charts, we collected information about the possible predisposing factors.
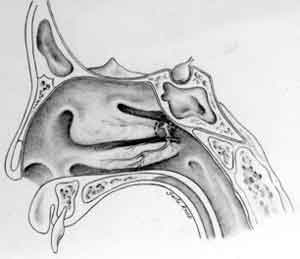
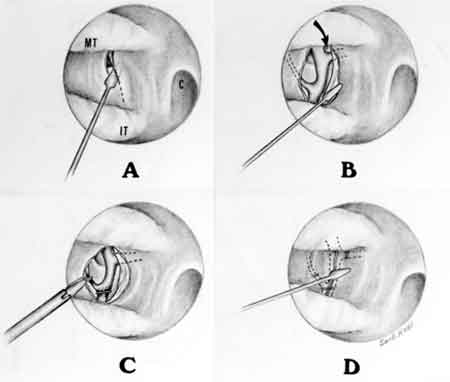
All surgeries were conducted under general anesthesia, with no specific care for blood pressure (patients were kept with normal blood pressure). Topical vasoconstriction was made with cotton balls soaked in adrenaline 1:2000, with no use of infiltration. The basic principle of the surgical technique, which involved the use of rigid nasal endoscope at zero degree and 4mm diameter, consisted of the identification of the branches of the sphenopalatine artery (Figure 1). We made a vertical incision inferior to the posterior portion of the middle turbinate, 1cm anterior to the most posterior region (Figure 2 A). By elevating a posterior and superior mucoperiosteal flap, the fibroneurovascular bundle was reached at the sphenopalatine foramen (Figure 2B). After isolating the artery and the branches, we placed vascular clips (Titanium Clip, Ethicon Endo-Surgery; INC; REF:LT200) under direct visualization (Figure 2 C) and the mucoperiosteal flap resumed its original position (Figure 2D).
Figure 1. View of the lateral wall of the nasal fossa that shows the relation of the sphenopalatine foramen with the middle turbinate and the branches of the sphenopalatine artery.
Figure 2. A. incision vertical to the posterior portion of the middle turbinate; B. elevation of a posterior and superior mucoperiosteal flap, reaching the sphenopalatine artery at the level of the sphenopalatine foramen; C. application of vascular clips under direct view; D. return of the mucoperiosteal flap to its original position (MT: middle turbinate; IT: inferior turbinate; C: choana; arrow: indicates the sphenopalatine foramen).
Results
Sixteen (51.6%) of the patients were submitted to anterior-posterior packing, conducted with foley probe posteriorly and Vaseline rayon anteriorly, and all patients had been previously treated with anterior packing. Endoscopic electrical cauterization of bleeding points was conducted in 6 subjects (19.3%). Blood transfusion was necessary in 6 patients (19.3%).
Sphenopalatine artery ligature via endonasal endoscopy was conducted unilaterally in 29 cases (93.5%) and bilaterally in 2 subjects (6.4%), amounting to a total of 33 ligatures. The identification of the branches of the sphenopalatine artery was possible in all cases, and we reached therapeutic success with the isolated technique. No patients required postoperative nasal packing. There were no complications during or after the surgery related to the procedure. The patients were discharged after 48 hours or more of observation.
Table 1. Characteristics and predisposing factors of the studied patients.
Table 2. Treatment conducted previously to sphenopalatine artery ligation and need for blood transfusion.
Table 3. Sphenopalatine artery ligation via endoscopic endonasal access.
Discussion
Physicians are increasingly considering early vascular ligature as an alternative for some patients that have severe posterior epistaxis. This fact is due to the possibility of providing more comfort to the patient, reducing hospitalization rate and the need for blood transfusion, and reducing morbidity and even mortality. Some indications for vascular ligature, similarly to those indicated for endoscopic cauterization made by O'Leary-Stickney et al.7 are: a) blood dyscrasia that contraindicates packing or open surgery; b) refractory bleeding with packing already in place; c) hemorrhage after nasal surgery, and d) patient's intolerance to packing.
Surgical treatment for severe epistaxis is also associated with different predisposing factors. In our study, hypertension, hematological disorders and trauma were present in 16 (51.6%), 1 (3.2%) and 4 (12.9%) patients, respectively. Epistaxis secondary to inferior turbinectomy was observed in 11 cases (35.4%). In addition, Barlow et al.1 observed that the surgical treatment for severe epistaxis was strongly associated with posterior bleeding and blood transfusion. In this study, all patients presented posterior epistaxis, but only 19.3% needed blood transfusion.
Endoscopic sphenopalatine artery ligature has proven to be an effective surgical technique in the treatment of severe posterior epistaxis, as observed in our first study9.
In 1992, Budrovich et al.5 described some difficulties in isolating the artery, but they did not observe complications. However, as a result of the increase in the experience with endoscopic surgery and anatomical parameters, no difficulty was found in isolating the artery in our study. We believe that this surgical technique is simple, promotes good exposure of the surgical field, presents low morbidity and should be considered early in handling severe posterior epistaxis.
References
1. Barlow DW, Deleyiannis FWB, Pinczower EF. Effectiveness of surgical management of epistaxis at a tertiary care center. Laryngoscope 107;21-24, 1997.
2. Sharp HR, Rowe-Jones JM, Biring GS et al. Endoscopic ligation or diametry of the sphenopalatine artery in persistent epistaxis. J Laryngol Otol 111:1047-1050, 1997.
3. Prades J. Abord endonasal de la fosse pterygo-maxillaire. LXXIII Cong Franc Compt Rendus des Seanc 290-296, 1976.
4. Sulsenyi G, Yanez C, Kadiri M. Recurrent epistaxis: microscopic endonasal clipping of the sphenopalatine artery. Rhinology 25:141-142, 1987.
5. Budrovich M, Saetti R. Microscopic and endoscopic ligature of the sphenopalatine artery. Laryngoscope 1390-1394, 1992.
6. Simpson GT, Janfaza P, Becker GD. Transantral sphenopalatine artery ligation. Laryngoscope 1001-1005, 1982.
7. O'Leary-Stickney K, Makielsky K, Weymuller EA. Rigid endoscopy for the control of epistaxis. Arch Otolaryngol Head Neck Surg 118:966-967, 1992.
8. White PS. Endoscopic ligation of the sphenopalatine artery (ELSA): a preliminary description. J Laryngol Otol 110:27-30, 1996.
9. Voegels RV, Thomé DC, Iturralde PPV, Butugan O. Endoscopic ligature of the sphenopalatine artery for severe posterior epistaxis. Otolaryngol Head Neck Surg 124 (4):464-467, 2001.
1 Ph.D., Professor, Department of Otorhinolaryngology, Medical School, University of São Paulo, Director of Rhinology,
Department of Otorhinolaryngology, Hospital das Clinicas, Medical School, University of São Paulo.
2 Doctorate studies under course, Department of Otorhinolaryngology, Medical School, University of São Paulo.
3 Otorhinolaryngologist, graduate from the Department of Otorhinolaryngology, Medical School, University of São Paulo.
4 Associated Professor, Department of Otorhinolaryngology, Medical School, University of São Paulo.
Address correspondence to: Richard Louis Voegels - Rua Iubatinga 145 ap 61-B São Paulo SP 05716-110 - Fax: (55 11) 3749-1029 - E-mail: voegels@attglobal.net
Article submitted on June 01, 2001. Article accepted on September 19, 2002.