Year: 2002 Vol. 68 Ed. 1 - (11º)
Artigo Original
Pages: 65 to 68
Eyelid gold weight for treatment of lagophthalmus in patients with facial palsy
Author(s):
José Ricardo Gurgel Testa 1,
Mariana Dantas Aumond 2,
Cláudia Regina Figueiredo 3
Keywords: gold weight implant, lagophthalmus, facial palsy.
Abstract:
Introduction: Lagophthalmus in facial palsy must be treated in order to avoid ocular complications. The gold weight eyelid implant as an alternative to tarsorrhaphy has been studied with good results. Aim: The purpose of this report is to study the effects of the gold weight eyelid implants for treatment of lagophthalmus. Study design: clinical retrospective not randomized. Material and method: 59 patients with Lagophthalmus associated with facial paralysis of many causes underwent gold weight implantation and were studied retrospectively. Results: All patients achieved satisfactory eyelid closure and improvement of ocular symptoms. 8.5% of patients had implant extrusion and 5% had infection. The average time with the implant varied from 6 months to 6 years, being removed in 20.3% of patients with recover of facial palsy. Discussion: Many methods have been described for enhance corneal protection in patients with facial palsy with different degrees of success and acceptance by the patient. The gold weight eyelid loading is a simple easy technique with good cosmetic result. The average time with the implant is inconstant and the complications are rare. Conclusion: Gold weight eyelid implants in patients with facial palsy have good results for the treatment of lagophthalmus and prevention of ocular complications.
![]()
1 Professor, Discipline of Pediatric Otorhinolaryngology, Federal University of São Paulo-Escola Paulista de Medicina.(UNIFESP-EPM).
2 Resident physician in Otorhinolaryngology, Federal University of São Paulo-Escola Paulista de Medicina.(UNIFESP-EPM).
3 Doctorate studies under course, Discipline of Otorhinolaryngology, Federal University of São Paulo-Escola Paulista de Medicina.(UNIFESP-EPM).
Study conducted at the Discipline of Otorhinolaryngology, Federal University of São Paulo-Escola Paulista de Medicina.(UNIFESP-EPM)/ Department of Head and Neck Surgery, Hospital do Câncer de São Paulo.
Paper presented as free communication at II Congresso Triológico de Otorrinolaringologia, August 22 - 26, 2001, in Goiânia-GO.
Address correspondence to: Mariana Dantas Aumond - Av. Higienópolis, 1048, apto 126 - 01238-000 São Paulo, SP - Tel: (55 11) 38223037- Fax: (55 11) 38223398 - E-mail: marklebl@hotmail.com
Article submitted on September 13, 2001. Article accepted on October 29, 2001.
Introduction
Lagophthalmus is defined as an inability to close the eye and it is present in patients with peripheral facial palsy. As complications, there is drying of the conjunctival mucosa with the consequent corneal-conjunctival inflammatory process. In order to avoid such complication, we may use clinical methods, such as ophthalmic lubricating ointments and eye drops, and surgical methods such as tarsorrhaphy, canthoplasty, silicone prostheses, muscle transposition and springs and eyelid weight implants.
For a long time, tarsorrhaphy was the classically described method to treat and prevent keratitis by exposure and corneal ulcer. The use of gold implants as an alternative to tarsorrhaphy was primarily suggested by Smellie in 1966 (12) and by Barclay et al. in 19691. Jobe improved the technique and reported his results in 19744. May em 1987 reported 91% of success with 94 gold weight implants8.
The purpose of the present paper was to study the effects of the implantation of upper eyelid gold weight to correct lagophthalmus.
Material and Method
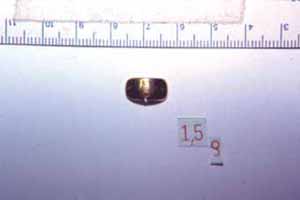
We studied retrospectively 59 patients with lagophthalmus secondary to facial palsy of different etiologies who were submitted to placement of 24 karat gold weight implants (1 to 1.5g) in the upper eyelid (Figure 1). Patients were followed in the ambulatory of facial nerve disorders of the Department of Otorhinolaryngology at UNIFESP and in the Head and Neck Surgery sector of Hospital do Câncer de São Paulo, between 1994 and 2000.
The placement of gold was conducted under local anesthesia in most cases and under general anesthesia when concomitantly performed with other surgeries. After upper eyelid infiltration with 2% xylocaine, we performed an incision of 1.5cm to place the gold weight in juxtatarsal position and centered over the pupil, fixed with separated mononylon 6.0 stitches and intradermal incision suture with mononylon 6.0.
Patients were assessed concerning epidemiological distribution, etiology of facial paralysis, functional result, complications and time with the implant.
Results
Age of patients varied from 22 to 79 years (mean age of 50.4 years), with 31 male patients and 28 female patients. Etiologies of facial paralysis are listed in Table 1.
All patients managed to close completely the eye (Figures 2 and 3) and all of them referred improvement of ocular symptoms, such as ardor, hyperemia, and foreign body sensation.
Complications occurred in 5 patients (8.5%), characterized by extrusion of the weight. Three of the patients presented associated surgical wound infection (5%).
The time with the implant ranged from 6 months to 6 years, being removed in 13 patients (20.3%) after recovery of peripheral facial palsy. In 6 patients (10.2%), the weight remained until the patients died.Table 1. Number of patients with different etiologies of facial palsy.Figure 1. Eyelid gold weight implant.Figure 2. Patient with lagophthalmus secondary to facial palsy.Figure 3. Patient submitted to placement of eyelid gold weight implant.
Discussion
Treatment of facial palsy should include measures that promote appropriate eyelid closure in order to prevent ocular complications that could lead to blindness.
Although all patients who have lagophthalmus secondary to facial palsy are potential candidates for eyelid surgical correction, there is no consensus on the literature concerning its indication. Catalano et al.2 proposed that the surgical correction be performed in patients with grades 1 and 2 of facial paralysis (classification by House Brademann), associated to simultaneous impairment of the 4th and 5th cranial nerve owing to the presence of corneal anesthesia and absence of Bell's phenomenon; in patients with grades 3 and 4 with electrical tests without evidence of reinnervation, and in all patients grades 5 and 6. To May8, the only absolute surgical indication is the presence of keratitis even when appropriate corneal lubrication measures (use of ophthalmic ointments and eye drops) are adopted. The most sensitive test for diagnosis of corneal lesion is the fluorescein test7.
Other indications described for early surgical intervention include section of the facial nerve and monocular vision7.
Many methods have been used to promote ocular protection in cases of facial paralysis with variable degrees of success and acceptance by the patient. Among them, we can cite placement of upper eyelid gold weight, tarsorrhaphy, canthoplasty, silicone prosthesis, muscle transposition, spring implants and transposition of temporal muscle11.
Ideally, any method used to correct lagophthalmus secondary to facial paralysis should include: appropriate corneal protection, esthetical acceptance, absence of visual disorders, low rate of complications, promote facial symmetry, have possibility of reversing the procedure in case of spontaneous improvement of facial paralysis, and be technically easy and reproducible.
Tarsorrhaphy is the classically described method to provide corneal protection in cases of facial paralysis. However, tarsorrhaphy has some inconvenient, such as unsatisfactory esthetical result, possible limitation of the visual field and formation of cysts along the eyelid margin when tarsorrhaphy is reverted7, 8, 9.
The gold weight implant in the upper eyelid promotes the ocular closure by the force of gravity, relaxing the eyelid elevator muscle. It is a simple method, easy to revert, with low rate of complications and good esthetical results5. Ocular closure during sleep may be adequately obtained with a slight elevation of the head and the use of a pillow. Other described methods for correction of lagophthalmus secondary to facial paralysis are technically more complexes and the only contraindication for the eyelid weight implant is the presence of glaucoma7. However, if it is an old and well controlled glaucoma, a low-weight gold implant may be considered after ophthalmic consultation2.
The gold weight implant is usually combined with other procedures to correct hypotonic lower eyelid and ectropium, such as resection of the lateral portion of the lower eyelid, canthoplasty and cartilage implant8, 11.
Gold remains as the preferred material for eyelid implants owing to its high density, low rate of reaction and color, which results in good cosmetic outcome1. Platinum weights can be used in patients allergic to gold3.
Facial paralysis improvement is multifactorial, but it is primarily influenced by the cause of the paralysis, degree of neural lesion, age and clinical conditions of patients. The time with an eyelid weight implant is variable in the literature. Linder, Pike and Linstrom7, in a study with 45 patients, had weight removal rate of 31% in 5 years, with a mean time with the implant of 11 months, ranging from 4 to 32 months. Catalano et al.7, in a study with 60 patients, had implant removal rate of 6.7% in 3 years, with mean time with the implant of 9.5 months. In our study, the time with the weight implant ranged from 6 months to 6 years and it was removed in 13 patients (20.3%).
Complications of the procedure are rare and include mobilization and extrusion of the implant, infection, ptosis, unsatisfactory esthetical result, but they may be minimized by appropriate preoperative assessment, determining the right amount of weight and the suitable surgical technique. Rare complications, such as monocular diplopia, astigmatism, and residual lagophthalmus are also described3.
The rate of weight extrusion ranged in the literature from 0%8 to 10%10. High extrusion rates are found in studies that used insertion of lateral weight into the eyelid, without tarsal fixation6. Linder, Pike and Linstrom7 obtained an infection rate of 6.6%. In our study, complications were detected in 5 patients (8.5%) and they were caused by extrusion of the weight. Three of the patients presented associated infection of the surgical wound (5% of the total number of patients).
Conclusion
The use of gold weight eyelid implant to correct lagophthalmus in patients with facial paralysis is a simple, reversible method, with low complication rates and good results concerning ocular closure and prevention of ocular complications.
References
1. Barclay, T.; Roberts, A. - Restoration of movement to the upper lid in facial palsy. Br J Plast Surg., 22:257, 1969.
2. Catalano, P.J.; Bergstein, M.J.; Biller, H.F. - Comprehensive management of the eye in facial paralysis. Arch Otolaryngol Head Neck Surg., 121(1):81-6, 1995.
3. Dinces, E.A. et al - Complications of gold weight eyelid implants for treatment of fifth and seventh nerve paralysis. The Laryngoscope, 107:1617-22, 1997.
4. Jobe, R. - A technique for lid-loading in the management of lagophthalmus in facial palsy. Plast Reconstr Surg.; 53:29-31, 1974.
5. Kartush, J.M. et al. - Early gold weight eyelid implantation for facial paralysis. Otolaryngol Head Neck Surg., 103(6):1016-23, 1990.
6. Kelly, S.A.; Sharpe, D.T. - Gold eyelid weights in patients with facial palsy: a patient review. Plast Reconstr Surg. 89:436-440, 1992.
7. Linder, T.E.; Pike, V.E.; Linstrom, C.J. - Early eyelid rehabilitation in facial nerve paralysis. The Laryngoscope, 106:1115-8, 1996.
8. May, M. - Gold Weight and wire spring implants as alternatives to tarsorrhaphy. Arch Otolaryngol Head Neck Surg., 113(6):656-60, 1987.
9. May, M. - Surgical rehabilitation of facial palsy. In: May, M., ed. The facial nerve. New York: Thieme Stratton, 1986: 695-780.
10. Pickford, M.A.; Scamp, T., Harrison, D.H. - Morbidity after gold weight insertion into the upper eyelid in facial palsy. Br J Plast Surg., 45:460-4, 1992.
11. Sobol, S.M.; Alward, P.D. - Early gold weight lid implant for rehabilitation of faulty eyelid closure with facial paralysis: an alternative to tarsorrhaphy. Head Neck., 12(2):149-53, 1990.
12. Smellie, G.D. - Restoration of blinking reflex in facial palsy by a simple lid-load operation. Br J Plast Surg. 19:279-83, 1966.