Year: 2004 Vol. 70 Ed. 4 - (20º)
Relato de Caso
Pages: 565 to 568
Condyloma of the tongue: a case report
Author(s):
Therezita M. P. P. G. Castro1,
Maria Luisa Duarte2
Keywords: Key words: condyloma in the tongue, HPV, oral cavity.
Abstract:
The acuminated condyloma is a sexually transmissible disease caused by the Papilomavirus (HPV). It is frequently found in the anus-genital region and rare in the mouth cavity. However, the increase of the oral-sexual activity has even more favored the occurrence of the HPV in the oral mucous. This report describes a condyloma in the oral cavity of a 35-year old man with a history of oral sex practice, which diagnostic was confirmed by a biopsy. The treatment for his case was clinical through the use of TCA (trichloro acetic acid, at 80%) with a total restoration of the lesion. A literature review was carried out on the incidence, clinical, diagnosis, treatment, and prophylaxis of the disease.
![]()
Introduction
HPV is an acronym for Human Papillomavirus, which causes condyloma acuminatum (in Greek kondilus, a circular tumor; in latin acuminare, i.e., to become pointed), also known as "rooster crest" or "genital wart".1,2 They are small non-enveloped epitheliotropic viruses, with double circular DNA and from the Papovaviridae family. They may be responsible for sub-clinical disease and be associated with pre-malignant lesions, as well as with certain intraepithelial neoplasias.2,3 They present approximately 55 nm in diameter and 8,000-pair base genome with molecular weight of 5.2 x 106 daltons; the capsideum has 72 capsomers of icosahedric structures.2,3
More than 90 different types of HPV have been identified and are responsible for both benign and malignant lesions. Out of that total, nearly 50% infect the anus-genital tract; among those, are the types considered of high oncogenic risk.2,3
Currently, HPV genital infection is the most frequent sexually transmitted viral disease (STD) among the sexually active population. In 1996, the CDC (Center for Disease Control and Prevention) had estimated the rise of 500 thousand up to 1 million new cases of HPV infections per year. On that occasion, HPV rates were second only to those of Chlamydia infection (4 million) and Tricomoniasis (3 million).1,4
Suskind et al., 1996, have confirmed that anus-genital condyloma was more frequent in sexually active young men than in women; they have also reported 50% higher risk of oral condyloma among patients with anus-genital condyloma and oral sex practice habits. More recently, with improvement of Polymerase Chain Reaction (PCR) technique, HPV infections may reveal to be much more frequent.1,5 HPV transmission occurs by contact to genital or perianal skin. In the great majority of cases it occurs by sexual transmittion.1,6 The virus may get installed in different anatomical regions, such as the anus, penis, vagina and vulva, as well as in the oral mucosa, uterine colon and epithelial tissue.1,6 In the oral cavity, the viral transmission process is still not clear, considering that it occurs through self-inoculation and oral sex practices.7,8 In this region, the tongue is the most frequent area affected by HPV, with 55% incidence as reported by Premoli de Percoco and Christensen in 1992. Other sites in the mouth are the palate, oral mucosa, gingiva, lips, tonsils, uvula and floor of the mouth. This latter is where much saliva is concentrated and in which cancerous agents - such as alcohol and tobacco - are dissolved, allowing viral deleterious action to occur.2
Incubation period of condyloma acuminatum ranges from 2 to 8 weeks and it is related to the individual's immunity level. Evolution from the incubation phase to active expression depends on 3 factors: cellular permissiveness, virus type and the host immunity status.1
Early sexual activity associated with a great number of sexual partners and added to tobacco use, oral contraceptives and other sexually transmitted diseases are factors that highly increase the chances of HPV infections.4
The increasing interest in HPV is due to its significant oncogenic role and some studies show the association of HPV with pre-cancerous lesions, carcinomas and other types of neoplasia.2,4
Among various HPVs, types 1, 2,4,6, 11, 13, 16, 18, 30, 31, 32 and 57 were the ones found in the oral cavity, the same types that affect other mucosa and skin. Types 6 and 11 are found in condylomatous lesions; type 16 is the most prevalent in neoplastic lesions; and 18, the most aggressive.2,10,11
Clinically, condyloma acuminatum is expressed as superficial single or multiple lesions, of exophytic growth, papillary, with raised and rosaceous aspect, of isolated or coalescent distribution forming a cauliflower-like mass. Generally, lesions are asymptomatic, sometimes regress spontaneously, and may or may not relapse.1,6,10
Diagnosis of condyloma acuminatum is mainly achieved through clinical manifestation, cytology, colposcopy and biopsy.10 Cytological exam is characterized by minor or major criteria. For major criteria, the following are considered: coilocytes with perinuclear cytoplasmatic halos and nuclear dysplasia; minor criteria include diskeratocytes, metaplasia, macrocytes and binucleation.4,8 Biopsies provide histopathological confirmation and graduation of the lesion. They are effective exams to determine the intraepithelial lesion's nature and distinguish lesions caused by HPV infection from those of other nature. However, these exams cannot determine the type of HPV involved, which may be obtained only through molecular biology techniques, such as in situ hybridization, hybrid capture and PCR (Polymerase Chain Reaction) -expensive exams and, therefore, not accessible.3,10 Differential diagnosis should be performed with other causes of papular lesions, such as: contagious mollusk, seborrheic keratosis, lichen planus and squamous cell cancer.1,10
Treatment may be clinical or surgical - in which the visible lesion is removed - given that there is no effective treatment for definitive eradication of HPV. Recurrence may occur in previously treated areas, or in other sites, in 20-30% of the cases.12 On the other hand, spontaneous resolution may be observed within one year (20-30% in 3 months and 60% in one year). For clinical treatment, caustic agents are used, leading to tissue destruction; 50-80% solution of trichloroacetic acid (TCA) is the most frequently used, which is applied once a week on the lesion, for 4 weeks. Another agent is 25% podophylin in alcohol solution or 0.5% gel applied to the lesion 2 to 3 times a week. There are also antiblastic agents, such as 5-fluoracil , which is so effective as other agents, although its use is restricted due to high cost and skin intolerance (extreme irritation). Surgery consists of surgical, electrical or laser excision and may be used on lesions with the benefit of preserving the sample for clinical pathology study. Alternative methods include electrocauterization or cryotherapy, although this may be painful in cases of extensive lesions or those found in much innervated sites, such as vulva, vagina or perineo.10,12,13
Prophylaxis consists of clinical guidance, when the patient needs to understand that lesion removal does not exclude the permanence of the virus, even in previously treated areas, or in others, so that general hygiene measures in those areas are mandatory, as well as monogamy, use of condoms and periodical clinical examinations. This is the most effective way to prevent HPV transmission.10,12,14
Case Report
Patient N.M.S., male, Caucasian, 35 years old, married, living in Maceió/Alagoas and born in Recife/Pernambuco was admitted to the Ambulatory of Otorhinolaryngology, Hospital José Carneiro, Escola de Ciências Médicas de Alagoas, complaining of a tumor-like lesion on the tongue which had appeared 3 months before. The patient was not being submitted to any type of treatment. Anamnesis revealed that the patient had oral and anal sex practices. He had initiated his sexual life at the age of 14 years and had had more than 20 sexual partners (of both sexes). He also confirmed the use of tobacco and alcoholic beverages. In addition, he had history of STD (herpes and genital condyloma, already treated). He mentioned that he had gone through Elisa test for HIV, with negative result.
Otorhinolaryngological examination through oralpharyngoscopy revealed 3-cm diameter tumor on the posterior portion of the tongue anterior third, with cauliflower-like appearance. The anterior pillars, uvula, tonsils and jugal mucosa were normal. A biopsy of the lesion was performed revealing the diagnosis of condyloma acuminatum. Microscopy showed hyperplastic epithelium with akantosis and papillomatosis at 100x, 400x and 1000x (immersion), respectively; 400x magnification presented coilocytes with perinuclear halos and irregular hyperchromatic nuclei, as well as coilocystic cells with bi-nucleation. Due to the high cost, a molecular biology test was not performed. Clinical treatment was chosen, with application of 80% solution of trichloroacetic acid (TCA) once a week, resulting in full regression of lesion. After one-year follow-up, there has been no lesion recurrence. Prophylaxis consisted of clinical counseling into monogamy, use of condoms and clinical follow-up every six months to search for lesion recurrence. The patient was recommended not to smoke or have alcohol. He was also told that treatment did not guarantee inexistence of the virus, even in the treated areas - the genital, anal or the oral cavity sites.
Discussion
Condyloma acuminatum is a sexually transmitted disease extremely common in the anus-genital region, but rarely found in the mouth. Its transmission to the oral cavity may occur by oral-sexual contact or self-inoculation. This clinical study describes a male patient of 35 years of age who had oral and anal sex practices presenting a condyloma on the tongue.
The condyloma in the oral cavity is most likely to occur in individuals with early initiation of sexual life and oral sex practices, allied with high number of sexual partners, tobacco and alcohol use and other sexually transmitted diseases. The reported patient presented history of early sexual life, several partners, smoking habit and use of alcohol, presenting genital herpes.
A lesion in the oral mucosa is most frequently found on the tongue, but may also occur on the soft palate, uvula, tonsils and floor of the mouth. Its clinical aspect is of single or multiple lesions with exophytic growth, with papillary, raised and rosaceous aspect, forming a cauliflower-like mass. In this case, the patient's lesion was located on the back of tongue's anterior third, with 3 cm diameter and cauliflower-like appearance.
Condyloma acuminatum is diagnosed through clinical exam, cytology and confirmed through biopsy. The biopsy shows the presence of coilocytes with perinuclear cytoplasmatic halos, nuclear dysplasias, diskeratocytes, metaplasias, macrocytes and bi-nucleation. Molecular biology techniques (in situ hybridization, hybrid capture and PCR) are suitable to identify the HPV type, although they are not accessible due to their high cost. In this case, diagnosis was performed by clinical examination and biopsy, which microscopically (100x magnification) revealed a hyperplastic epithelium with akantosis and papillomatosis; 400x magnification presented coilocytes with perinuclear halos and irregular hyperchromatic nuclei (dyskaryotic); and 1000x magnification (immersion) showed the presence of coilocystic cells with bi-nucleation. Due to high cost, a molecular biology test was not carried out.
Clinical or surgical treatment approaches are alternatives and, usually, the choice is an once-a-week application of 50-80% trichloroacetic acid (TCA) until full regression of lesion is reached. For this case, the option was weekly 80%- trichloroacetic acid application on the condyloma until the lesion completely disappeared.
The patient was told that treatment could eliminate the lesion, although the virus could persist in the epithelium after treatment of genital, anal or oral cavity sites. Prophylaxis consisted of clinical counseling into monogamy, the use of condoms, periodical checkups, as well as to avoid smoking or alcohol. He was also instructed to go through clinical follow-up every 6 months.
Closing Remarks
Due to high transmissibility of HPV to different sites, possibility of malignancy, and the social aspects inherent to the disease, it is important to emphasize that infection by this virus in the oral mucosa should be better understood. Few investigations have been conducted over HPV latent state and sub-clinical aspects.
References
1. Carvalho J & Oyakava N. I Consenso Brasileiro de HPV nº1. São Paulo: BG Editora; 2000.
2. Sarruf MBJ & Dias EP. Avaliação Citopatológica da cavidade bucal em pacientes portadores de infecção genital pelo Papilomavírus Humano (HPV). J Bras Doenças Sex Trans 1997; 9(2):4-18.
3. Tavares RR, Passos MRL, Cavalcanti SMB, PinheiroVMS, Rubinstein I. Condiloma genital em homens e soropositividade para HIV. DST. J Bras Doenças Sex Trans 2000; 12(1): 4-27.
4. Alvarenga GC, Sá EMM, Passos MRL, PinheiroVMS. Papilomavírus Humano e carcinogênese no colo do útero. J Bras Doenças Sex Transm 2000; 12(1):28-38.
5. Badaracco G, Venuti A, Acambia G, Mozzetti S, Benedetti Panici P, Mancuso S, Marcante ML. Concurrent HPV infection in oral and genital mucosa. J Oral Patho Med 1998; 27: 130-4.
6. Gross GE & Barrasso R. Atlas do Papilomavirus Humano 2a Edição. Porto Alegre: Editora Artes Médicas Sul Ltda.; 1999.
7. Chappuis JM, Papa BM, Maldonado MS, Consigli JE. Patologia blanca de la mucosa oral. Arch Argent Dermatol 1998; 48: 209-33.
8. Giraldo CP, Simões JK, Filho DR, Tambascia JK, Dias ALV, Pacelo PCC. Avaliação citológica da Orofaringe de Mulheres portadoras de HPV Genital. Rev Bras Ginecol Obstet 1996 out; 18(9): 737-42.
9. Premoli-de-Percoco G, Christensen R. Human Papillomavirus in Oral Verrucal-Papillary Lesions. Pathologica 1992; 84:383-92.
10. Camargos AF, Hugo de Melo V. Ginecologia ambulatorial. Belo Horizonte: Coopamed; 2001: 397-400.
11. Tominaga S, Fukushima K, Nishizaki K, Watanabe S, Masuda Y, Ogura H. Presence of Human Papillomavirus Type 6f in Tonsillar Condyloma Acuminatum and Clinically Normal Tonsillar mucosa. Japanese Journal of Clinical Oncology 1996; 26: 393-7.
12. Tatti SA, Belardi G, Marini MA, Eiriz A, Chase LA, Ojeda J et al. Consenso en la metodología diagnóstica y terapéutica para las verrugas anogenitales. Revista Obstetricia y Ginecologia Latino-Americanas 2001; 59 (3): 117-31.
13. Suskind DL, Mirza N, Risin D, Stanton D, Sachdeva R. Condyloma Acuminatum Presenting as a Base of tongue mass. Otolaryngology Head and Neck Surgery 1996; 114 (3): 487-90.
14. Eluf Neto J, Zeferino LC, Dores GB, Passos MRL. Prevenção da infecção pelo Papilomavírus Humano. DST. J Bras Doenças Sex Trans 2000; 12(1): 39-42.
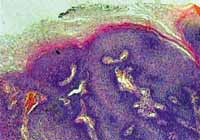
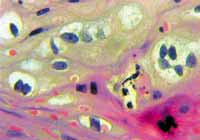
The microscopic examination shows:
Figure 1. 100x-Magnification - Hyperplastic epithelium with akantosis and papillomatosis.
Figure 2. 400x-Magnification - Coilocytes with perinuclear halos and irregular hyperchromatic nuclei (dyskaryotic).
Figure 3. 1000x-Magnification (immersion) - Coilocystic cell with bi-nucleation.