Year: 2004 Vol. 70 Ed. 3 - (18º)
Relato de Caso
Pages: 410 to 414
GelfoamŪ applications as an emergency treatment in glottic insufficiency in singer
Author(s):
Paulo A. L. Pontes 1,
Vanessa P. Vieira 2
Keywords: larynx, insufficiency, implant, GelfoamŪ
Abstract:
GelfoamŪ, a product referred to patients presenting unilateral vocal fold paralysis, was applied to a female singer who showed glottic insufficiency by vocal fold atrophy and who needed urgently to proceed with her professional activities. The product was applied through percutaneous and translumination viae, in clinic, and followed by vocal assessments to confirm the efficacy of the treatment. There were realized two series with one year of interval, both with two applications, respectively 28 and 30 days. The result was positive allowing the patient to return to her activities and to conclude her work during the period that GelfoamŪ, that was in progressive absorption, permitted a glottic coaptation compatible with the necessities of the voice use.
![]()
INTRODUCTION
GelfoamŪ (absorbable gelatin sponge) has been used for many years in Otorhinolaryngology surgeries, especially in Otology, to accommodate tissues and for hemostasis. Recently, it started to be used also for correction of glottic insufficiency in cases of unilateral vocal fold paralysis with or without aspiration 1-3. In these cases, the objective is to have medialization of the paralyzed vocal fold's free margin during the period in which we can still wait for functional recovery. Since it is absorbable material, the expectation is that there is coincidence or closeness between absorption and restart of muscle activity. If absorption is quicker than necessary, we can reapply the product. Based on this experience we thought we could also use it for correcting glottic insufficiencies not from paralysis, but for a short time in which the patients needed more vocal support to respond to demands in their activities.
The purpose of the present study was to show the results obtained with GelfoamŪ to correct glottic insufficiency by structural affections in a singer, when she had to quickly improve her voice.
CASE REPORT
E.C, female, 46-year-old married subject, born and living in Sao Paulo, singer, came to Instituto da Laringe for the first time in 1989, complaining of intermittent hoarseness, throat-clearing, and vocal fatigue for six years. At that time, she had already been submitted to different clinical treatments and voice therapy, referring vocal improvement (but still insufficient for her activity) but not of presence of secretions.
Popular music singer for 20 years, the patient had opera singing classes to better project her voice. She did not report family history, smoking, alcohol abuse, exposure to air conditioning, and bronchial asthma. She presented allergic rhinitis and referred she had been treated with prednisolone. The exam revealed thin vocal folds, slightly bowed, with presence of stria major vocal sulcus superficially and bilaterally, larger on the left, and anterior spindle chink.
The initial treatment was clinical management for allergy and voice therapy, with unstable progression and no laryngoscopic changes up to the beginning of 1993. In vocal therapy, she had exercises for whispering voice, vibration exercises including basal sounds and exercises proposed by Jo Estill method. We also investigated hormonal and digestive aspects, which proved to be within the normal range.
We then decided for surgical procedure, with the possibility of injecting collagen or performing bilateral type I thyroplasty 4; we decided for thyroplasty, which was performed in January 1993. After one month, she presented chondritis, was medicated with antibiotics, which resulted in reduction of inflammatory process and formation of fibrosis on the middle third of the right vocal fold. Despite the complication, there was improvement in vocal quality, and she still had difficulty to produce high frequencies, the most important frequencies for singing voice.
Two months after the surgery, laryngoscopy showed granulomatous reaction on the left vocal fold and we conducted laryngeal microsurgery on the same month to remove the granuloma, when we detected the extrusion of the silicon plate, which was then removed. A small area of the cartilage was exposed on the left, to the anterior commissure of the subglottic region. We also found thin mucosa bridge on the anterior third of the right vocal fold, which was also removed. Four days postoperatively, she already had scarring and voice had good quality, still remaining singing difficulties only, except in high frequencies. She restarted voice therapy and reached marked vocal improvement with reduction of chink and vibration on subglottic aspect of vocal folds. She resumed her singing classes in an attempt to expand vocal range up to falsetto.
In September 1993, she had GelfoamŪ application on the left vocal fold in order to reduce the chink and support vocal therapy. After two months, she could sing without hoarseness, with practically no anterior chink and symmetrical vibration of mucosa vocal folds. Low frequencies were stable but there were some sound breaks in high frequencies. She resumed her professional activities as popular singer. She maintained stable and unrestricted vocal conditions up to May 1995, when she came back for control, reporting excellent improvement in singing, giving performances and singing up to 40 songs in each of them.
She came back again in August 1998, reported panic syndrome and the prescribed medication improved her condition. After 8 months without singing, she resumed her regular activities and started to have difficulties again. Laryngoscopy showed marked increase of chink, mucosa atrophy and salience of the left vocal fold border during abduction. She was instructed to resume singing classes. The cause of atrophy was not determined, since once she resumed her activities, there was vocal improvement.
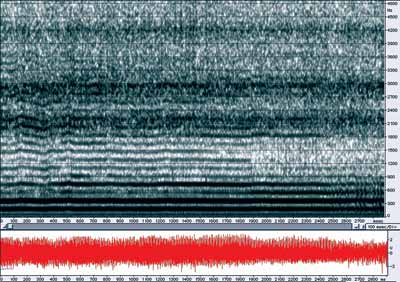
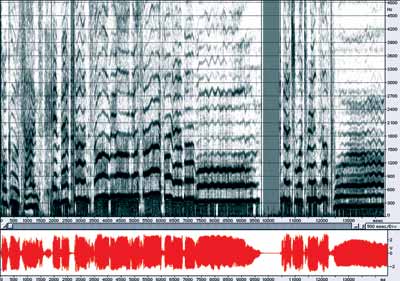
In August 2001, she reported worsening of voice for the past months. The period coincided with the recording of a new album, which was almost completed, but she did not manage to finish it owing to vocal worsening. The test showed fibrosis plate on the anterior commissure and increase in spindle chink (Figure 1). In the visit, we conducted vocal assessment and detected breathy, harsh and tense moderate to severe voice, and mild bitone characteristics, reduced maximum phonation times (7 to 9 seconds), hard vocal attacks, s/z ratio of 1.9, laryngopharyngeal resonance, with laryngeal predominance; low pitch, reduced loudness, modulation with mild restriction, appropriate articulation mode, inappropriate lung-articulation coordination, vocal breaks in high frequencies, mild reduction of harshness and breathiness during singing and modal head register. In the acoustic assessment of sustained vowel /?/ f0 was 184 Hz, unstable acoustic sign at the end of production, breaks and fluctuations of frequency during emission (Figure 2). Spectroscopy in singing voice presented regions of tension, breaks during passage zones, diplophonics, increase in noise in vowels and instability of emission (Figure 3).
She was indicated for GelfoamŪ application on the right vocal fold as emergency treatment to close the glottic chink and reduce vocal deviations.
GelfoamŪ was previously prepared with progressive hydration, using physiological solution up to paste consistency and it was deeply applied on the right vocal fold at the region with spindle chink. The application was made with Brunning syringe and needle 30-8. The introduction of the needle in the vocal fold was made by percutaneous and translumination access, penetrating through the opposite side, at the cricothyroid membrane. The direction and deepness of the needle were monitored under videonasofibroscopy (Figure 4). Anesthetics was topical, in the endolaryngeal region, using Xylocaine spray 10%, and local, with the same product, under injecting form at 2% in the cutaneous region.
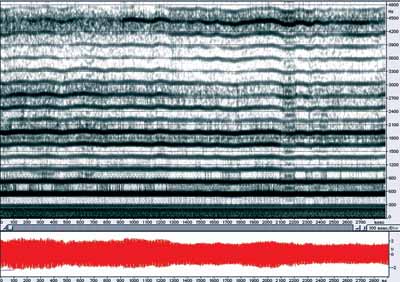
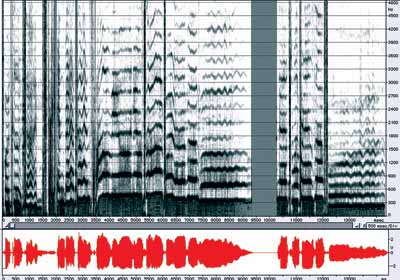
After application of GelfoamŪ (Figure 5) we conducted new perceptual-auditory and acoustic vocal assessment and she had moderate breathy, harsh and tense vocal quality, no more bitone quality, increase in maximum phonation times (13 to 15 seconds), hard vocal attach, high pitch, appropriate loudness and sound breaks only in very high frequencies. During singing, she had marked reduction of breathiness and harshness with clearly production of lower frequencies, but still presenting shorten phonation times in singing voice, managing to produce maximum four words per inspiration. Spectroscopy showed well-defined harmonics with range of 5,400 Hz, no noise between the bands, oscilloscopy with more homogenous configuration and good definition of formant bands (Figure 6). In the spectroscopy, we observed greater vowel stability, noise reduction, no more diplophonics and maintenance of tension using the same sentence she had previously sung five days before the application (Figure 7).
The patient resumed her professional activities and could sing well, without requiring too much from high frequencies. One month and 20 days later, we could see signs of absorption and worsening of vocal quality, which required new application of GelfoamŪ, whose effect remained until the end of the recording, 30 days later.
In December 2000 vocal demand was too intense owing to year-end performances and once again we applied Gelfoam in two 30-day interval steps, allowing continuity of her work.
Figure 1. Laryngeal image before GelfoamŪ application.
Figure 2. Sustained /?/ production before GelfoamŪ application.
Figure 3. Production of sung sentence before GelfoamŪ application.
Figure 4. Laryngeal image with needle during GelfoamŪ application.
Figure 5. Laryngeal image after GelfoamŪ application.
Figure 6. Sustained /?/ production after GelfoamŪ application.
Figure 7. Production of sung sentence after GelfoamŪ application.
DISCUSSION
This case showed that application of GelfoamŪ in mobile vocal folds with minimal structure alterations and associated with postoperative scars allowed correction of glottic insufficiency providing to the patient, in an immediate fashion, vocal quality improvement to perform her professional activities within a period of about 60 days.
The procedure, in addition to this purpose, allows observation of the vocal behavior of the patient, correcting defects by the injection of substances. It was defined that the patient would undergo a new surgery to insert non-absorbable or low absorbable material in order to reach permanent results similar to those obtained with GelfoamŪ.
In this case in particular, the choice of material to be implemented did not depend on viscosity, considering that it can also be applied deeply and maintain the mucosa intact.
Thyroplasty was ruled out, considering the occurrence of adverse reaction when the first procedure was made.
CONCLUSION
The use of GelfoamŪ, in addition to habitual indication for unilateral vocal fold paralysis, proved to be efficient to correct glottic insufficiency by structural alterations in voice professional user, with improvement of vocal performance in the short run.
REFERENCES
1. Anderson TD, Mirza N. Immediate Percutaneous Medialization for acute vocal fold immobility with aspiration. Laryngoscope 2001; 111:1318-21.
2. Morpeth JF, Willians MF. Vocal fold Paralysis after anterior cervical diskectomy and fusion. Laryngoscope 2000; 110:43-6.
3. Schramm VL, May M, Lavorato AS. Gelfoam paste injection for vocal cord paralysis: temporary rehabilitation of glottic incompetence. Laryngoscope 1978; 88:1268-73.
4. Isshiki N, Morita H, Okamura H, Hiramoto M. Thyroplasty as a new phonosurgical technique. Acta Otolaryngol 1974; 78:451-3.
1 Faculty Professor in Otorhinolaryngology, Department of Otorhinolaryngology and Human Communication Disorder, Federal University of Sao Paulo - UNIFESP - EPM.
2 Speech and Voice Therapist, Specialization in Human Communication Disorders, Federal University of Sao Paulo - UNIFESP- EPM. Speech and voice therapist, Instituto da Laringe - INLAR.
Instituto da Laringe - INLAR - Sao Paulo
Address correspondence to: Rua Dr. Diogo de Faria, 171 Vila Clementino Sao Paulo 04037-000
Tel (55 11) 5549-2188 - Fax (55 11) 5575-7649 - E-mail: ppontes@inlar.com.br or vpedrosa@inlar.com.br