Year: 2002 Vol. 68 Ed. 6 - (10º)
Artigos Originais
Pages: 834 to 837
Injection of esclerosant substance on tongue base: experimental model for OSAS treatment
Author(s):
Rony P. Lopes 1,
Luciano G. Gomes 1,
Danielle Ramos 1,
Maria Célia Jamur 2,
José A. A. Oliveira 3,
Denílson S. Fomin 4
Keywords: OSAS, tongue base, injection, esclerosant substance
Abstract:
The obstructive sleep apnea syndrome is a medical and social problem with important comorbidities. It has being treated by desobstruction of the airway that collapse causing breathing stop. The treatment varies since using CPAP until nasal, palatal and tongue base surgeries demonstrating good results proportionally to the previous sites evaluation. Study design: Experimental. Aim: Evaluate histological changes on pigs tongue base after injection of ethamolin® in that site. Material and Method: It has injected ethamolin® in pigs tongue base wich were divided in three groups: a control pig not injected; two pigs that were injected in tongue base and sacrified in sixty hours; five pigs that were injected in tongue base and sacrified in five weeks. All of them were injected in the same day. The animals had their tongues took of and slices were prepared for histological analysis. Results: Increase of collagen occured in the sites injected with ethamolin® after sixty hours and was showed more evident in five weeks. Discussion: Use of ethamolin® induced fibrotic reaction in the treated animals tongue base comproved by the increase of the collagen in this site, a fact that can help on treatment of OSAS because fibrosis leads to tissue reduction. Conclusion: We have concluded in this study that occurred tissue fibrosis formation with collagen increase in pig tongue base by using etanolamina (ethamolin®).
![]()
Introduction
The snoring and Obstructive Sleep Apnea Syndrome (OSAS) are medical-social conditions related to significant co-morbidity factors such as systemic high blood pressure, acute myocardial infarction (AMI), and cerebral vascular accidents (CVA) related to these alterations 1-5. The patients that suffer from sleep apnea have their quality of life affected due to sleepiness at daytime that may have variable levels, depending on the severity of the illness.
The prevalence of OSAS ranges from 40% to 60% according to the author, and its incidence is two times higher in males than in females5, 6.
Several treatments are used, and the high resolution rates of the disease are proportional to the accurate evaluation of the obstructive site7-10. One of the key factors for the success of the OSAS is the topographic diagnosis of the breathing obstruction and the accurate indication of several management procedures, whether surgical or not. The treatment of OSAS is based on sustaining the patency of the upper airways, therefore preventing an interruption on the airway flow in the nasal, hypo or oropharynx, and ensuring the proper oxygen saturation in the blood. In the investigation of the likely sites of airway obstruction we should pay attention to the deviation of the nasal septum and nasal conchae hypertrophy, laxity or redundancy of the veli palatini, reduction of the space of the oropharynx or hypopharynx by enlarged pharyngeal or lingual tonsils, or by the increased volume of the tongue base. If these structures present hypertrophy they may lead to narrowing or even total interruption of the air column in these sites.
Among the surgical options for the treatment of OSAS we found the techniques that use cold “ instruments” and the techniques assisted by specific instruments such as CO2 laser, electrocautery devices and radio-frequency that provide higher safety and comfort for both doctors and patients if surgery is needed10-14. All these surgical procedures have shown results7, 9,12,14, improving the quality of life of patients; however, a major hindrance of the surgical treatment of OSAS is the post operative pain reported by patients in a significant and systematic way in lower or higher intensity. 9 Another significant hurdle in the treatment of respiratory sleeping disorders is its high cost due to the high level of technological complexity of the tools involved in the surgical procedures. The use of the sclerosing agent ethamolin® could be an alternative treatment. Ethamolin® is a sterile agent that irritates the tunica intimae of the vascular wall, used in sclerotherapy of varicose veins. Brietzke10 has been using a similar procedure that utilizes another sclerosing drug, the Sothradecol®, injected in the palate of the patients with snoring symptoms. The author reported a significant improvement of snoring in 92% of the cases due to the increase of palate tension, with mild intra and postoperative pain (average of 3 in a visual scale of 1 to 10). There are not histological studies available on the action of sclerosing drugs that explain the changes reported by Brietzke.
Objective
The objective of this study is to analyze the action of the sclerosing agent ethanolamine (ethamolin®) on the histology of the base of the tongue of pigs.
Material And Method
We decided to use pigs due to the similarity between the tongues of these animals and the human tongue 13, particularly in thickness. The animals fasted for 12 hours and have undergone general anesthesia with Thionembutal intravenously after previous administration of intramuscular ketamine. The exposure of the oropharynx was made by fixing the mandible in the inferior part and elevating the animal maxilla, obtaining a clear and wide view of the posterior side of the tongue. Next, 1.5 ml of drug was injected in the base of the tongue of pigs, and three points were chosen following the V of the tongue, and 0.5 ml of ethamolin (ethanolamine 50 mg with Benzilic Alcohol at 20 mg) was injected in each point approximately 0.5mm deep. Eight animals were studied with weights ranging from 10.5 kg to 17 kg (average of 14.5 kg), and the control has not undergone the procedure. The animals were injected on the same day; three (including the control) were sacrificed 60 hours after the procedure and the remaining 5 animals were sacrificed five weeks after ethamolin injection. Painkillers and antibiotic prophylaxis were used during the procedure and for two additional days after it. Baytril® and Banamine® were used as antibiotics and painkiller, respectively, at dosage of 0.1 ml per kg of weight. Evidences of pain or epithelial damage were not found in the tongue of such animals, which were able to eat easily. The animals were fed with a specific feed to prevent high weight gain in the animals, which ended up presenting low weight variations at the end of the study. The tongues were removed and prepared for histological analyzes of the injected sites. Fixation was performed with 10% buffered formaldehyde for 72 hours. The pieces were dehydrated in increasing sequence of ethanol, diaphanized in xylene and included in paraffin. Next, they were section in 5 mm thick sections, deparafinized in xylene, hydrated in a solution Sirius Red of 0.1 g in 100 ml of saturated picric acid at pH 2.0 for 20’solution and washed twice in running water for 10’ and once in distillated water. The counter staining was performed with Harris hematoxylin for 1’ and then the slides were washed in running water once. Subsequently, the slides were dehydrated at an increasing sequence of ethanol, diaphanized and assembled in Permount (EM Sciences-Fort Washington, USA). The slides that had sections stained with Sirius Red were observed and photographed by light microscopy using an Olympus BX50 in dark field obtained by polarizing filter.
Results
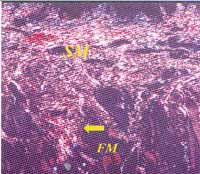
The microscopic analyzes of the damages caused by the ethamolin injection in the base of the tongue of swine showed in the optical microscopy with polarizing filters that the fibrosis is observed through the compacting and thickening of the collagen fibers in the submucosa (Figures 3 and 4) against the control (Figures 1 and 2). Sixty hours after the ethamolin injection we observed an increase in the thickness of the subepithelial layer secondary to the fibrosis, including the surroundings of the muscle fibers. In relation to the control, there was an increase in the collagen found in the submucosa and around the muscle fibers of the animals that were sacrificed in five weeks. No lesions were found in the epithelial cover of the animals that have undergone the treatment compared to the control animal.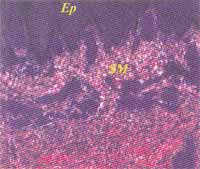
Figures 1 and 2. Polarization microscopy of the sections of control animals.
Figure 3. Polarization microscopy of the sections of the animals that have undergone the treatment and were sacrificed sixty hours later. Sixty hours after the injection of ethamolin we observed an increase in thickness of the subepithelial layer secondary to fibrosis, including the tissue adjacent to the muscle fibers.
Figure 4. Polarization microscopy of the sections of the animals that have undergone treatment and were sacrificed five weeks later. This increase was equally significant in the tongue of the pigs that were sacrificed five weeks after the procedure.
Legend: SM- submucous; Ep-epithelium; FM- muscular bundle; Arrow –fibrosis between the muscular bundles (collagen thickening)
Discussion
In this study we observed the compaction and thickening of the collagen fibers in the tongue submucosa of swine injected with ethamolin® compared to the control animal. This alteration pattern suggests that there may be tension increase and local volume reduction according to Fomin (2002). No lesions were found in the epithelial cover or necrosis spots in the animals that had undergone the treatment compared to the control.
Powell et al. (1997) demonstrated the use of radiofrequency in the base of the tongue of swine, and the histological analyzes showed fibrosis and chronic inflammatory process three weeks after the procedure. Courey et al (1999) and Fomin (2000), using radiofrequency in the palate of swine, also showed fibrosis process in the palate, but they showed a large area of collagen build up between the muscle fibers, probably resulting from a chronic inflammatory process. Brietzke & Mair (2001) suggested that the Sothradecol substance would be ideal to be used in the palate of patients with snoring symptoms, because after local damage, it is likely followed by collagen deposition that would promote the increase of the palate tension, but they never published any histological analyzes. The authors obtained only clinical and subjective improvement results in the snoring symptom of the patients that underwent this type of sclerotherapy.
Fomin (2002) showed that the amount of collagen in the palate of patients that have undergone radiofrequency or laser was increased, particularly type I collagen, and it was strictly related to the subjective improvement of snoring and sleepiness at daytime.
Conclusion
According to the present study, we concluded that the compaction and thickening of the collagen and the formation of fibrosis in the base of the tongue of swine occurred due to the use of ethanolamine (ethamolin®), and it may contribute to trial studies of new non-invasive therapies for the treatment of OSAS caused by the obstruction of the base of the tongue.
REFERENCES
1. Hillman DR. Sleep Apnea and Myocardial Infarction. Sleep 1993;16:23-24.
2. Kosenvuo M, Kaprio J, Telakivi T, Partinen M, Sarna S. Snoring as a risk factor for ischaemic heart desease and stroke in men. BMJ 1987;294:16-19.
3. Olson LG, King MT, Hensley MJ, Saunders N. A community study of snoring and sleep-disordered bresthing: health outcomes. Am J Respir Crit Care Med 1995;152:717-720.
4. Partinen M, Guilleminault C. Daytime sleepness and vascular morbidity at seven-year follow-up in obstructive sleep apnea patients. Chest 1990;97:27-32.
5. Roux F, DAmbrosio C, Mohsenin V. Sleep-related breathing disorders and cardiovascular disease. Am J Med 2000;108:396-400.
6. Zamarron C, Gude F, Otero Otero Y, Rodriguez-Suarez JR. Snoring and myocardial infarction: a 4-year follow-up study. Resp Med 1999;93:108-112.
7. Woodson BT, Huntley TC, Mickelson SA, Nelson LM. A Multi-Institutional Study of Tongue Somnoplasty for OSA. Otolaringol Head and Neck Surg 2000;123(2):53-54.
8. Powell NB, Riley RW, Guilleminault C. Radiofrequency Tongue Reduction in Sleep Disordered-Breathing: A Pilot Study. Otolaryngol Head and Neck Surg 1999;120:656-664.
9. Silva MN, Oliveira JAA, Fomin DS, Vallejo JC. Análise e Comparação da Dor Pós-Operatória em Pacientes Operados por LAUP e Radiofreqüência para Tratamento do Ronco. Revista Brasileira de Otorrinolaringologia 1999;65(6):504-508.
10. Brietzke SE. Injection Somnoplasty: How to treat Snoring Without All The Pain and Expence. Otolaryngol Head and Neck Surg 2001;124(5):503-510.
11. Powell NB, Riley RW, Troell RJ. Radiofrequency Volumetric Reduction of the Tongue: A Porcine Pilot Study for the Treatment of OSAS. Chest 1997;111:1348-1355.
12. Pinto JA, Fomin DS. Radiofreqüência para redução volumétrica dos tecidos. Ronco e Síndrome da Apnéia Obstrutiva do Sono. Rio de Janeiro: Revinter; 2000. cap. 11, p.78-88.
13. Courey MS, Fomin DS, Smith T, Huang S, Sanden D, Reinisch L. Histologic and Physiologic Effects of Eletrocautry, CO2 Laser and Radiofrequency Injury in The Porcine Soft Palate. Laryngoscope 1999;109:1316-1319.
14. Walker RP. Head and Neck Surgery-Otolaryngology. In: Bailey BJ. Second Edition, 1999.
15. Kanzler M. Basic Mechanisms in Healing Cutaneous Wound. Journal Dermatology Surg Oncol 1986;12(11):1156-1164.
16. Fomin DS. Alterações Histológicas e Tensiométricas na Uvulopalatoplastia com Eletrocautério, Laser de CO2 e Radiofreqüência em Modelo Animal. Dissertação de Mestrado apresentada a Faculdade de Medicina de Ribeirão Preto. USP, 2000.
17. Fomin DS. Análise Histológica pós-operatória do colágeno no palato mole de pacientes submetidos à uvulopalatoplastia. Tese de Doutorado apresentada a Faculdade de Medicina de Ribeirão Preto- USP, 2002.
1 Resident physician in Otorhinolaryngology, Hospital das Clínicas, Medical School of Ribeirão Preto, USP.
2 Professor, Department of Morphology, Medical School of Ribeirão Preto, USP.
3 Faculty Professor, head of the Department of Otorhinolaryngology and Ophthalmology, Medical School of Ribeirão Preto, USP.
4 Ph.D. in Medicine, Master in Otorhinolaryngology, Medical School of Ribeirão Preto/USP. Assistant Physician at Hospital das Clínicas, Medical School of Ribeirão Preto, USP.
Department of Otorhinolaryngology, Ophthalmology and Head and Neck Surgery, Hospital das Clínicas, Medical School of Ribeirão Preto, USP.
Study conducted at the Department of Otorhinolaryngology and Ophthalmology, Medical School of Ribeirão, University of São Paulo.
Address correspondence to: Departamento de Otorrinolaringologia e Oftalmologia da Faculdade de Medicina de Ribeirão Preto –
Av. Bandeirantes, 3900 Ribeirão Preto SP 14049-900
Tel (55 16) 602-3000 – Fax (55 16) 633-1586.
Article submitted on October 01, 2002. Article accepted on October 17, 2002