Year: 2003 Vol. 69 Ed. 3 - (20º)
Relato de Caso
Pages: 427 to 431
Rubinstein-Taybi Syndrome: physical anomalies, clinical and audiologic evaluation
Author(s):
Regina H. G. Martins 1,
Elaine C. Bueno 2,
Marisa P. Fioravanti 3
Keywords: Rubinstein-Taybi Syndrome, otorhinolaryngology, hearing loss, mental retardation
Abstract:
Introduction: The Rubinstein-Taybi Syndrome was first described in 1963 when the authors presented seven children with mental and growth retardation, broad thumbs and big toes, associated to face anomalies. Years later new publications characterized other physical anomalies. The incidence in the general population is one in 300.000 borns and the aetiology is unknown until now. The purpose of this study was to present the clinical manifestations, physical anomalies and the audiologic evaluation of five children with Rubinstein-Taybi Syndrome. Report of Cases: Five children with Rubinstein-Taybi Syndrome were evaluated by main clinical manifestations, physical anomalies and audiologic evaluation. The main clinical and physical manifestations were: mental retardation, short stature, short and broad fingers, beaked nose, high palate, irregular placement of teeth and poor speech development. The auditory acuity was evaluated by tonal audiometry, tympanometry and auditory brainstem response (ABR). Discussion: The physical characteristics presented by the patients with Rubinstein-Taybi Syndrome facilitate the diagnosis and are responsible for otolaryngological and phonoaudiological symptoms, like airway infections, nasal obstruction, otitis media, tonsillar hyperplasia, deafness, perioral hypotonia and dysphagia. The cognitive impairment is responsible to speech delay and learning disabilities. Conclusion: The presence of otolaryngologic and phonoaudiologic symptoms in patients with Rubinstein-Taybi Syndrome permit specialists to make early diagnoses and treatment.
![]()
INTRODUCTION
Rubinstein-Taybi syndrome has an incidence of 1 in every 300,000 live births in the general population and 1 in each 300 children with mental retardation. It is less frequent in African-descendents and there is no gender relation. Among the main physical anomalies and clinical manifestations presented by the people with Rubinstein-Taybi syndrome we can point out low stature, wide and large thumbs, craniofacial anomalies, among them microcephalia, corpus callosum agenesia, prominent frontal region, anti-mongoloid oblique palpebral cleft, strabismus, nasal pyramid alteration with high nasal dorsum, anterior growth of the cartilaginous septum towards the columella, septum deviation, maxilla hypoplasia, high palate, submucous cleft palate with or without bifid uvula, micrognathia, and morphological abnormalities of the teeth. Such children frequently present low intellectual level and delay of the neuropsychological motor and language development.
REVIEW OF THE LITERATURE
Rubinstein-Taybi syndrome was described for the first time in 1963, when the authors that named it described similar clinical manifestations and physical characteristics of seven children who had mental retardation, facial anomalies and wide fingers 1. As of then, other similar cases were reported by the literature, collaborating for the definition of the genetic traits presented by the holders of the disease 2, 3, 4.
The exact etiology is still unknown, even though some authors believe that it is a dominant autossomal inheritance with variable penetration, considering the various descriptions of phenotypes of the syndrome in various members of the same family, as well as in identical twins 5, 6, 7. The characteristics of the phenotype define the facial traits that are markedly characteristic of the syndrome 6, 8.
The several cranial-facial affections presented in such patients with Rubinstein-Taybi syndrome lead them to the manifestation of ENT and speech and language symptoms, reason why it is so important to know about this genetic syndrome.
The present article aimed at describing the main physical characteristics, clinical manifestations (emphasizing those that belong to the area of ENT and speech and language disorders) and the results of hearing tests of five children with Rubinstein-Taybi syndrome, seen by the outpatient unit of Otorhinolaryngology, Medical School of Botucatu (Unesp).Table 1. Main physical anomalies and clinical manifestations observed in children with Rubinstein-Taybi syndrome.
Table 2. Result of otoscopy and hearing acuity tests.
CASE REPORT
The study was approved by the Ethics Committee on Human Being Research Studies. We recorded results of ENT assessment, speech and voice, motor oral and reading and writing tests, and hearing acuity of five children with Rubinstein-Taybi syndrome. At the time of the study, the children who had already been discharged from hospital were invited again to come and take the tests.
As to hearing acuity, we performed the following tests: conventional pure tone audiometry (audiometer Madsen OB822); immittanciometry with tympanometry curves and stapedial muscle reflexes, obtained at 70 and 90 dB higher than the auditory thresholds of patients (device Amplaid 75); auditory brainstem potentials (ABR) (device Nihon Koden - MEB 7102 k). Positive electrodes were placed on the forehead and the negative ones on the retroauricular areas, after cleaning the skin with alcohol and abrasive substance. The ground electrode was fixed on the right earlobe. The test was conducted on each individually, with stimulation at 90 dB intensity, contralateral masking below 40 dB intensity of the used stimulus. We used 2,000 clicks, 10 ms of analysis, repeated for the confirmation of wave reproduction. After the collection of records, the intensity of stimuli was progressively reduced to 60 and 30 dB, or down until the absence of wave V, indicating the electrophysiological threshold. If there were no electrophysiological potentials at 90 dB, we increased stimulus to 100 dB.
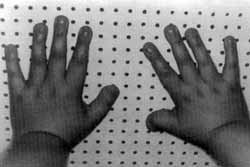
Table 1 synthesizes physical anomalies that were more marked and the clinical manifestations observed in the children. We can point out low stature, wide thumbs, high nasal pyramid, high palate, dental arches malformation, high occurrence of mental retardation, delay in neuropsychomotor and language development, present in all patients of our series. The presence of thick eyebrow and hypertelorism was detected in 80% of the children. Figures 1, 2 and 3 show the child case 1, illustrating the genetic traits described above.
Other observed manifestations were: polydactilia, oblique palpebral clefts, cranial asymmetry, hirsutism, palpebral ptosis, microcephalia, micrognathia, low pinna implantation, maxillary hypoplasia, nasal septum deviation and frontal prominence.
Table 2 presents the results of otoscopy and auditory assessment, which were abnormal in 2 assessed children (cases 1 and 5). In case 1, we observed hyperemia and retraction of both tympanic membranes, type C tympanometry curve and mild conductive hearing loss in both ears (audiometry thresholds at about 30 dB). In case 5, we observed retraction of both tympanic membranes, more marked on the right, type C tympanometry curve and conductive hearing loss on the right. The other children presented otoscopy and hearing assessment within the normal range.
Auditory brainstem potentials were conducted in 3 children only (cases 1, 3 and 5). One of the children did not allow the performance of the test, even after many attempts, and the other did not come to perform it. The test was normal in child number 3 and abnormal in cases 1 and 5, being that in such cases we detected conductive hearing loss pattern, that is, prolongation of isolated latencies of waves as of PI, and normal values of LI-LIII, LI-V and LIII-V, with electrophysiological potential thresholds at about 40 dB.
Figure 1. Child with Rubinstein-Taybi syndrome - note the nasal pyramid format and upper maxilla hypoplasia.
Figure 2. Malformation of the toes in a child with Rubinstein-Taybi syndrome.
Figure 3. Malformation of the thumbs (short and wide) of a child with Rubinstein-Taybi syndrome.
DISCUSSION
The main facial traits of Rubinstein-Taybi syndrome described in the literature were easily identified in our children. The characteristic format of the high and elongated nasal pyramid (beaked nose) associated with maxilla hypoplasia, hypertelorism, wide and large thumbs, led us to the suspicion of the diagnosis right on the first visit (Figures 1, 2 and 3).
The many facial affections make them present manifestations related to the area of ENT, such as nasal obstruction, upper airway repetitive infections and adenoid-tonsillary hypertrophy. Most of the children studied by us presented complaints of upper airways even after childhood, characterized by sinusitis, otitis and repetitive tonsillitis. In two children (cases 1 and 5), otoscopy as well as the auditory assessment, were abnormal, indicating impairment of the middle ear (conductive hearing loss), probably secondary to repetitive episodes of upper airway infections. Stevens et al. (1990)9 conducted a study in 50 patients with Rubinstein-Taybi syndrome and observed high incidence of frequent pictures of ear infections, present in 52% of the patients, with varied degrees of hearing loss.
The most frequent speech and language manifestations were oral language difficulties and perioral muscle tone abnormalities, which can be perceived at birth during the first attempts to breastfeed the child, when they present difficulty to suck and swallow. Such complaints were reported by two mothers (cases 3 and 4), who required professional guidance on swallowing. Coffin (1964)3 assessed six children with Rubinstein-Taybi syndrome and observed swallowing difficulties in infant years in all of them. Partington (1990)10 emphasized the occurrence of dysphagia episodes in these children, many times responsible for the aspiration pneumonia they present.
As to language development and school performance, we followed up the children during childhood and adolescence; when they were reassessed they evidenced difficulties to acquire language and learn how to read and write. It is believed that the high incidence of mental retardation, present in all assessed children (Table 1), was the main factor to account for school performance limitations and poor language development. We observed severe impairment of attention and memory, little interest in therapy sessions, even when it was a playing situation, difficulty in school activities, even of elementary level, such as color identification and geometry shapes, and extremely slow cognitive development. Only one child (case 3) managed to go to regular school up to the 4th grade, but he presented severe learning difficulties. According to the literature, mental retardation is present in all children who have Rubinstein-Taybi syndrome 9, 11, 12, at varied states, a fact that was confirmed by our cases.
All children studied under our protocol presented poor language, comprising short sentences, few connecting elements, many times restricted to verb and direct object, simple vocabulary, with little creativity to narrate facts. Except for the child in case 3, all the others presented language impairment that proved to be severe, affecting directly their emotional balance, manifested by irritability and anxiety. In all children we could observe performance in sign language associated with verbal language. Despite linguistic difficulties, we observed communication intention in all of them. Receptive language was more preserved than expressive language, a fact observed also by Battaglia & Ferrari (1993)12.
Reevaluation of these children at adolescence allowed us to observe that the new acquisition of language and cognitive development after discharge had been very limited. They ended up being adapted by their restrictive social environment and conducting daily home chores since they had no formal education.
REFERENCES
1. Rubinstein JH, Taybi H. Broad Thums and toes and facial abnormalities. A possible mental retardation syndrome. Am J Dis Child 1963;105:88-108.
2. Filipp G. The Rubinstein-Taybi syndrome: report of 7 cases. Clin Genet 1972;3:303-18.
3. Coffin GS. Brachydactyly, peculiar facies and mental redardation. Am J Dis Child 1964;108:351-9.
4. Ciacci G, D'amore I, Fabrizi G, Rocchi R, Volpi N, Federico A. Rubinstein-Taybi Syndrome: report of two cases. Acta Neurologica (Naples) 1988;43:335-42.
5. Berry AC. Rubinstein-Taybi Syndrome. J Med Genet 1987;24:526-66.
6. Rubinstein JH. Broad thumb-hallux (Rubinstein-Taybi) Syndrome. Am J Med Genet 1990; 6:3-16.
7. Ghanen Q, Dawod S. Monozygotic twin concordant for Rubinstein-Taybi syndrome. Clin Genet 1990;37:429-34.
8. Allason JE. Rubinstein-Taybi Syndrome: The changing face. Am J Med Genet 1990; [Suppl]6:38-41.
9. Stevens CA, Carey JC, Blackburn BL. Rubinstein-Taybi Syndrome: A natural history study. Am J Med Genet 1990; [Suppl]6: 30-7.
10. Partington MW. Rubinstein-Taybi Syndrome: A follow-up study. Am J Med Genet 1990; [Suppl]6: 65-68.
11. Hennekam RCM. Psychological and speech studies in Rubinstein-Taybi Syndrome. Am J Mental Retardation 1992;96: 645-60.
12. Battaglia A, Ferrari AR. Cognitive and psychological profiles in dysmorphic syndromes. La Pediatria Medica e Chirurgica 1993;1:23-5.
1 Ph.D., Assistant Professor, Discipline of Otorhinolaryngology and Head and Neck Surgery, Medical School of Botucatu (UNESP).
2 Speech Therapist and Audiologist, Improvement Course in Speech and Language Pathology and Audiology, Discipline of
Otorhinolaryngology and Head and Neck Surgery, Medical School of Botucatu (UNESP).
3 Speech Therapist and Audiologist, Discipline of Otorhinolaryngology and Head and Neck Surgery, Medical School of Botucatu (UNESP).
Address correspondence to: Regina Helena Garcia Martins - Faculdade de Medicina de Botucatu (UNESP) Departamento de Oftalmologia,
Otorrinolaringologia e Cirurgia de Cabeça e Pescoço 18618-970 Botucatu SP
Tel (5514) 6802-6256 - E-mail: rmartins@fmb.unesp.br
Study conducted at the Discipline of Otorhinolaryngology and Head and Neck Surgery, Medical School of Botucatu (UNESP).
Article submitted on August 14, 2002. Article accepted on August 29, 2002.