Year: 2001 Vol. 67 Ed. 4 - (14º)
Artigos Originais
Pages: 536 to 542
Laryngeal Electromyography.
Author(s):
Jeanne R. O. Ramalho*,
Renato J. Corso*,
Gustavo D. Ferreira*,
Henrique C. F. Pinto**,
José A. Pinto***,
Antonio L. Catai****.
Keywords: vocal fold, electromyography, larynx
Abstract:
Introduction: Laryngeal dysfunction and vocal fold immobility have been increasingly detected in our clinical practice, although it is still a challenge to differentiate between an immobile vocal cord due to paralysis or mechanical limitation. Laryngeal electromyography is an essential test for the objective evaluation of neuromuscular status and laryngeal function. The procedure has prognostic value and influences treatment. Study design: Clinical prospective. Aim: We present our experience in a clinical setting with five patients submitted to laryngeal electromyography. The advantages and disadvantages of the procedure, the results and management of the cases are discussed. Conclusion: Our data have shown that laryngeal electromyography is a viable, low cost, office procedure with minimum discomfort to the patient, without complications.
![]()
INTRODUCTION
Vocal fold mobility abnormalities are easily diagnosed by the clinical history and the physical examination. However, the differential diagnosis between immobility due to mechanical limitation and neuromotor disorders is difficult and has therapeutic and prognostic implications. Laryngeal electromyography is a clinical method that assesses the laryngeal function, used to differentiate neuropathy, myopathy, brainstem lesions, anterior medullar neuron diseases and neuromuscular transmission disorders, and to define which is the affected nerve (superior laryngeal or recurrent nerves), objectively differentiating between immobility due to mechanical limitations and neuromuscular transmission disorders. Moreover, it provides information about severity and extension of the nervous involvement, with prognostic value for the recovery of facial palsy, especially if performed early.
The first reports of the use of electromyography to study laryngeal intrinsic muscles were published by Weddel14, but the technique did not become wide spread in clinical practice9.
Recently, the interest in its clinical applicability was renewed after the publication of some articles that showed that electromyography use is essential to distinct recurrent laryngeal nerve paralysis from arytenoid fixation10,14. Laryngeal electromyography technique, with positioning of the electrode percutaneously, was initially reported by Fink6, and later internal muscle laryngeal access was standardized based on the anatomical projections of the laryngeal frameworks.
Despite its invasive character, it has high diagnostic, therapeutic and prognostic value, distinguishing vocal fold paralysis and arytenoid fixation, predicting the restoration of vocal movement, guiding injection of toxin botulinus, providing intraoperative monitoring to prevent damage of the recurrent laryngeal nerve and differentiating central and peripheral neuropathy and myopathy.
The purpose of the present study was to assess applicability of the technique, as well as its daily practical use, showing the real advantages and disadvantages of laryngeal electromyography and the experience of our service in diagnosing and treating laryngeal neuromotor disorders.
MATERIAL AND METHOD
We used percutaneous laryngeal electromyography in five consecutive patients who had laryngeal alterations, from paralysis to traumas and neurological conditions. The test was conducted in the ambulatory by removing all electrical devices from the room and providing appropriate grounding to the patients and the device. At the same time, we conducted indirect laryngoscopy with flexible endoscope for continuous visualization of the vocal folds and confirmation of the position of the electrode.
Figure 1. Nicolet electromyography device and laptop.
Figure 2. Stimulator and surface electrode.
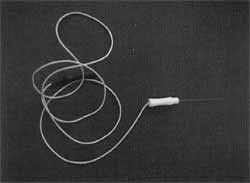
Electromyography consists of the study of the electrical activity in muscles and nerves. In the present article, laryngeal electromyography involved the areas of recurrent laryngeal nerve, through the electrical study of the thyroarytenoid muscle. The electromyography device used was Nicolet, model Compass Portabook II, double channel (Figure 1). The computer in which we recorded tracings was a laptop, model Extensa 502 DX, and the software was Compass-DOS-version 6.2. We used a 10mm silver plate electrode as reference, surface electrodes (Figure 2) and another monopolar needle electrode, model 902-DMF37, to collect the responses (Figure 3).
Figure 3. Monopolar needle electrode.
Figure 4. Right thyroarytenoid muscle - at rest - spontaneous potentials of denervation, fibrillation and positive waves.
The test analyzed insertion activity potentials (LAP), rest potential (RP) and action potential (AP); in addition, we performed electrical stimulation of the vagus nerve, in its high cervical tract, to analyze neural function. Insertion activity is a result of the mechanical excitation, after the trauma of the needle, promoting a contraction response of muscle fibers, which is present in normal and denervated muscles; however, in the latter, there is increase in LAY value. In normal muscles, IAP lasts between 8 and 20 ms. The increased duration implies alterations of electrical activity, which may be present in myopathy or neuropathy. During rest, in general, there is no electrical detectable activity in the examined muscle point: it is electrical silence. In cases of denervation, there may be spontaneous potentials of fibrillation or positive waves (Figure 4). During muscle contraction, we normally observe two or three-phase potentials (Figure 5). In cases of myopathy, they have low amplitude, short and paradoxical duration (great recruitment of motor units for little exerted force). In neuropathy, they are polyphasic (more than three phases), with increased duration and rarefaction at minimal contraction (Figure 6). Polyphasic action potentials of motor units (APMU) show the existence or previous existence of reinnervation.
Patients were instructed about the procedure, positioned in supine and after a slight extension of the neck we identified the anatomical projections of the thyroid and cricoid cartilages arid the cricothyroid membrane, submitted to scrubbing. We infiltrated the skin, over the cricothyroid membrane, with 1mL xilocaine at 2%. Some authors believe that local anesthesia is dispensable, since the procedure is relatively painless2. At the same time, we conducted indirect laryngoscopy with flexible endoscope located in the supraglottis, in order to enable continuous visualization of the vocal folds. The needle electrode was percutaneously inserted in the cricothyroid membrane, at the midline, right above the cricoid cartilage, directed upwards and laterally until it reached the thyroarytenoid muscle, as described by other authors5,11,12 (Figure 7). In order to make sure that the electrode was correctly placed in the thyroarytenoid muscle, we conducted a fibroscopy through the oscilloscope of the device that showed the insertion potential when the needle was introduced in the muscle and by the action potential during phonation. We also performed electrical stimulation to assess neural function. In cases of unilateral paralysis, we started the procedure on the normal side to evaluate normal potentials and then compared with the affected side. In cases of bilateral paralysis, we used the orbicular oris muscle as a parameter.
Case 1
Female, 62-year-old patient, admitted to the Intensive Care Unit (ICU) of Hospital a Maternidade São Camilo (HMSC), with orotracheal intubation because of acute respiratory failure resultant from fungal lobar pneumonia. She remained intubated for 13 days and two days after removal of the tubes she started to manifest aphonia, bronchial-pulmonary aspiration and generalized hypotonia (flaccid tetraparesis, symmetrical areflexia and laxity). Indirect laryngoscopy with flexible endoscope showed bowing of vocal folds and absence of bilateral movement, with glottic incompetence. Laryngeal electromyography revealed right and left thyroarytenoid muscle with spontaneous denervation potentials, fibrillation and positive waves at rest (Figure 4); for voluntary contraction, there was action potential in the polyphasic motor unit, low amplitude and rarefaction (Figure 6). She presented normal conduction of electrical stimulation, with no signs of demyelination, suggesting axonal damage. Picture compatible with acute axonal polyradiculoneuritis with bulbar predominance. After treatment of central neuropathy, she restored phonation and glottic competence.
Figure 5. Right thyroarytenoid muscle - normal voluntary contraction.
Figure 6. Left thyroarytenoid muscle - voluntary contraction action potential of the polyphasic motor unit, low amplitude and rarefaction.
Figure 7. Percutaneous insertion of the monopolar needle electrode.
Figure 8. Left thyroarytenoid muscle - voluntary contraction action potential of the normal motor unit.
Case 2
Female, 30-year-old patient with Down syndrome, submitted to cervical discectomy through right lateral cervical access, who progressed after surgery to dysphonia and aspiration. Indirect laryngoscopy with flexible endoscope revealed immobility of right vocal fold at paramedian position and parallel glottic chink. At laryngeal electromyography, conducted on the second post-operative day, she had normal left thyroarytenoid muscle and right thyroarytenoid muscle with fibrillation, abundant positive waves (signs of denervation); at rest, during contraction, she presented long lasting polyphasic potentials and extreme rarefaction of potentials. During the electrical stimulation of right recurrent laryngeal nerve, there were attempted impulses but no recordable responses, whereas the electrical stimulation of left recurrent laryngeal nerve produced normal impulses. The patient was submitted to speech therapy and two months later the clinical picture showed improvement, dispensing surgical intervention.
Figure 9. Right thyroarytenoid muscle - voluntary contraction - long lasting polyphasic action potentials.
Case 3
Female, 49-year-old patient with coronary artery disease, was submitted to myocardium revascularization one month before, progressing with post-operative dysphonia and choking. Flexible indirect laryngoscopy showed immobility of the left vocal fold, compensated by the contralateral vocal fold. Laryngeal electromyography showed normal motor unit action potentials (Figure 8), suggesting fixation of the left vocal fold by ankylosis of the cricothyroid joint, probably caused by intubation trauma. Since the patient was compensated, she was referred to speech therapy and the vocal condition showed improvement.
Case 4
Female, 36-year-old patient, victim of a car accident 13 years before, submitted to ototracheal intubation for 20 days, followed by tracheotomy 3 months later. After decannulation, she presented dysphonia (hoarse and breathy voice) and took voice therapy sessions with no improvement. At laryngostroboscopy, she showed immobility of right vocal fold at paramedian position and parallel glottic chink, with absence of mucosal wave. One year before, she had been submitted to right arytenoid adduction by Netterville's technique, followed by voice therapy (30 sessions); dysphonia persisted, with no vocal improvement. At laryngostroboscopy, there was posterior glottic chink and absence of mucosal wave. At laryngeal electromyography, the results were normal (Figure 5). Three months later she was submitted to revisional surgery of right arytenoid adduction, by Isshiki's technique (type 2 thyroplasty). She presented improvement of voice and hoarseness and indirect laryngoscopy revealed good glottic coaptation.
Case 5
Female, 50-year-old patient with peripheral polyneuritis, she was admitted to the ICU with bilateral lobar pneumonia, intubated for 12 days, and presented post-intubation manifestation of dysphonia and choking. Indirect laryngoscopy showed right vocal fold immobility at literal position, bowing of folds, ample spindle chink and salivary aspiration. Laryngeal electromyography showed normal left recurrent laryngeal nerve and normal voluntary contraction of left thyroarytenoid muscle. Right thyroarytenoid muscle had pseudomyotonic discharges at rest. At voluntary contraction, there was rarefaction of interference potentials and long lasting polyphasic action potentials (Figure 9). The test favored reinnervation, indicating good prognosis.
RESULTS
In the cases reported here, we noticed different electromyographic alterations and action potentials with variable amplitude and duration, which hindered the interpretation of the test. It is important to define some interpretation reference point and we created that in our service together with the electrophysiologist: 500mV/ division for the normal motor unit action potential. Therefore, it enabled distinction of normal and pathological waves.
In Case 1, laryngeal electromyography revealed marked denervation of thyroarytenoid muscles, electrical stimulation showed preserved neural conduction, with no signs of demyelination, suggesting axonal damage. These results, together with generalized hypotonia, were essential to define the diagnosis of acute axonal polyradiculoneuritis with bulbar predominance. The patient was treated from the neurological condition, underwent voice therapy and after improving her central neuropathy, restored phonation and glottic competence.
In Case 2, laryngeal electromyography defined the diagnosis of right iatrogenic lesion post-discectomy. This is a condition with a favorable prognosis, because in 80% of the cases, there is a tendency of spontaneous compensation of the lesion within 12 to 18 months. In these cases, there is no need for surgical intervention. The patient was submitted to speech therapy and two months later presented compensation of the contralateral vocal fold, improvement of dysphonia and glottic competence.
In Case 3, laryngeal electromyography was essential to exclude the lesion of left recurrent laryngeal nerve and showed fixation of the vocal fold probably caused by ankylosis of cricoarytenoid joint, resultant from chondritis generated by the trauma of the endotracheal tube.
In Case 4, laryngeal electromyography defined fixation of the arytenoid cartilage as the main cause of right vocal fold immobility, excluding recurrent nerve lesion. It was decisive to indicate surgical reinnervation for the revision of arytenoid adduction and closure of glottic chink, with improvement of vocal quality and dysphonia.
In Case 5, the test was conducted early, after extubation, showing recurrent laryngeal nerve lesion. However, we could not define if the nerve impairment was caused by polyneuritis or by the trauma of the cuff during endotracheal intubation. The presence of polyphasic action potentials was suggestive of reinnervation and good prognosis. We suggested use of nasoenteral tube and voice therapy. One month later, we repeated indirect laryngoscopy and noticed right vocal fold mobility and competent glottis, the early prognosis initially suggested by the laryngeal electromyography.
DISCUSSION
We used percutaneous via laryngeal electromyography, as suggested by different authors5,11,12. As the component of vagus innervation, we studied thyroarytenoid muscle; it corresponds to the representative portion of the function of the recurrent laryngeal nerve, which is easy to access and reliable to study, according to the described technique. In addition to being easily accessed through the skin, its anatomical location allowed endoscopic control to confirm the position of the electrode during the procedure. Another technical advantage is that it is an ambulatory procedure, minimizing the electrical interference that may be present in the operating room7.
Laryngeal electromyography via percutaneous access, with monopolar electrode, may also be used on the posterior cricoarytenoid muscle. It is the only laryngeal abductor muscle and it is extremely important to study its electrical activity in breathy dysphonia and stridor cases2. Although it is not easy to perform, because the needle is positioned posteriorly to the thyroid lamina, reaching the muscle over the cricoid cartilage, it is an extremely important test, especially in bilateral paralysis. Recently, Blitzer1,3 described this technique for the treatment of spasmodic dysphonia of abductors with Botox.
We decided to use monopolar electrodes because they are light, fine, delicate and less traumatic, and because we did not need more precise location of the electrical activity, as provided by the bipolar electrodes, because the control was performed by indirect laryngoscopy.
Laryngeal electromyography has shown to have diagnostic and prognostic value, evaluating the degree of paralysis, documenting denervation and incipient reinnervation. Although some authors9,4 suggested the use of computed tomography or magnetic resonance imaging to differentiate arytenoid cartilage subluxation and vocal fold paralysis, only laryngeal electromyography provides direct evidence of vocal function and clarify the cases of mechanical and neuromuscular alterations that are concomitantly present.
Based on the cases described here, we observed that most of the times the required intervention was clinical and in only one case it was surgical. This rate was achieved thanks to the electrical and functional study of the vocal folds, which provided information about etiology of paralysis and prognosis, guiding the laryngologist to the most suitable procedure.
Differently from what other authors have said13 laryngeal electromyography is technically easy to perform and we found no difficulties in identifying the thyroarytenoid muscle, especially because we used indirect laryngoscopy to confirm the position of the electrode.
CONCLUSIONS
Laryngeal electromyography is a very feasible ambulatory method, presenting extremely good cost-benefit ratio. It is an easy, little invasive, low cost and relatively comfortable technique, with no associated complications, provided that appropriate standards of conduction and interpretation are defined.
It does not provide specific clinical diagnosis per se, but it helps in the assessment of laryngeal disorders, conducting differential diagnosis of lesion site and determining the recovery potential of vocal fold immobility.
It should be used in daily clinical practice because it supports diagnosis of laryngeal dysfunctions and has therapeutic and prognostic value.
REFERENCES
1. BLITZER, A.; BRIN, M. F.; FAHN, S. et al. - Localized injections of botulinum toxin for the treatment of focal laryngeal dystonia (spastic dysphonia). Laryngoscope, 98: 193-197, 1988.
2. BLITZER, A.; BRIN, M. F.; SASAKI, C. T.; FAHN, S.; HARRIS, K. S. - Neurological disorders of the larynx. laed., New York, Thieme Medical Publishers, Inc., 66-81, 1992.
3. BLITZER, A.; BRIN, M. F.; STEWART, C.; FALM, S. Abductor laryngeal dystonia: a series treated with botulinum toxin. ALA 1991. Abstract.
4. CLOSE, L. G.; MERKEL, M.; WATSON, B.; SCHAEFER, S. D. - Cricoarytenoid subluxation, computed tomography, and electromyography findings. Head Neck Surg., 9: 341-8, 1987.
5. Devi, S.; Lovelace, R. E.; Blitzer, A. - Electrodiagnosis of laryngeal muscles. Electroencephal Clin Neurophysiol, 55: 42, 1983.
6. FINK, B. R.; BASCK, M.; EPANCHIN, V - The mechanism of opening of the human larynx. Laryngoscope, 66: 41025, 1956.
7. GARTLAN, M. G.; PETERSON, K. L.; LUSCHEI, E. S.; HOFFMAN, H. T.; SMITH, R. J. H. - Bipolar hooked-wire electromyographic technique in the evaluation of pediatric vocal cord paralysis. Ann. Otol. Rhinol. Laryngol., 102: 695-700_ 1993
8. HIROTO, L; TOYOZUMI, Y; SHIN, T. - A new method of placement of a needle electrode in the intrinsic laryngeal muscles for electromyography. Otorhinolaryngol. Clin. (Kyoto), 55: 499-504, 1962.
9. HOFFMAN, H. T.; BRUNBERG, J. A.; SULLIVAN, M. J.; WINTER, P; KILENY, P R. - Arytenoid subluxation: diagnosis and treatment. Ann. Otol. Rhinol Laryngol, 100: 1-9, 1991.
10. MILLER, R. H.; ROSENFIELD, D. B. - The role of electromyography in clinical laryngology. Otolaryngol. Head Neck Surg., 92: 287-91, 1984.
11. RONTAL, E.; RONTAL, M.; SILVERMAN, B.; KILENY, E R. - The clinical differentiation between vocal cord paralysis and vocal cord fixation using electromyography. Laryngoscope, 103: 133-137, 1993.
12. RODRIQUEZ, A. A.; MYERS, B. R.; FORD, C. N. Laryngeal electromyography in the diagnosis of laryngeal nerve injuries. Arch. Phys. Med. Rehabil, 71: 587-589, 1990. 13. YIN, S. S.; QUI, W W; STUCKER, F. J. - Major patterns of laryngeal electromyography and their clinical applications. The Laryngoscope, 107: 126-136, 1997.
14. WEDDEL, G.; FEINSTEIN, B.; PATTLE, R. E. - The electrical activity of voluntary muscle in man under normal and pathological conditions. Brain, 67: 178-256, 1944.
* Resident Physician, Núcleo de Otorrinolaringologia de São Paulo.
** Assistant Physician, Núcleo de Otorrinolaringologia de São Paulo.
*** Medical Director, Núcleo de Otorrinolaringologia de São Paulo.
**** Electrophysiologist, Physician, Hospital a Matemidade São Camilo.
Study presented at 35° Congresso Brasileiro de Otorrinolaringologia, held on October 16 - 20, 2000, in Natal/RN.
Address correspondence to: Dr. Jose Antonio Pinto - Alameda dos Nhambiquaras, 159-Indianópolis-04090-010 São Paulo/SP
Tel/Fax: (55 11) 5573-1970-E-mail: japorl@cepa.com.br
Article submitted on December 19. 2000. Article accepted on February 16. 2001.