Year: 2001 Vol. 67 Ed. 4 - (10º)
Artigos Originais
Pages: 513 to 517
Endoscopic Endonasal Surgery: Experience in 706 Cases.
Author(s):
Marcus M. Lessa*,
Renata A. Marcondes**,
Elder Y. Goto***,
Fabrízio Romano***,
Richard L. Voegels****,
Ossamu Butugan*****.
Keywords: endoscopic endonasal surgery; functional endoscopic sinus surgery; complications
Abstract:
Introduction: The functional endoscopic endonasal surgery (FEES) is used for diagnosis, biopsy, treatment and follow-up of different diseases. FEES presents a rate of success which ranges from 76% to 98%. It is a conservative surgery, with a more anatomical access to the nasal structures by preserving the mucosa and restoring the nasal function. Aim: The purpose of the present study was to report the experience with FEES in our department. Study design: Clinical retrospective. Material and method: The authors performed a retrospective study of all the endoscopic endonasal surgeries carried out from December 1995 to March 2000. All surgeries were performed by resident physicians of the third year of the Residence Program in Otolaryngology of University of São Paulo, under the supervision of an assistant physician. Results: We analyzed 706 patients, 386 (54.7%) were male and 320 (45.3%) were female. The average age was 35.8 years. As to kind of anesthesia, 700 (99.2%) procedures were carried out under general anesthesia. Intraoperative bleeding was deemed moderate in 432 patients (61.2%) and the use of nasal packing was unnecessary in 96.6% of the patients. Complications were seen in only 16 (2.27%) patients. Conclusion: According to our experience, FEES is an effective method because it allows approach of a great diversity of affections and maximum preservation of the nasal anatomy and physiology, presenting low rates of complications.
![]()
INTRODUCTION
In the 50's, Messerklinger was the first author to describe a systematic approach to perform endoscopic diagnosis of the lateral wall of the nasal fossa. His studies demonstrated that in most cases of maxillary and frontal sinuses pathology the primary disease lies in the narrow spaces of the lateral wall of the nasal fossa and in anterior ethmoid cells. This finding enabled the development of endoscopic surgical techniques directed to the primary affection of the ethmoidal region. Messerklinger observed that the elimination of the ethmoidal primary disease through circumscribed and limited endoscopic procedures resulted in resolution of massive pathologies of the adjacent paranasal sinuses. By analyzing these studies and observations, his disciple Stammberger introduced the term FESS (Functional Endoscopic Sinus Surgery) 12. Endonasal endoscopic surgery was introduced in the US by Kennedy, in 19841, and since then it has presented significant progress.
FESS is used for diagnosis, biopsy, treatment and follow-up of different diseases. It has a success rate that varies from 76% to 98%11. It is a conservative surgery, using an anatomical approach of the nasal structures, preserving the mucosa and restoring normal nasal function12. Thanks to technological progress, it has been widely used and it has provided more precision in diagnosis and treatment of nasosinusal diseases.
The purpose of the present study was to report the experience with endonasal endoscopic surgery in the Division of Clinical Otorhinolaryngology, Hospital das Clínicas, Faculdade de Medicina da Universidade de São Paulo (HC-FMUSP).
MATERIAL AND METHOD
The authors carried out a retrospective study of all FESS procedures conducted in the Division of Clinical Otorhinolaryngology at HC-FMUSP, between December 1995 and March 2000. We included all patients and analyzed the following data: 1. gender and age; 2. diagnosis; 3. type of anesthesia; 4. intraoperative bleeding; 5. type of nasal packing placed in the early post-op period and duration of use; 6. combined surgery; 7. intra and post-operative complications.
Data were collected from the surgical files that were specific and individualized, filled in by the surgeon right after the conclusion of the procedure, and complemented during outpatient postoperative follow-up.
All surgeries were performed by resident physicians, supervised by an assistant physician, under general or local anesthesia with sedation. Intraoperative bleeding was subjectively classified by the surgeon as mild, moderate and severe
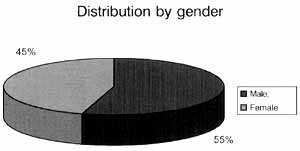
Graph 1. Distribution of patients according to gender.
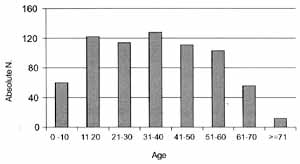
Graph 2. Distribution of patients according to age range.
RESULTS
Gender and age
We analyzed 706 cases, 386 (54.7%) male and 320 (45.3%) female patients (Graph 1). The minimal age was 2 months and the maximum age was 89 years. The mean age was 35.8 years. Distribution of patients according to age range is shown in Graph 2.
Diagnosis
Affections found in patients submitted to FESS are described in Table 1.
Cases of choanal polyps were divided into: antrochoanal, in 27 cases (82%); ethmoidochoanal, three cases (9%), and sphenochoanal, three cases (9%).
The most frequent site of mucoceles were: frontal sinus, 7 cases (28%); frontal-ethmoid, 9 cases (36%); ethmoid, three cases (12%); sphenoid, four cases (16%), and maxillary sinus, two cases (8%).
There were 15 cases of choanal atresia operated on with FESS: two had bilateral atresia and 13 patients had unilateral atresia.TABLE 1 - Affections found in patients submitted to FESS.
Patients with epistaxis were submitted to ligature of sphenopalatine artery: three cases were bilateral and 13 were unilateral.
Histological types of neoplasias are described in Table 2.
Type of anesthesia
As to type of anesthesia, 700 (99.2%) of the procedures were performed under general anesthesia and 6 (0.8%) were performed under local anesthesia with sedation.
Intraoperative bleeding
Intraoperative bleeding was considered mild in 432 cases (61.2%), moderate in 222 cases (31.4%) and severe in 52 patients (7.4%).
Type of nasal packing placed in the early post-operative period and duration of use.
We employed anterior nasal packing with finger glove in 23 cases (3.3%), and all patients maintained it for 48 hours. Anterior-posterior packing was conducted in only one case (0.14%), removed 72 hours later. In the remaining patients (96.6%), there was no need to apply nasal packing.
Combined surgeries
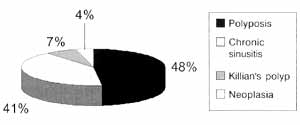
Twenty-seven surgeries were performed with Caldwell-Luc approach (3.82%). Among them, 13 were due to polyposis, two to Killian polyp, 11 to chronic sinusitis and one to neoplasia (Graph 3).TABLE 2 - Histological types of neoplasias resected with FESS.
Graph 3. Distribution of affections that required Caldwell-Luc approach as combined procedure.
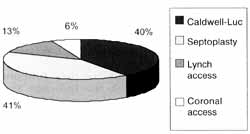
Other combined surgeries were: 28 septoplasties (3.97%), four coronal access (three because of chronic sinusitis and one because of complicated acute sinusitis), nine were via Lynch access (five because of mucoceles, three for chronic sinusitis and one for complicated acute sinusitis). The surgeries are shown in Graph 4.
Intra and post-operative complications
Among all cases, there were 16 complications (2.27%). Minor complications (1.9%) were two cases of middle concha luxation; six cases of partial middle turbinectomy; five cases of damage to the papyraceous lamina, and one case of damage to the anterior ethmoid artery. Major complications (0.3%) were one case of iatrogenic fistula and one case of intra-operative death caused by acute myocardium infarction (Table 3).
Graph 4. Combined access to FESS.
TABLE 3 - Complications of FESS.
DISCUSSION
Functional endoscopic sinuses surgery (FESS) has been widely used because it enables a more anatomical access to the paranasal sinuses and preserves its physiology. Initially, it had restricted and limited indications, such as treatment of chronic sinusitis. As time went by, indications were diversified and other pathologies, such as nasal polyposis, choanal atresia, dacryocystitis, recurrent epistaxis, CSF fistula and tumors, were also included. This fact may be illustrated by our sample, showing an array of affections approached by FESS in our service and described in Table 1.
The procedure may be performed under general or local anesthesia, with sedation'. Surgeries under local anesthesia enable better distinction between normal and abnormal mucosa, and transoperative pain is a warning sign to avoid complications 17. Fedok et a1.4 concluded that the advantages of the use of local anesthetics in selected patients are shorter surgical time and lower frequency of nausea, vomiting and epistaxis, when compared to general anesthesia. In procedures under general anesthesia, there are more cases of hemorrhage, because of the vasodilatation effects. The advantages of general anesthesia are reduction of patient's anxiety, better pain and movement control, and more comfort for the surgeon17. Among the procedures performed in our service, 99.2% were conducted under general anesthesia. We observed severe bleeding in 7.4% of the cases, all performed under general anesthesia, and among them, 60% were conducted with associated Caldwell-Luc access. In all cases conducted under local anesthesia, bleeding was considered mild.
Excellent hemostasis and visibility are key for the success of FESS. The use of vasoconstrictors in the nasal mucosa allows reduction of bleeding and more visibility during the procedure. Wolfgang et al.17 used topical vasoconstriction with adrenaline at 1:1,00 concentration and concluded that systemic absorption of epinephrine is minimal, because of the intense vasoconstriction of the mucosa, preventing the elevation of serum levels. In our service, we use topical adrenaline at 1:2,000 concentration for vasoconstriction as a routine, and we believe that this is the reason why we found low incidence of severe bleeding (7.4%). In early post-operative, we applied finger glove nasal packing in 3.3% of the patients, and anterior-posterior packing in only one case.
Cardiovascular toxic effects of adrenaline (arrhythmia, tachycardia, hypertension) are maximized by the use of halogen anesthetic agents (such as halotane). These agents maximize the sensitivity of the myocardium for the effects of adrenaline. After the introduction of propofol, volatile anesthetics were abandoned in some services. Enflurane and isoflurane minimize the adverse cardiac effects related to adrenaline; therefore, the effects became very rare17.
Among the combined surgeries, Caldwell-Luc access was performed in 3.82 % of the cases. Despite the development of FESS, Caldwell-Luc indications still include: exeresis or biopsy of supposedly malignant maxillary sinus tumors, fungal sinusitis, multiple septated antral lesions, antrochoanal polyp, reduction of orbital or zygomatic fractures, closure of oroantral fistulas, and removal of foreign bodies18. Among the 27 combined surgeries with Caldwell-Luc access, 13 (48.15%) were for polyposis. Septoplasty was the most frequently used combined surgery (3.97%), because septal deviations restrict the access via endoscopy and the correction becomes imperative.
We had a low rate of complications, in 2.27% of the surgeries. Gross et al.5 observed that complication rates of endoscopic surgeries in a program of medical residence were 15.9% higher than in a service without medical residence (8%). The authors also observed that complications in the first service were considered minor (synechiae, minor hemorrhages, exposure of orbital fat and infections). Major complications, apart from death, are intracerebral hemorrhage, CSF fistula, amaurosis, diplopia, meningitis and severe hemorrhage. In our service, major complications were infrequent (0.3%) when compared to other services with and without medical residence (0.7% and 1.1%, respectively). All the residents in our service dissect at least 20 nasal fossae before they perform their first FESS.
CONCLUSION
In our experience, FESS has shown to be an effective method because it provided a procedure to approach different pathologies and enabled preservation of the nasal anatomy and physiology, presenting low complication rates.
REFERENCES
1. BAILEY, B. J.; PILLSBURG, H. C.; DRISCALL, B. E -Head and Neck Surgery-Otolaryngology, Second Edition, Chapters 35, 36, 37; 1998.
2. DAVID, L. et al. - The Role of Second-Look Nasal Endoscopy After Pediatric Functional Endoscopic Sinus Surgery. Arch Otolaryngol Head and Neck Surg., 124: 425-428, 1998.
3. DAVID, S. et al. - Functional Endoscopic Sinus Surgery Outcomes for Contact Point Headaches. The Laryngoscope, 108: 696-702, 1998.
4. FEDOK, F. G. et al. - Operative Times, Postanesthesia Recovery Times, and Complications During Sinonasal Surgery Using General Anesthesia and Local Anesthesia With Sedation. Otolaryngol Head and Neck Surg., 122(4); 560-566, 2000. .
5. GROSS, R. D.; SHERIDAN, M. F.; BURGESS, L. E Endoscopic Sinus Surgery Complications in Residency. Laryngoscope, 107: 1080-1085, 1997.
6. HARTIKAINEN, J. et al. - Prospective Randomized Comparison of Endonasal Endoscopic Dacryocystorhinostomy and External Dacryocystorhinostomy Laryngoscope, 108: 1861-1866,1998.
7. HASSAN, H. et al. - Surgical Causes of Failure in Endoscopic Sinus Surgery. Laryngoscope, 109: 27-29, 1999.
8. JOE, J. K. - Documentation of Variations in Sinonasal Anatomy by Intraoperative Nasal Endoscopy Laryngoscope, 110(2Pt1): 229-235, 2000.
9. KLOSSEC, J. M. et al. - Diffuse Nasal Polyposis: Postoperative Long-term Results After Endoscopic Sinus Surgery and Frontal Irrigation. Otolaryngol Head and Neck Surg., 117(4): 355-361, 1997.
10. RAMADAN, H. H. - Nonsurgical Versus Endoscopic Sinonasal Surgery for Rhinogenic Headache. Am J. Rhinol., 13(6): 455-457, 1999.
11. RON, L. M. et al. - Revision Endoscopic Sinus Surgery: The Thomas Jefferson University Experience. Ear, Nose and Throat J, 77(3): 190-202, 1998.
12. STAMMBERGER, H. et al. - Functional Endoscopic Sinus Surgery - The Messerklinger Technique. Philadelphia, BC Decker, 1991.
13. STAMMBERGER, H. - Possibilities and Limitations of Endoscopic Management of Nasal and Paranasal Sinus Malignancies. Acta Otorhinolaryngol Belg., 53(3): 199-205, 1999.
14. STAMMBERGER, H. - Surgical Treatment of Nasal Polyps: Past, Present and Future. Allergy, 54 (Suppl53): 711, 1999.
15. VOEGELS, R. L. - Cirurgia endoscopica dos seios paranasais. Arquivos da Fundação Otorrinolaringologia, 1(1):1997.
16. WINSTEAD, W - Impact of Endoscopic Sinus Surgery on Global Health Perception: An Outcome Study. Otolaryngol Head and Neck Surg., 119(5): 486-491, 1998.
17. WOLFGANG, A. et al. - Plasma Adrenaline Concentrations During Functional Endoscopic Sinus Surgery. Laryngoscope, 109: 204-207, 1999.
18. YANAGISAWA, E. - The Caldwell-Luc Procedure: Is It Still Indicated in this Endoscopic Sinus Surgery Era?; Ear, Nose and Throat J., May: 294-296, 1997.
* Postgraduate Physician, Division of Clinical Otorhinolaryngology, Hospital das Clínicas, Faculdade de Medicina da Universidade de São Paulo.
** Resident Physician, Division of Clinical Otorhinolaryngology, Hospital das Clínicas, Faculdade de Medicina da Universidade de São Paulo.
*** Intern Physician, Division of Clinical Otorhinolaryngology, Hospital das Clínicas, Faculdade de Medicina da Universidade de São Paulo.
**** Ph.D., Professor, Discipline of Clinical Otorhinolaryngology, Hospital das Clínicas, Faculdade de Medicina da Universidade de São Paulo.
***** Associate Professor, Discipline of Otorhinolaryngology, Faculdade de Medicina da Universidade de São Paulo.
Study conducted at the Division of Clinical Otorhinolaryngology, Hospital das Clínicas, Faculdade de Medicina da Universidade de São Paulo.
Study presented at 35° Congresso Brasileiro de Otorrinolaringologia, held on October 16-20, 2000, in Natal/RN.
Address correspondence to: Marcus Miranda Lessa-Divisão de Clínica Otorrinolaringológica - Hospital das Clínicas - FMUSP - Avenida Dr. Enéas de Carvalho Aguiar, 255 - 6° Andar, Sala 6167 - 05403-000 São Paulo/SP - Tel: (55 11) 3069-6288-Fax: (55 11) 280-0299-E-mail: marcusmlessa@hotmail.com
Article submitted on February 6. 2001. Article accepted on March 9. 2001.