Year: 2001 Vol. 67 Ed. 2 - (21º)
Relato de Casos
Pages: 274 to 278
Endoscopic Repair of Encephaloceles and Cerebrospinal Fluid Fistulae.
Author(s):
Daniel C. Pinheiro*,
Ricardo C. Demarco**,
Wilma T. Anselmo Lima***.
Keywords: CSF leak, sodic fluorescein, endonasal endoscopic surgery
Abstract:
Rhinogenic cerebrospinal fluid fistulae are potentially lethal and surgical treatment is indicated. Affected patients may evolve to repetition meningitis and brain abscess. Early diagnosis as well as the choice of the best surgical approach with minor morbidity must be instituted. Three cases cases are presented from the Hospital das Clinicas de Ribeirao Preto, two of them of patients with meningocele, treated by nasal endoscopic surgery, with the use of a hypodence solution of sodium fluorescein. The surgical approach showed to be effective for all cases and the intrathecal injection of the sodium fluorescein hypodense solution made easier as much the diagnosis as the approach of die fistulous sites, what avoided the Tredenlenburg positioning of patients, as well as the delay of hours before the start of surgical procedure.
![]()
INTRODUCTION
Persistent cerebrospinal fluid fistulae are potentially fatal and surgical treatment is indicated. Patients affected may progress into episodes of repetitive meningitis and cerebral abscesses if they are not properly intervened. Early diagnosis and appropriate selection of surgical technique aimed at low morbidity should be encouraged1.
For a long time, authors have discussed what the best approach to CSF rhinorrhea and nasal meningoceles was; there is a consensus, however, about the potential to complications of intracranial approach. Thanks to the advance of the modern nasal endoscopic technique developed by Messerklinger, associated with the use of intrathecal sodium fluorescein, identification and surgical approach of patients with these affections have become easier. The inconvenience of waiting some hours after the injection of diluted fluorescein in CSF, reported by some surgeons, may be avoided by diluting it into twice distilled water (hypotense solution); in addition, it maximizes the effect of the injection and does not require position of Trendelenburg, even in cases of low output fistulae5.
We presented three patients with CSF rhinorrhea treated at Hospital das Clínicas, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo, submitted to nasal endoscopic surgery in the year 2000.
CASE REPORT
Case 1
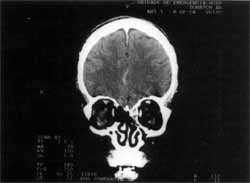
Female, 46-year-old patient, born in Passos/MG, professional clothes washer. She was referred to the ambulatory of Otorhinolaryngology because of intermittent unilateral hyaline rhinorrhea on the left, of sudden onset eight years before. She also reported frontal-occipital headache. She did not refer history of cranial traumas or repetitive meningitis. The analysis of nasal secretion showed 40mg protein by 100ml and 58mg glucose by 100m1. Nasofibroscopic exam with rigid optic fiber at 0° showed bowing of left sphenoethmoid recess, with CSF drainage at Valsalva maneuver, as well as exposure of dura mater, suggestive of meningoceles. Cisternography confirmed the diagnostic hypothesis, showing a CSF fistula through discontinuity of cribrosa lamina on the left, close to crista galli (Figure 1). Based on the diagnosis of anterior cranial fossa meningoceles we indicated nasal endoscopic surgery to resolve the condition.
Case 2
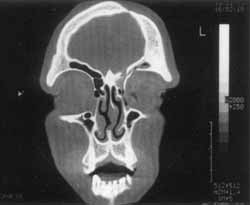
Male 29-year-old patient, born in Morro Agudo/SP, agriculture worker. He was referred to the ambulatory of Otorhinolaryngology to confirm hypothesis of repetitive meningitis. He reported four episodes of bacterial meningitis in the previous 9 years, presenting intermittent unilateral rhinorrhea on the right, associated with frontal and parietal headache for a long time. He did not report cranial trauma. CT scan of paranasal sinuses revealed bone discontinuity of anterior cribrosa plaque on the right, frontal-ethmoidal velamentum on the right and image suggestive of retention cysts in the right maxillary sinus (Figure 2). The analysis of nasal secretion showed 84mg of glucose by 100m1, suggesting cerebrospinal fluid. Nasofibroscopy with optic fiber at 0° showed bowing of cribrosa lamina on the right, drainage of hyaline secretion, in addition to high septal deviation to the right. Based on the diagnosis of nasal meningoceles, we indicated surgical correction via nasal endoscopy.
Figure 1. CT scan with contrast showing discontinuity of cribrosa lamina on the left, close to crista galli, with overflow of contrast (case 1).
Figure 2. CT scan showing bone discontinuity on anterior cribrosa plaque on the right and frontal ethmoid velamentum on the right (case 2).
Figure 3. CT scan showing fracture of the roof of orbit and posterior wall of frontal sinus on the left (case 3).
Case 3
Male 24-year-old patient, born in Barrinha/SP, was referred by the Neurosurgery Department with a history of cranial trauma caused by car accident nine years before. The patient had been submitted to craniotomy and drainage of clot in the frontal region. He also reported three episodes of bacterial meningitis after that period. The patient complained of frontal-parietal headache on the left and aqueous rhinorrhea on the left nasal fossa. Nasofibroscopy with 0° and 30° fiber optic showed high septal deviation to the right, no evidence of bowing or CSF drainage. Paranasal sinuses CT scan showed evidence of frontal left craniotomy, fracture of the roof of orbit and the posterior wall of frontal sinus on the left (Figure 3). After the injection of contrast, we observed CSF leak through the fracture of the posterior wall of frontal sinus. Based on the diagnosis of CSF rhinorrhea in the frontal sinus post-cranioencephalic trauma, we indicated endoscopic surgical correction of the case.
Description of the surgical technique
We initially conducted lumbar puncture during anesthetic induction, followed by injection of solution of sodium fluorescein at 0.1ml for each 10Kg of weigh, respecting the maximum dosage of 1ml of solution. We decided to dilute the solution in l0ml of twice distilled water, transforming it into a hypotense solution; therefore, we did not have to wait for one hour or more to start surgery, nor needed Trendelenburg's position, according to Guimarães5. Thus, it was easier to find the fistula site by the yellow greenish color characteristic of CSF stained by the solution. We then proceeded with the exploration of the condition using rigid 4mm-endoscopes at 0° and 30°, followed by cauterization and resection of meningoceles (cases 1 and 2). The fistula site was isolated and sealed with mucoperiosteum of the middle concha removed from the patient, followed by its fixation with fibrin glue (Tissucol®) and lined with Surgicel®. Nasal cavity was packed for 14 days. Prophylactic antibiotic therapy was recommended in all patients, including 1g endovenous ceftriaxone, single daily dose for 3 days, plus oral amoxicillin at therapeutic doses until removal of nasal packing. During lumbar puncture, we collected 3ml of CSF before the surgery to conduct bacterioscopic and culture analyses. In case 3, endoscopic approach had to be complemented by external access to the frontal sinus (Linch's incision), because it was difficult to access the fistula site.
We did not experience intra or post-operative complications caused by the surgical procedure or the lumbar puncture. In case 2, anatomic pathological analysis revealed astrocytes and neuronal cells confirming the diagnosis of meningoencephaloceles. We succeeded in closing the fistulae of the three cases and in resolving the cases' of meningoceles and meningoencephaloceles.
DISCUSSION
Cerebrospinal rhinorrhea may be traumatic or spontaneous, but the majority of the cases is traumatic and may be caused by accident or iatrogenic episodes14. In our sample, two of them were classified as spontaneous and one was the result of a trauma.
Among post-trauma CSF leaks iatrogenic affections are common, considered the most frequent severe complications after nasosinusal endoscopic surgery. In this group, the most common affected sites are cribrosa plaque, ethmoid fovea, sphenoid sinus and frontal sinus14.
Diagnosis depends on clinical history: the patients normally report intermittent unilateral hyaline rhinorrhea. We should always ask about previous cranial trauma. Other important complaints are headache and post-nasal dripping. Repetitive meningitis is also common and it may be the first clinical manifestation of patients with CSF leak. Cases 2 and 3 presented repetitive meningitis, which facilitated diagnosis.
As complementary diagnostic methods, high resolution CT scan, cisternography and MRI may be useful. Protein electrophoresis of nasal secretion and glucose dosage above 30mg per 100ml may ratify the diagnosis. Recently, dosage of P-2-transferrin by electrophoresis of immunofixation, a protein produced by active neuroaminidase in the brain, has also been investigated, because it is present in CSF and perilymph and its presence in nasal secretion confirms the diagnosis of CSF leak11.
In the past, these affections were treated with craniotomy with intradural repair. Thanks to the advent of nasal endoscopic surgery, transnasal repair has become more frequent8,9. Low morbidity and high success rates with endoscopic technique have made it the preferred treatment for CSF rhinorrhea. However, the technique is not 100% free of complications. Intrathecal fluorescein injections are associated with severe complications in a number of cases, such as limb paresia, paralysis, seizure, opisthotonus and alterations of cranial nerves1,10. Intracranial mucoceles and chemical encephalitis are other rare but potentially fatal complications described by the literature15.
The need for post-op lumbar drainage is another controversial issue in this surgical technique. Cassiano et al. (1999) reported 33 patients treated with endoscopic nasal surgery without lumbar drainage, including cases of 3cm fistula, and they concluded that routine lumbar drainage is not necessary, and surgical success is not related to the output of the fistula2. Among the cases reported here, no patient required post-op lumbar drainage.
Materials used to close the bone failures in the skull base vary a lot, but they normally produce good results. The use of middle turbinate mucosa may be substitute by septal cartilage, mucoperiosteum of inferior turbinate, muscles, bone fragments, omentum flap, associated or not to fibrin glue, Gelfoam® or Surgicel®4,5,6,7,12,13.
CONCLUSION
Endoscopic treatment of CSF rhinorrhea, as well as nasal meningoencephaloceles, has become attractive because it has high success rates and low morbidity. In our experience, it was effective in all cases and it is considered the preferred treatment option for such cases. Despite the small number of cases and the maximum follow-up of 6 months, it is important to notice from our study that intrathecal injection of hypotense solution of sodium fluorescein is a safe procedure and it facilitates diagnosis and the approach of CSF leaks.
REFERENCES
1. BAILEY, B. J. - Read and Neck Surgery-Otolaryngology, Lippincott-Raven, 2ª edition, 1998.
2. CASSIANO, R. R.; JASSIR, D. - Endoscopic cerebrospinal fluid rhinorrhea repair: is a lumbar drain necessary? Otolaryngol. Head Neck Surg., 121 (6): 745-50, 1999.
3. CUMMINGS, C. W; FREDRICKSON, J. M.; HARKER, L. A.; KRAUSE, C. J.; RICHARDSON, M. A.; SCHULLER, D. E. Otolaryngology & Head Neck Surgery Review. Mosby, 1998.
4. GJURIC, M.; GOEDE, U.; KEIMER, H.; WIGAND, M. E. Endonasal endoscopic closure of cerebrospinal fluid fistulas at the anterior cranial base. Ann. Otol. Rhinol. Laryngol., 105 (8): 620-3, 1996.
5. GUIMARÃES, R. E. S. - Reparação Microendoscópica da Rinoliquorréia. In: Stamm, A. Rinologia 2000, Revinter, 2000, 401-402.
6. HUGHES, R. G.; JONES, N. S.; ROBERTSON, I. J. - The endoscopic treatment of cerebrospinal fluid rhinorrhea: the Nottingham experience. J. Laryngol. Otol. Fev., 111(2): 1258, 1997.
7. KELLEY, T. F.; STANKIEWICZ, J. A.; CHOW, J. M.; ORIGITANO, T C.; SHEA, J. - Endoscopic closure of post-surgical anterior cranial fossa cerebrospinal fluid leaks. Neurosurgery, 39 (4): 743-6, 1996.
8. LANZA, D. C.; O'BRIEN, D. A.; KENNEDY, D. W Endoscopic repair of cerebrospinal fluid fistulae and encephaloceles. Laryngoscope, 106 (9): 1119-25, 1996.
9. MARKS, S. C. - Middle turbinate graft for repair of cerebral spinal fluid leaks. Am. J Rhinol, 12 (6): 417-9, 1998.
10. MAY, M.; LEVINE, H. L.; MESTER, S. J.; SCHAITKIN Complications of endoscopic sinus surgery: analysis of 2,108 patients-incidence and prevention. Laryngoscope, 104 (9): 1080-3, 1994.
11. NORMINGTON, E. Y; PAPAY, F. A.; YETMAN, R. J. Treatment of recurrent cerebrospinal fluid rhinorrhea with a free vascularized omental flap: a case report. Plast. Reconstr Surg., 98 (3): 514-9, 1996.
12. SCHIEVINK, W L; MORREALE, V M.; ATKINSON, J. L.; MEYER, F. B.; PIEPGRAS, D. G.; EBERSOLD, M. J.- Surgical treatment of spontaneous spinal cerebrospinal fluid leaks. J Neurosurg. Feb.; 88 (2): 243-6, 1998.
13. VOEGLES, R. L.; SANTORO, E E; MEDEIROS, I. R. T; BUTUGAN, O. - O use da Fluoresceina Sódica no Tratamento Endoscópico das Fistulas Liquóricas Rinogênicas. Rev. Bras. Otorrinolaringol. 65 (4): 326-330, 1999.
14. WANG, L.; KIM, J.; HEILMAN - Intracranial mucoceles as a complication of endoscopic repair of cerebrospinal fluid rhinorrhea: case report. Neurosurgery, 45 (5): 1243-5, 1999.
15. WETMORE, R. F.; DUHAIME, A. C.; KLAUSNER Endoscopic repair of traumatic CSF rhinorrhea in a pediatric patient. Int. J Pediatr Otorhinolaryngol., 36 (2): 109-15, 1996.
* Resident Physician of Otorhinolaryngology at Hospital das Clínicas, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo.
** Assistant Physician of Hospital das Clínicas, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo.
*** Professor, Ph.D., Department of Ophthalmology and Otorhinolaryngology at Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo.
Study conducted at the Department of Ophthalmology and Otorhinolaryngology at da Faculdade de Medicina de Ribeirão Preto, Univasidade de São Paulo.
Address for correspondence: Professora Wilma T Anselmo-Lima - Departamento de Oftalmologia a Otorrinolaringologia da Faculdade de Medicina de Ribeirão Preto.
Avenida Bandeirantes, 3900 - 14049-900 Ribeirão Preto/SP
Tel: (55 16) 602-3000 - Fax: (55 16) 633-1586.
Article submitted on August 4. 2000 l. Article accented on September 28 2000