Year: 2001 Vol. 67 Ed. 1 - (14º)
Artigos Originais
Pages: 90 to 93
National Voice Week: Descriptive Study of 451 Patients.
Author(s):
João B. Ferreira*,
Diogenes S. Ferreira**.
Keywords: voice, hoarseness, laryngeal diseases
Abstract:
Introduction: The National Voice Week, which took place between April 12th and 16th, 1999, became the first large event related to the importance of the phonatory function aimed to the Brazilian population. Aim: To present the data obtained from 451 consultations, without further diagnostic exams, in the Otolaryngology Division of the Department of Surgery of the UFG Medical School during the National Voice Week. Material and method: Four hundred and fifty one patients were initially interviewed by speech therapists who filled in a form for each one of them. Each patient was then interviewed by an otolaryngologist and examined by the conventional method, indirect laryngoscopy, and oriented. Results: Among 451 patients, 350 (77,60%) had two symptoms, 93 (20,62%) had only one and 8 (1,78%) had no complaint. The most frequent symptoms were: hoarseness, in 262 patients (58,09%); sore throat, in 260 patients (57,65%) and cough clearing, in 260 patients (57,65%). After the otolaryngological examination, 270 patients (59,87%) had no evidence of vocal, pharyngeal, laryngeal or regional alterations; 87 patients (19,29%) had evidence of such alterations and it was not possible to assure if there were alterations in 94 patients (20,84%). Among the 87 patients that had evidence of alterations, 51(11,31%) had laryngeal alterations (functional or organic) , and 2 (0,44%) of these were suspect of malignancies. Conclusion: Among 451 patients interviewed and examined during the event, 51 (11,31%) showed clinical evidence of alterations located in the larynx, and 2 (0,44%) of these were suspect of malignancies.
![]()
INTRODUCTION
The National Week of Voice was a campaign conducted between 12 and 16 April 1999 and it was the first large coverage event directed to the Brazilian population addressing the importance of phonation and voice care. It was promoted by the Brazilian Society of Otorhinolaryngology - SBORL, and the Brazilian Society of Laryngology and Voice - SBLV. This study is a result of the participation in the event of the Service of Otorhinolaryngology at Faculdade de Medicina, Universidade Federal de Goiás and the speech pathologists. It was based on the guidelines of the campaign, including clinical management with screening, ENT exam and counseling of patients. Owing to limitations inherent to the set of actions programmed and the dynamics necessary for individual management, definite diagnoses were not reached, excluding etiological, anatomical and functional diagnoses³.
The study aimed at presenting the results obtained in 451 visits, without complement exams, at the Service of Otorhinolaryngology, Faculdade de Medicina, Universidade Federal de Goiás during the National Week of Voice.
MATERIAL AND METHOD
The total number of evaluated subjects was 451 people, seen at the Service of Otorhinolaryngology, Faculdade de Medicina, Universidade Federal de Goiás, during the National Week on Voice campaign. Patients underwent a screening protocol with speech and voice pathologists. An anamnesis form created for the campaign was filled in manually for each patient including the following items: identification, complaint or reason for visit (sore throat, dysphagia, hoarseness, throat clearing, changed voice, etc.), duration and persistence of symptoms, frequency, vocal abuse/fatigue, risk factors (alcohol use, smoking, pollution), and perceptual voice assessment (adapted, hoarse, harsh, breathy, bitonal, inadequate for gender and age). After the opinion of the speech and voice pathologists about evidence of vocal and/or laryngeal and pharyngeal alterations, the patient was seen by the Otorhinolaryngologist and examined according to the conventional exam - indirect laryngoscopy. The exam was conducted with photophore, spatula and Garcia's mirror. Local anesthesia of pharyngolaryngeal mucosa was made if necessary, using lidocaine 10%, applied in 2 or 3 nebulations, to avoid nausea reflex. The exam was based on the observation of the items in the form: 1) No evidence of vocal and/or pharyngeal/laryngeal or regional alteration, 2) There was evidence of vocal and/or pharyngeal and laryngeal or regional alteration (pre-neoplasia, benign or malignant neoplasia). After laryngoscopy patients were submitted to professional counseling. Based on the information collected from the forms, we created a computed database using the software EpiInfo version 6.04 and the variables were analyzed using frequency tables of the software Analysis.
RESULTS
Among 451 patients seen, 301 (66.74%) were female and 150 (33.26%) were male subjects, aged from 3 to 90 years and with 86 different occupations. Distribution of patients by age ranges is shown in Table 1.
The most frequent occupations or professions were housewife, 109 (24.17%); student, 38 (8.42%); dressmaker, 15 (3.32%); teacher, 13 (2.88%); civil servant, 11 (2.44%) and salesperson, 11 (2.44%). Among the less frequent professions, there were two singers (0, 44%).
Out of the total number of patients, 89 (19.73%) said that they used their voice professionally.
Three hundred and fifty patients (77.60%) reported two or more complaints; 93 (20.62%), only one complaint; and A (1.78%) did not refer any complaint. The frequency of complaints were: hoarseness, 58.09%; sore throat, 57.65%; throat clearing, 57.65%; changed voice, 23.50%; dysphagia, 20.18%; and other complaints, 22.39%.
Duration of symptoms: 337 cases (74.73%) for more than 6 months; 89 cases (19.73%), between 3 weeks and 6 months; and 25 cases (5.54%) for less than 3 weeks. Symptoms were frequent in 178 patients (39.47%), persistent in 148 (32.82%), occasional in 103 (22.84%) and rare in 22 patients (4.87%).TABLE 1 - Distribution of patients by age range.
Key: * Cumulative relative frequency.
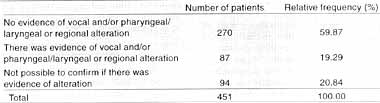
TABLE 2 - Results of ENT exams.
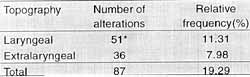
Table 3 - Results of frequency of laryngeal and extralaryngeal alterations.
Key: * Two cases suggestive of malignant nepplasia.
Patients that had already participated in the campaign amounted to 194 people (43.01%).
One hundred and fifty-six people referred voice abuse (34.59%). Among them, 81 (51.92%) had frequent abuse, 40 (25.64%) had persistent abuse, 28 (17.95%) occasional abuse and 7 (4.49%) rare abuse.
As to life habits, 159 people (35.26%) were smokers or users of alcohol. Among them, 86 (19.07%) were smokers and 73 (16.19%) were alcohol users, and 31 (6.87%) were both smokers and alcohol users. Patients that reported exposure to polluted environment amounted to 184 people (40.80%).
Among women, 51(16.94%) were smokers, 29 (9.63%) were alcohol users and 13 (4.32%) were smokers and alcohol users. Among men, 34 (22.67%) reported smoking, 43 (28.67%) reported alcohol abuse and 18 (12.00%) had both habits.
Based on the vocal perceptual assessment, 265 people (58.76%) had adapted voice, 129 (28.60%) hoarse voice, 16 (3.55%) harsh voice, 4 (0.89%) bitonal voice, 3 (0.67%) breathy voice, 2 (0.44%) inadequate voice for gender, 2 (0.44o/o) inadequate voice for age and 30 people (6.65%) had no register in their form.
According to the forms of initial screening .conducted by voice therapists, 280 patients (62.08%) had evidence of vocal and/or pharyngeal/laryngeal alterations, 147 (32.60%) did not have evidence and 24 (5.32%) were not defined.
After the ENT exam, in 270 cases (59.87%) there was no evidence of vocal and pharyngeal/laryngeal or regional alteration, in 87 cases (19.29%) there was evidence and in 94 cases (20.84%) it was not possible to confirm the existence of alteration (Table 2). Among the 87 patients with evidence of alteration, 51 (11.31%) had laryngeal alterations (organic or functional), and, among them, 2 (0.44%) were indicative of malignant neoplasia at indirect laryngoscopy. The remaining 36 patients (7.98%) presented evidence of extralaryngeal alterations (Table 3).
DISCUSSION
This study showed the result of part of the service provided at the National Week on Voice at state level, because it corresponds only to the visits of patients to the service of Otorhinolaryngology at Faculdade de Medicina, Universidade Federal de Goiás.
The larynx is the adequate organ for respiratory and phonation functions, maintaining a very close anatomicaltopographic and functional relation with the pharynx (breathing and swallowing). Similarly to other organs, it may be where many affections lie, as seen in practice, and in the literature 1,5,4. A number of alterations, such as congenital, infectious, traumatism, benign and malignant tumors, immunodeficiency and allergy are known, as well as all the risk factors (alcohol use, smoking, pollution) and some triggering factors such as vocal misuse or abuse, in addition to other environmental factors. The symptoms, as a consequence, are dysphonia, dyspnea, cough, sensitivity and mobility disorders (pain, paresia, paralysis), dysphagia², and aspiration, among others, are equally known. Treatment of laryngeal disorders should be preceded of diagnosis based on anamnesis, clinical picture, complete ENT exam, and complementary exams. Part of the population with laryngeal disorders in the presence of symptoms (early or late) or voluntarily exposed to risk factors, do not search for medical support within reasonable time.
In our sample, we noticed that about two thirds of the 451 patients were female. Patients of different age ranges also came to the ambulatory, from 3 years to 90 years. The largest number of patients (23.50%) was concentrated on the age range of 41 to 50 years, whereas the smallest (0.89%) was between 81 and 90 years. We noticed that the search for medical treatment was ascending from the first to the fifth decades and descending from the fifth to the ninth decades.
Among the 86 different occupations, the most frequent was that of housewife. More than three quarters of the evaluated patients (77.60%) reported two or more complaints, and about one fifth (20.62%) had only one complaint; eight patients (1.78%) came to the service without any specific complaint.
As to frequency of complaints, hoarseness (58.09%), sore throat (57.65%), throat clearing (57.65%) were the most common, followed by changed voice (23.50%) and dysphagia (20.18%), plus other complaints (22.39%).
We would like to point out that a myriad of complaints was described and it was sometimes difficult for the patient to define the main one. It is thought that maybe this difficulty derived from the fact that the patients were making reference to the campaign that stressed the importance of voice care and emphasized all possible symptoms, encouraging people to come to the exams.
As to duration of symptoms, the most frequent ones were referred for more than 6 months in 337 cases (74.73%). Subjectively, 39.47% of the patients said they had frequent symptoms, 32.82% said persistent, 22.84%, occasional and 4.87% said symptoms were rare.
It is important, to highlight the number of people that had risk factors: out of 451 patients, 159 (35.26%) of the patients were smokers and/or users of alcohol, and 40.80% were exposed to polluted environments.
In the perceptual assessment conducted by voice pathologists, 265 patients (58.76%) had adapted voices and in 129 (28.60%) the voice was hoarse. In the others, 16 (3.55%) had harsh voice, 4 (0.89%) had bitonal voice, 3 (0.67%) had breathy voice, 2 (0.44%) had inadequate voice for gender and 2 (0.44%) had inadequate voice for age.
Based on the results it was possible to conclude that there were disagreements between what was reported as symptomatology by the population and the subjective opinions made by the professionals about evidence or not of vocal and/or laryngeal/pharyngeal alterations and the results after the ENT exam. We should consider the obstacles expected in such a campaign, the involvement of population and professionals and the limitations of clinical management defined under such conditions.
Once carried out the exam by the Otorhinolaryngologist with indirect laryngoscopy, we noticed that more than half of the 451 patients (49.87%) did not have evidence of alterations and in 20.84% it was not possible to confirm the evidence. Among 87 patients (19.29%) with evidence of alterations, 51 (11.31%) were classified as having some kind of organic or congenital alterations observed in the topography of the larynx (vocal fold nodule, polyp, cyst, acute/chronic laryngitis, leukoplasia, Reinke's edema, alteration of mobility - vocal fold paresia and paralysis, in addition to others); among them, 2 patients (0.44%) had alterations suggestive of laryngeal malignant neoplasia. Thirtysix (7.98%) of the 87 patients had extralaryngeal alterations (pharyngitis, tonsillitis, peritonsillar abscess, goiter, cleft palate, among others).
CONCLUSION
Among 451 patients seen at the campaign, 87 (19.29%) presented clinical evidence of vocal and/or laryngeal/pharyngeal or regional alterations, and 51 (11.31%) were located in the larynx, being that 2 of them (0.44%) were suggestive of malignant neoplasia.
REFERENCES
1. BEHLAU, M.; PONTES, P. - Avaliação a tratamento das disfonias. São Paulo, Lovise, 1995, 17-312.
2. BRETAN, O.; TAGLIARINI, J. V. - Investigação clínica da disfagia orofaríngea. Rev. Bras. ORL, 64(4): 320-324, 1998.
3. FARAJ, M.; FREIR, P. C.; COPPOLI, A. B. R. - O papel da propedêutica na medicina contemporânea. JBM, 77(1):1220, 1999.
4. FORD, C. N. et al. - Anterior commissure micronodules associated with vocal nodules: Detection, prevalence and significance. Laryngoscope, 104(17): 1369-1375, 1994.
5. SENNES, L. U.; TSUJI, D. H.; GUIMARAES, J. R. R. - Câncer da laringe: Diagnóstico a tratamento. Arquivos da Fundação Otorrinolaringologia, 2(2): 62-68, 1998.
* Ph.D. Joint Professor of the Service of Otorhinolaryngology at Faculdade de Medicina da Universidade Federal de Goiás.
** Undergraduate at School of Medicine, Universidade Federal de Goiás.
Study conducted at the Service of Otorhinolaryngology Faculdade de Medicina da Universidade Federal de Goiás.
Address for correspondence: João Batista Ferreira - Avenida R-9, 30 - Setor Oeste - 74125-110 Goiânia /GO - Tel/ Fax: (55 62) 291-2944.
Article submitted on May 9. 2000. Article accepted on November 6, 2000.