Year: 2001 Vol. 67 Ed. 1 - (3º)
Artigos Originais
Pages: 22 to 27
Permanence Time of 164 Ventilation Tympanic Tubes in 82 Cleft Palate Pacients.
Author(s):
Douglas S. R. Morales*,
José R. G. Testa**,
Arnaldo Guilherme***,
Yotaka Fukuda****.
Keywords: cleft palate, seromucinous otitis, ventilation tubes insertion
Abstract:
Introduction: Pacients with deft palates have seromucinous otitis media (OMS), that's considerate almost universal in cleft palate pacients. The cleft may be classified in: preforame, transforame and posforame. The OMS occours with bigger frequency in pacients with transforame and posforame clefts. Cleft palate pacients (CPP) are treated by a team of health profissionals; the otolaryngologist treat OMS, with a tympanotomy with a insertion of a ventilation tympanic tube. Objective: This work saw the permanence time of the tympanic tubes in pacients with cleft palate. Material and method: 164 ears (82 pacients) were analysed, with or without palate plastic surgery (PPS). Statisticiam tests (Kruskal Wallis, Whitney and Wilcoxon) were used to compare the diferents subgroups. Results: Pacients with PPS Nave the permanence time of the tympanic tube smaller than the pacients without PPS. When the permanence of the tympanic tube in pacients with unilateral transforame cleft were analysed, the tubes homo and ipsilateral weren't diferents. When we compared clefts uni and bilateral, the permanence time was superior in the group bilateral (with-or without PPS). We compared too transforame and posforame clefts; the time was superior in the group posforame (with and without PPS). We could look that the permanence time of the ventilation tympanic tubes in tympanic membrane was related to the local inflammatory process; than, that's events to facilite or prejudice this inflammatory process: the colocation of ventilation tympanic tubes permits the better draining of seromucinous secretion of the media ear; the PPS permits a mechanism of oppenig of the Eustachian tube, getting arise the oppenig of its cavity, due the action of the muscles tensor and elevator of the palate. Pacients with big clefts don't have stopped secretion in the nasopharynge. The permanence time of ventilation tubes the kind Armstrong in pacients with cleft palate was, in media, 223 and 279 days, when with and without PPS, respectely. Generally, the ventilation tympanic tube stayed at tympanic membrane for about 251 days in cleft palate pacients studied.
![]()
INTRODUCTION
Patients with cleft lips and palate, cleft lip or cleft palate should be followed since birth. According to Modolin et al. (1.988), among Caucasians, one in each 1,000 will have a congenital lip, palate or lip and palate cleft. The incidence is considerably lower among Black people and higher among Asians.
Patients with cleft lip and palate are followed by multidisciplinary teams and routinely managed by the otorhinolaryngologist, because there is high incidence of affections related to the specialty. Patients have difficulties to close completely the mouth and swallow; there may be nasal reflux of food and liquids. Upper and lower airways are affected, changing the physiology of breathing and swallowing. Speech is equally compromised, and they may present open rhinolalia, dysphonia and velopharyngeal insufficiency. We may also list alterations of occlusion and position of teeth, and normally there is also modification of nasal morphology. The abnormal function of Eustachian tube leads to otitis media (acute, repetitive, serous, chronic suppurative and cholesteatomatous) and conductive hearing loss. According to Oberascher and Albegger (1992), the typical symptom of serous otitis media (SOM) is conductive hearing loss. SOM is the presence of secretion (effusion) in the tympanic cavity and, according to Paradise (1976), it is known as a universal complication in patients with cleft palate. Doyle, Cantekim and Bluestone (1980) studied patients with cleft palate and concluded that children with this condition have reduced capacity to actively open the Eustachian tube, an evidence of their incapacity to balance positive and negative pressures.
Berlin et al. (1971) described the most used classification for study and treatment of these patients - Spina's classification, which takes into consideration embryogenesis and described post-foramen cleft, transforamen cleft (unilateral or bilateral), and pre-foramen cleft (unilateral or bilateral) (Figure 1).
Bluestone (1975) referred in his article that otitis media may be the result of a tubarian dysfunction, inflammation of middle ear or both. In patients with cleft palate obstruction is functional and it is related to the mechanism of opening of Eustachian tube, triggered by the veli palatini tensor muscle.
Becker, Naumann and Pfaltz (1994) referred that the treatment of these patients should involve a multidisciplinary team with otorhinolaryngologist, plastic surgeon, pediatrician, geneticist, orthodontist, dentist, speech and hearing pathologist, physical therapist, psychologist, nutritionist and social worker. Each team has an arsenal of specialized techniques for the treatment of cleft lip and palate. If there is cleft lip, correction is between the 3td and 6td months of life using the technique of primary lip reconstruction; sometimes it requires final surgical review, secondary procedure, conducted between the 14th and 16th months of life. Cleft palate (hard or soft) is corrected between the 4th and 9th months of life, named primary palate plastic surgery. A second surgery may also be required, secondary palate plastic surgery, to be conducted during the first year of life. If the nose requires rhinoplasty, it is normally recommended to wait until the 16th year of life. Orthodontic procedures, if necessary, are performed as from the 5th year of life. As to speech, 70% of them, succeed after these procedures. Some patients continue to have velopharyngeal insufficiency, requiring pharyngoplasty, whose main purpose is to restore the function of the short, immovable and insufficient soft palate closer to the normal range.
Figure 1. Ilustrative scheme of the different types of clef palate, including oronasal aspect and axial section at the level of the palate:A - left pre-foramen cleft, B - right pre-foramen cleft, C bilateral pre-foramen cleft, D - left transforamen cleft, E - right transforamen cleft, F - bilateral transforamen cleft, G -Post-foramen cleft.
Patients with cleft palate frequently have serous otitis media (Paradise, 1976) that are difficult to solve. Implantation of ventilation tubes is advocated in such cases, and longer lasting tubes, such as Armstrong type, are recommended (Quante, Esser e Strauss, 1976). Children submitted to tympanotomy with implantation of ventilation tubes present improvement of hearing loss, language delay and possible intellectual deficits (Paradise, 1976).
The management of cleft palate patients motivated the conduction of the present study with the purpose of measuring the permanence of Armstrong ventilation tubes in patients with post-foramen and transforamen clefts and to observe if there was relation between the side of the transforamen cleft and permanence of homolateral and contralateral ventilation tube.
MATERIAL AND METHOD
This study was carried out in Fundação para o Estudo das Deformidades Crânio-Faciais Foundation for the Study of Craniofacial Deformities, in its out-patient unit in São Paulo, where treatment of pre, post and transforamen cleft palate cases are provided. There were 191 patients aged between 4 months and 30 years. Eighty-two were surgically approached, and 56 were male and 26 were female patients. They were submitted to a research protocol analyzed and approved by the committee on ethics and research of Universidade Federal de Sao Paulo. Diagnosis of SOM was based on ENT exam, pure tone audiometry, speech discrimination and immitanciometry (tympanometry and stapedial reflex). These patients were submitted to unilateral or bilateral tympanotomy and placement of ventilation tubes (Armstrong) and followed for a period of one year. At the end of the study, the distribution was as follows:
• 84 patients who underwent bilateral ventilation tube placement had extruded them up to the last date of data collection; two of the patients had pre-foramen cleft and 82 had transforamen cleft (164 ears);
• 13 patients submitted to unilateral tympanotomy and extrusion of tube (13 ears);
• 4 patients submitted to placement of ventilation tubes bilaterally had extruded one tube and maintained the other (8 ears);
• 11 patients who had been submitted to bilateral placement of ventilation tubes and had not extruded any of them (22 ears);
• 9 patients submitted to placement of bilateral ventilation tube who had extruded one tube and maintained the other (18 ears);
• The remaining patients did not participate in this study because they had, been followed for less than one year (32 patients), did not fit the protocol (35 patients), abandoned treatment or had other facial malformations.
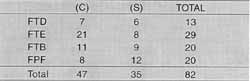
The 82 patients (164 ears) that were submitted to bilateral tympanotomy and had transforamen cleft were divided into the subgroups:TABLE 1 - Number of patients (82), according to location of cleft palate (right transforamen; left transforamen, bilateral transforamen; and post-foramen) - and presence of correction: (C) with and (S) without.
Key: FTD - right transforamen cleft; FTE - left transforamen cleft, FTB - bilateral transforamen cleft, FPF - Post-foramen cleft.
• Right transforamen cleft (FTD) (corrected and not corrected: 13 patients)
• Left transforamen cleft (FTE) (corrected and not corrected: 29 pattients)
• Bilateral transforamen cleft (FTB) (corrected and not corrected: 20 patients)
• Post-foramen cleft (FPF) (corrected and not corrected: 20 patients)
Therefore, the 82 patients were subdivided as shown in Table 1.
RESULTS
We recorded the permanence of ventilation tubes (Armstrong type) in patients with cleft palate, and the limits were the date of placement and of extrusion of tube. Based on these data, we observed, by using Wilcoxon statistical test, that permanence of ventilation tubes in patients with unilateral transforamen cleft did not differ from the homolateral or contralateral cleft situation; therefore, we analyzed them as a single group of unilateral transforamen cleft.
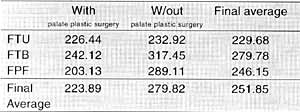
Table 2 is a result of the analysis of the average time of permanence of the ventilation tube (in days) in patients with unilateral transforamen cleft (FTU), bilateral transforamen cleft (FTB) and post-foramen cleft (FPF) compared to presence or absence of palate plastic surgery.
DISCUSSION
We analyzed 82 patients (164 ears) who had bilateral extrusion of middle lasting ventilation tubes (Armstrong type), and presented FTD, FTE, FTB and FPF. These groups of patients were subdivided as with or without palate plastic surgery (Table 1). The permanence of the ventilation tube in patients that had transforamen unilateral cleft (FTD or FTE) was grouped as homolateral and contralateral to the cleft side in patients that had undergone palate plastic surgery or not (Table 2). Wilcoxon statistical test was applied to the data of Table 2 and it did not show statistically significant difference between homolateral and bilateral columns, allowing grouping of them and maintaining the division of patients with unilateral transforamen cleft (FTD and FTE) submitted to palate plastic surgery and patients with unilateral transforamen cleft (FTD and FTE) who were not submitted to palate plastic surgery. This fact made us realize that anatomical abnormalities related to unilateral transforamen cleft result, functionally speaking, in the same affection for both ears, because the permanence of the ventilation tube in the tympanic membrane is associated with epithelial migration (Lopes Filho, 1984). Therefore, the inflammatory process generated by SOM effusion would be a local stimulating factor, resulting in faster epithelial proliferation. Since both the homolateral and contralateral sides did not present statistically significant differences, we noticed that the severity of affection is the same, despite the fact that the cleft palate is unilateral, different from what was found by Casselbrant et al. (1985) in studies with rhesus monkeys, in which they opened the palate and showed that the Eustachian tube on the open side had the function severely affected. This difference may be due to the fact that patients with cleft palate have already developed a mechanism of adaptation since birth, not being classified as an acute affection.TABLE 2 - Average of permanence of ventilation tube (in days) in patients with FTU, FTB and FPF, and presence of palate plastic surgery.
Key: FTU - unilateral transforamen cleft; FTB - bilateral transforamen cleft, FPF - Post-foramen cleft.
Despite the fact that we expected a difference between the average permanence of the ventilation tube in patients with unilateral transforamen cleft with palate plastic surgery and those without palate plastic surgery it was not observed: both groups were compared using Mann-Whitney statistical test and there was no statistically significant difference between them (P=0.642), and the averages were very close (225 and 221 days). This fact made us believe that palate plastic surgery does not have a direct action on the mechanism of opening of the Eustachian tube during the first year of follow-up of these patients. As a result, there were averages of permanence similar for the two groups. In patients with post-foramen cleft (FPF), presence or not of palate plastic surgery seemed to be an important factor in the middle ear, because the mean time of permanence of the ventilation tube in the tympanic membrane of these patients varied a lot. Patients with palate plastic surgery presented a shorter permanence time (242 days, in average), compared to those without palate plastic surgery (317 days, in average). There is then a problem: how could we explain the difference in average of permanence of ventilation tube in this group (FPF) and no difference in the group of unilateral transforamen cleft and palate plastic surgery? Next, we observed the average permanence of ventilation tube in patients with bilateral transforamen cleft, who had a higher average for the group without palate plastic surgery (289 days), as opposed to 203 days for the group with palate plastic surgery. One hypothesis would be that after palate plastic surgery stasis of secretion at the level of rhinopharynx would be more abundant (comparing to the pre-surgical period), altering the local physiology. Patients submitted to palate plastic surgery had a shorter period of permanence of the ventilation tube than in non-operated patients: 226 days as opposed to 232 days for patients with unilateral transforamen cleft, 242 as opposed to 317 days for patients with bilateral transforamen cleft, and 203 as opposed to 289 days for patients with post-foramen cleft. This fact was not detected in the literature. The probable reason for this difference between groups of patients submitted or not to palate plastic surgery should be related to local inflammatory process (topography of rhinopharynx and oropharynx), due to surgical manipulation of palate, in which veli palatini tensor and elevator muscles are inserted; it also has the other insertion of the cartilage of the Eustachian tube, which possibly facilitates the mechanism of active opening of the tube after the palate plastic surgery. Therefore, we believe that some factors may be concomitantly influencing the middle ear.
Ventilation tubes enable drainage of effusion contained in the middle ear (factor that reduces chronic inflammatory process in the middle ear). According to Dhillon (1988), patients that only correct palate cleft remain with SOM, and according to Frable et al. (1985), patients with corrected. cleft palate only improve SOM after placement of
ventilation tubes.
Palate plastic surgery may work as a facilitating factor for the mechanism of active opening of the Eustachian tube, also altering local physiology because it inserts the palate muscles closer to the normal anatomical position, and it is a factor that enlarges the tube lumen during the mechanism of active opening and making the auditory tube less collapsible. According to Doyle et al. (1980), children with cleft palate are less capable of opening the Eustachian tube because of the inability of the veli palatini tensor muscle. To Bluestone et al. (1975), patients with corrected cleft palate balance better positive pressure directed to the middle ear. Both procedures, due to local manipulation, may acutely increase local inflammatory process, in addition to causing infection.
Therefore, these two procedures result in three factors (two that facilitate reduction of chronic inflammatory process and one that stimulates acute inflammatory process) that when associated to local and general anatomical and functions abnormalities of patients lead to reduction of local inflammatory process and alter the permanence of the ventilation tube. According to Takahashi et al. (1994), patients with cleft palate have a more collapsible Eustachian tube. Palate plastic surgery seems to act exactly on this aspect and after surgery they have the possibility of opening the auditory tube by the action of the veli palatini tensor muscle. To Falk et al. (1984), tubarian dysfunction in patients with cleft palate is the result of failure in mechanism of middle ear emptying, nasal inspiration and secondary failure at the opening of Eustachian tube, plus inability to balance negative pressure during nasal inspiration.
As to average permanence of ventilation tubes in patients with unilateral and bilateral transforamen cleft compared to post-foramen cleft patients, both groups without palate plastic surgery, it was observed that permanence was considerably lower in the group with transforamen cleft (245 days, in average), than in the group with post-foramen cleft (317 days, in average), possibly because they had less nasal secretion stasis. According to Hutton et al. (1993), mucin presents in rhinopharynx secretion of patients with cleft palate has a higher amount of glycopeptides and becomes hydrodynamically heavier than in children with normal anatomy; that would be a way of proving, that secretion stasis in patients with cleft palate is one of the causes of the long lasting inflammatory processes.
The same groups of cleft palate were divided according to patients submitted to palate plastic surgery, but permanence was shorter for transforamen cleft (221 days in average) than in patients with post-foramen cleft (242 days). In both groups with and without palate plastic surgery, the presence of surgical procedure in the palate resulted in shorter period of permanence of the ventilation tube in the tympanic membrane.
Patients with unilateral transforamen cleft had longer permanence of ventilation tube (226 days, in average) than those with bilateral transforamen cleft (203 days, in average), both submitted to palate plastic surgery. In patients that had not undergone surgery, permanence is longer among those with bilateral transforamen cleft (289 days, in average) than in patients with unilateral transforamen cleft (232 days, in average). How could we explain this difference? Probably, patients with bilateral. transforamen cleft without palate plastic surgery present a chronic local inflammatory process smaller than patients with unilateral transforamen cleft, because FTB patients do not have stasis of secretion in the nasal fossae and rhinopharynx, because of the large opening that communicates both nasal fossae with oral and oropharyngeal cavity, whereas patients with unilateral transforamen cleft one of the nasal fossa has this factor of stasis, which invariably leads to chronic inflammatory process. This relation is inverted after palate plastic surgery, because in patients with unilateral transforamen cleft one of the nasal fossa is chronically adapted to the situation of not communicating with oral and oropharyngeal cavities, whereas in the patients with FTB both nasal fossae will go through the mechanism of adaptation after palate plastic surgery. The permanence of 203 days in average for FTB (C), against 226 days in average for FTU (C), may be explained by the chronic pattern of the local mucosa without stasis, and the less severe inflammatory process of FTB reduces the permanence of the tubes.
Although the groups were different, we may come to a total average for each group FTU, FTB and FPF and presence or not of palate plastic surgery and we came with a global average for patients with cleft palate submitted to palate plastic surgery (223 days) and those not submitted to the surgery (279 days). According to Weigel et al. (1989), Armstrong ventilation tubes remain less than one year in the tympanic membrane of patients without cleft palate. The mean of these averages (251 days or approximately 8 months) represents a global clinical notion of the permanence of ventilation tubes in patients with cleft palate.
The study of 82 patients with post-foramen and transforamen cleft palate enabled us, from a clinical point of view, to observe that the permanence of ventilation tubes in patients with cleft palate and correction of palate was 223 days, in the group without correction it was 270 days, and in general, the ventilation tube remained for 251 days in average and allowed us to conclude that:
1. the permanence of tympanic ventilation tubes is longer in patients that have not been submitted to palate plastic surgery;
2. comparing the average permanence of tubes and side of cleft palate (if unilateral transforamen cleft), we did not observe differences between homolateral or contralateral side to the cleft;
3. analyzing FTB and FTU and presence of palate plastic surgery, permanence was longer in the FTB group;
4. when comparing transforamen and post-foramen cleft palate in the groups with and without palate plastic surgery, permanence of ventilation tube was longer in the post-foramen cleft palate.
REFERENCE
BECKER, W.; NAUMANN, H. H.; PFALTZ, C. R. - Congenital Anomalies of the mouth and pharynx. In: BECKER, W.; NAUMANN, H. H.; PFALTZ, C. R. Ear, nose, and throat diseases. 2.ed. Nova Iorque, Thieme Medical publishers, 1994. p.374-376.
BERLIN, A. J. - Classification of clef lip and palate. In GRABB, W. C.; RESENSTEIN, S. W.; BZOCH, K. R. - Cleft Lip and palate. Surgical, clinical and speech aspect, Boston, Little Brown and cols., 1971.
BLUESTONE, C: D.; BEERY, Q. C.; CANTEKIN, E. L.; PARADISE, J. L.- Eustachian tube ventilatory in relation to cleft palate. Ann Otol Rhinol laryngol; 84 (3Pt1): 333-8, 1975 .
CASSELBRANT, M. L.; DOYLE, W. J.; CANTEKIN, E. L.; INGRAHAM, A. S.- Eustachian tube function in the rhesus monkey model of cleft palate. Cleft palate J., 22 (3): 185-91, 1985.
DHILLON, R.S. - The middle ear in cleft palate children pre and post palate closure. J, R. Soc. Med., 81(12): 710- 3, 1988.
DOYLE, W. J.; CANTEKIM, E. L.; BLUESTONE, C. D. - Eustachian tube function in cleft Children - Ann. Otol. Rhinol. Laryngol. Suppl., 89 (3 Pt 2): 34 - 40, 1980.
FALK, B.; MAGNUSON, B. - Eustachian tube closing failure. Occurrence in patients with cleft palate and middle car disease. - Arch. Otolaryngol., 110(1): 10-4, 1984.
FRABLE, M. A; BRANDOM, G. T.; THEOGARAJ, S. D.- Velar closure and ear tubings as a primary procedure in the repair of cleft palates- Laryngoscope, 95 (9Pt 1): 1044-6; 1985.
HUTTON, D. A.; FOGG, F. J.; MARTY, G.; BIRCHALL, J. P.; PEARSON, J. P.- Preliminary characterization of mucin from effusions of Cleft palate patients. - Otolaryngol Head Neck Surg., 109 (6): 1000-6, 1993.
LOPES FILHO, O.- Otite Media Serosa Crônica. In: Otacílio & Campos - Tratado de Otorrinolaringologia. São Paulo, Roca, 1994. P. 677-694.
MODOLIN, M.- Fissuras Labiopalatinas. In: MODOLIN, M.; NETTO, A. C.; RAIA, A. A.; ZERBINE, E. J. - Clínica cirúrgica Alípio Correa Netto -1° volume- 4° edição - São Paulo, Sarvier, 1988. p.260-321.
OBERASCHER, G. & ALBEGGER, K.- Muco-serous otitis media- Wien Med Wochenschr, 172 (11- 12): 248- 53, 1992.
PARADISE, J. L.; Management of middle ear effusions in infants with cleft palate - Ann. Otol. rhinol. laryngol., 85 (2 Suppl 25 Pt 2): 285 - 8, 1976.
QUANTE, M.; ESSER, G.; STRAUSS, P. - Therapeutic results in the treatment of otitis media in children with and without cleft palate - Laryngol. Rhind. otol. (Strug), 55 (11).: 879 -82, 1976.
TAKAHASHI, H.; HONJO, J.; FUJITA, A.- Eustachian tube compliance in cleft palate- a preliminary study- Laryngoscope, 104 (1Pt1): 83-6; 1994.
WEIGEL, M. T.; PARKER, M. Y.; GOLDSMITH, M. M.; POSTMA, D. S.; PILLSBURRY, H. C.- A prospective randomized study of four commonly used tympanostomy tubes - Laryngoscope, 99 (3): 252- 6, 1989.
* Master degree at the Discipline of Otorhinolaryngology, Universidade Federal de SÃo Paulo (UNIEESP)-Escola Paulista de Medicina (EPM).
** Ph.D. Professor at UNFESP-EPM.
*** Ph.D. Professor of the Discipline of Otorhinolaryngology at UNIFESP-EPM.
**** Full Professor and Head of the Discipline of Otorhinolaryngology at UNIFESP-EPM.
Study presented at 35° Congresso Brasileiro de Otorrinolaringologia, which received a special citation. Study conducted at the Discipline,of Otorhinolaringology of the Department of Otorhinolaryngology and Human Communication Disorders at Universidade Federal de São Paulo - Escola Paulista de Medicina.
Address for correspondence: Douglas S. R. Morales - Disciplina de Ororrinolaringologia - UNIFESP-EPM - Rua Botucatu, 740- Vila Clementino
04023-900 São Paulo /SP - Tel: (55 11) 5549-7041.
Article submitted on August 15, 2000. Article accepted on October 20, 2000.