Year: 2000 Vol. 66 Ed. 6 - (8º)
Artigos Originais
Pages: 627 to 630
Prophylactic Antibiotic Therapy After Tonsillectomy. Study with Amoxilin-Clavulanic Acid.
Author(s):
Cecil C. Ramos*,
Maria E. R.Gonçalves**,
Priscila Bogar Rapoport***,
Elie Fiss****.
Keywords: tonsillectomy, post-operative, antibiotic
Abstract:
Backgrounds and aims: The authors carry through prospective study in children submitted to tonsillectomy, with and without antibiotic (Amoxicillin-Clav.) post-surgery, aiming to determine which is the best altitude in this situation. Patients and methods: Tonsillectomy was carried out in 58 children by Sluder technique, in fortuitous forte, with ser and age equivalence. The aim of this study was to compare subjective parameter (pain, edema, hyperemia, secretion) , laboratorial (hemogram and coagulogram.), and culture in infection suspect cases. Results: There was not difference in the subjective parameters, even so in the laboratorial analyze was observed increment in the white series from children without antibiotic. There was not meaningful difference between the two groups about infection or infection suspect in the post-surgery. Conclusion: These findings suggest that, in children, there isn't a real indication of Amoxicillin-Clavulanic acid in post-surgery tonsyllectomy.
![]()
INTRODUCTION
There are innumerous contradictions between what is taught in theory at Medical school and the practice we face in a daily basis in our offices or surgical rooms. The indication of use of prophylactic antibiotics in contaminated surgeries is classical, but there is controversy as to its administration in surgeries potentially considered contaminated or non-contaminated. However, in our daily medical practice and observing the procedure of our colleagues, in loco or through the literature, we clearly see the preference in using prophylactic postoperative antibiotics in a great deal of surgeries, and there does not seem to be any standardization of procedure1, 2, 3, 4, 5, 6.
Classically, we define the use or not of prophylactic antibiotics based on the type of surgical wound. Howard et al., in 19645, classified surgical wounds in clean, clean contaminated, contaminated and dirty. Therefore, a clean wound would be voluntarily made during the surgical act, in a area where there is room for ideal asepsis and under appropriate surgical conditions. Clean contaminated wound is this kind of surgical wound in potentially contaminated sites, such as oropharynx, urinary tract, respiratory system, without signs of inflammation or infection. Contaminated wounds are those involving an infected area; and dirty ones are caused by non-surgical trauma, involving clinical infection or visceral perforation. Therefore, based on the classification of surgical wound, we could define the best way to use or not antibiotic prophylaxis9. Authors such as W. R. Sandusky et al., in 198010, did not recommend the use of prophylactic antibiotics in clean surgeries; we should bear in mind that 75% of all surgeries fall within this category. According to their statistics, 17% of the surgeries would be classified as clean contaminated, and in their opinion, the use of prophylactic antibiotics would be indicated in this category only in surgeries in which there was a direct communication between a potentially contaminated area and the area initially free of pathological agents, such as neck dissection together with approach of oropharyngeal cavity. However, the authors did not believe that prophylactic antibiotics were necessary in clean contaminated surgeries, but rather that they should be limited to the area of the surgical wound, such as septoplasty or tonsillectomy, in which the degree of contamination would not justify the use of antimicrobial agents. Authors such J. C. Tabet et al., in 19908, 11, and S. A. Telian et al., in 198612, in turn, advocated the use of postoperative antibiotics in clean contaminated surgeries.
Taking into account the lack of uniformity of prophylaxis intervention in tonsillectomy, a surgery considered clean contaminated, we aimed at collecting data that would help us standardize prophylactic intervention in this kind of surgery, in order to protect patients from possible postoperative infections, and also to avoid administration of unnecessary medication that could lead to side effects and development of bacter resistance.
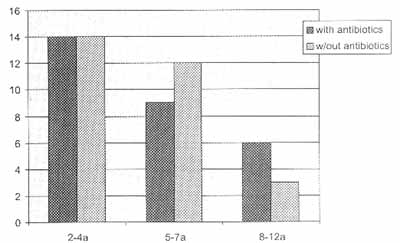
Figure 1. Distribution of patients according to age and group.
MATERIAL AND METHODS
We conducted a prospective study with 58 children submitted to tonsillectomy by Sluder's technique, both sex, at randomly divided into 2 groups: 29 patients received Amoxicillin-Clavulanate intra and post-operatively, at doses according child's weight, for 7 days; the second group consisted children who did not receive antibiotic therapy (Figure 1). TI choice of antibiotic was made based on the pathogens most found in the bacterial flora of oropharynx and their sensitive to drugs8, 9. Mothers were instructed to give paracetamol P according to child's weight, in case of fever or pain. Children were anesthetized and operated with the same technique and by the same surgeon. Postoperative follow-up was conducted blindly by another physician of the Service, in which data such as severity of pain, fever, local hyperemia, local edema an presence of secretion were measured through a linear analog test adjusted to our needs, both by the patient and the examiner. We asked children to score the symptoms from 0 to 3, and zero was absence of symptom, 1 was mild, 2 was moderate and 3 was intense severity. The same analysis was conducted with the signs scored by the physician. Children were assessed preoperatively, and 3rd, 7th and 14th days after surgery, through history, physical exam and Complete Blood Count (CBC) and coagulogram in the pre and 3`d postoperative days, repeated if there was suspicion of infection, together with secretion culture and antibiogram. The results were analyze by qui-square test, with significance of p<0.5. The study was conducted in a private hospital of the city of Santo Andre, ii middle class patients, with previous authorization of parents.
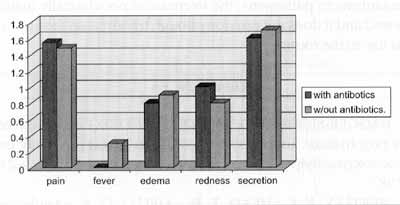
Figure 2. Mean score of subjective variables in the different) groups analyzed.
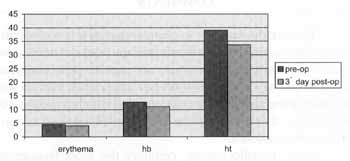
Figure 3. Mean variation of quantitative parameters of red cell series pre and 3rd post-op day.
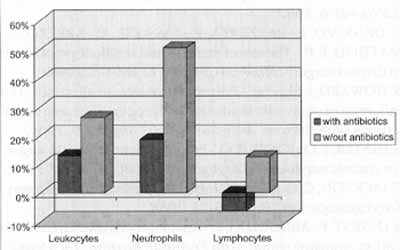
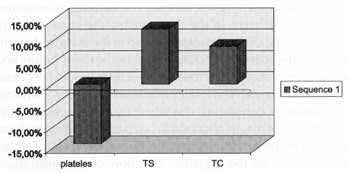
Figure 4. Variation of percentage means of the main elements of white cell series between pre and 3'd post-by day in the different studied groups.
Figure 5. Variation of percentage means of the main elements of coagulogram between pre and 3'd post-op day.
RESULTS
Postoperative assessment of subjective parameters (pain, edema, hyperemia and secretion) did not produce significant difference between the two groups (Figure 2). In the group treated with postoperative antibiotics we observed 5 children with suspicion of infection (17.24%) in the analysis conducted in the 3rd day (fever of 38° C or more and/or 11,000 or more leukocytes), with positive result for Staphylococcus aureus in one case, and negative in the others. In the group without prophylactic antibiotic therapy, 4 children (13.79%) presented suspicion of postoperative infection, but all cultures were negative. On the 7th post-op day, no children of both groups presented any sign or symptom indicating infection. Antibiotic supplementation was not necessary in any case.
In the lab exam, red cell series of CBC presented a significant reduction of quantitative parameters in the Yd post op day when compared to preoperative exams, with a mean difference of -11.15% in the number of erythrocytes, -12.59% in hemoglobin levels, and -13.36% in hematocrit level (Figure 3). The remaining parameters of the red series did not show significant differences. In the white cell series, results showed a general mean increase of elements in the comparative analysis between pre and 3`d post-op day (15.55%), significantly higher in the group that did not receive antibiotic prophylaxis (26.27%). In this analysis, neutrophils were the cells that suffered the largest increment, a mean increase of 50.35% in the 3rd post-op day of children without antibiotic therapy compared to pre-op exam (Figure 4). In the evaluation of coagulograms, in the global analysis we observed a mean reduction of 13.82% of platelets when comparing pre-op and 3nd a post-op day, followed by a mean increase of 12.82% in bleeding time and 8.81% in coagulation time, but the differences between the two groups were not statistically significant (Figure 5).
COMMENTS
Despite the fact that in clean surgeries it is well established that prophylactic antibiotic therapy does not need to be used, 1°, the same consensus does not exist for clean contaminated surgeries - both based on our experience and on the literature, there are different positions as to whether prophylactic antibiotic therapy should be used, as well type and administration of antibiotics.
As to tonsillectomies, certainly the most frequently performed clean contaminated surgery all over the world, authors such as J. C. Tabet et al. in 1990, considered mandatory the use of prophylactic antibiotic therapy, as well as S. A. Telian et al. in 1986, who showed in their study a significant difference in incidence of surgical infections in the group of patients who did not receive prophylactic antibiotic therapy, compared to a group of patients with antimicrobial medication. In our analysis, although hematological response was clearly different in the two groups, the same was not -observed in the clinical assessment and in the definite demonstration of the active infectious process, by means of culture and antibiogram of secretion of tonsillar sites; thus, we did not obtain a conclusion favorable to routine administration of prophylactic medication in conditions described by the present study. Discrepancy of results obtained in our data compared to those obtained by other authors may be due to diversity of drugs used, as well as the variables duration of administration, frequency and concentration of drug. Other factors, such as age, social and economic background, and nosocomial characteristics may modify considerably the results, and they did not enable generalizations on a standardized intervention.
CONCLUSIONS
In our study, we observed a clear difference in some lab parameters between the two groups, especially in the white cells of CBC, in which leukocytes and neutrophils had a larger increment in the group that did not receive postoperative antibiotic therapy. However, similar controversy was not observed in clinical parameters, and we did not find statistically significant differences between the two groups as to severity of symptoms, signs or frequency of post-op infections, suggesting that although prophylactic antibiotic therapy with Amoxicillin Clavulanate in tonsillectomies reduces the exposure of the organisms to pathogens, the decrease is not clinically man fested and it does not provide enough information to suppol its use in the routine.
REFERENCES
1. BAGGER-SJOBACK, D.; MENDEL, L.; NORD, C. E. -The role of prophylactic antibiotics in middle ear surgery. A study or phenoxymethyl penicillin prophylaxis. Am J Otol; 8(6):519-23 1987.
2. BERTLEY, K. C.; HEAD, T. W.; AIELLO, G. A. - Antibioti prophylaxis in orthognathic surgery: a 1-day versus 5-day regimen. J Oral Maxillo fac Surg; 57(3):226-30 1999.
3. CARLIN, W. V.; LESSER, T. H.; JOHN, D. G.; FIELDER, C CARRICK, D. G.; THOMAS, P. L.; HILL, S. - Systemic antibiotic prophylaxis and reconstructive ear surgery. Clin Otolaryngol 12(6): 441-6, 1987.
4. DE SALVO, L.; RAZZETTA, F.; TASSONE, U.; AREZZO, A. MATTIOLI, F. P. -The role of drainage and antibiotic prophylaxis in thyroid surgery. Minerva Chir; 53(11): 895-8, 1998.
5. HOWARD, J. M., et al. -Postoperative wound infections: The influence, of ultraviolet irradiation of the operating room and d various other factors. Ann. Surg., 160 (Suppl.): 9, 1964.
6. HESTER, T. O.; JONES, R. O. - Prophylactic antibiotics in surgery for chronic ear disease. Laryngoscope; 108(9):1334-7, 1998
7. JACKSON, C. G. - Antimicrobial prophylaxis in ear surgery Laryngoscope; 98(10): 1116-23, 1988.
8. LEGENT, F.; ARNOULD. J. F. -Antibioprophylaxie en chirurgie ORL et stomatologique. Ann FrAnesth Reanim; 13(5 Suppl) S100-9, 1994.
9. MENSA, J.; GATELL, J. M.; ANTA, M.T. J.; PRATS, G. - Guia de Terapeutica Antimicrobiana. Editora Masson. Oitava edição: 367-371.1998.
10. SANDUSKY, W. R. - Use of Prophylactic Antibiotics in Surgical Patients. The Surgical Clinics of North America, February.-8392, 1980.
11. TABET, J. C.; JOHNSON, J. T. - Wound infection in head and neck surgery: prophylaxis, etiology and management. J Otolaryngol; 19(3): 197-200, 1990.
12. TELIAN, S. A.; HANDLER, S. D.; FLEISHER, G. R.; BARANAK, C. C.; WETMORE, R. F:; POTSIC, W. P. - The effect of antibiotic therapy on recovery after tonsillectomy in children. A controlled study. Arch Otolaryngol Head Neck Surg; 112(6):610-5, 1986.
* Physician, graduated from FM Botucatu - UNESP - Otorhinolaryngologist graduated from Faculdade de Medicina da USP, Doctorate studies under course at FMUSP.
** Nurse, Master degree under course at Faculdade Medicina da Fundaqao ABC.
*** Ph.D., Professor of Otorhinolaryngology at FMUSP.
**** Joint Professor of the Discipline of Pneumology at Faculdade de Medicina da Fundação ABC.
Study conducted at Hospital a Maternidade Cristóvão da Gama - Santo Andre/ SP.
Approved by the Committee of Ethics of Faculdade de Medicina da Fundação ABC.
Address for correspondence: Cecil Cordeiro Ramos - Rua Gamboa, 245 - 09190-670 Santo André/ SP - Tel: (55 11) 4994-8970 - E-mail: cecill@zaz.com.br
Article submitted on August 4, 2000. Article accepted on September 28, 2000.