Year: 2000 Vol. 66 Ed. 6 - (6º)
Artigos Originais
Pages: 614 to 618
Headache by Nasal Mucosal Contact: Surgical Results in 21 Patients.
Author(s):
Christian Wiikmann*,
Marcus M. Lessa*,
Patrícia P. Santoro**,
Rui Imamura***,
Richard L. Voegels****,
Ossamu Butugan*****.
Keywords: Rhinogenic headaches, nasal septum, concha bullosa, treatment
Abstract:
Introduction: Headache and facial pain are symptoms with which otolaryngologists must deal frequently. Several anatomic variations of the nose and sinuses can originate chronic headache, even in the absence of inflamatory or tumoral affections. These variations may cause contact points between opposite nasal mucosas which, in turn, may cause pain. Aim: The aim of this study is to analise patients with contact point headaches, corelating anatomic variations and outcomes after surgical treatment. Material and methods: From january of 1996 to june of 1999, medical data of twenty one patients with contact point headache resistant to medical therapy were retrospectively studied. Results: A septal deviation and/or spur was found in 80,95% of the patients, concha bullosa in 14,28% and hipertrophic inferior % turbinate in 4,76%. All patients were surgically treated and 80,95% showed improvement of pain. This improvement was related to concomitant improvement of nasal obstruction. Conclusion: The authors concluded that surgery must be considered in the management of contact point headaches resistant to clinical treatment.
![]()
INTRODUCTION
Otorhinolaryngologists frequently manage symptoms of headaches and facial pains. Many sinonasal affections manifest headaches and facial pain associated with other symptoms, such as nasal obstruction, rhinorrhea, and nasal pruritis, among others. Therefore, patients with inflammatory or tumor affections are frequently present with headache, whose cause is predominantly identifiable2, 13. Nevertheless, some sinonasal alterations with more difficult diagnoses may present headache as the predominant or sole symptom, which is in many occasions mistaken by primary headaches3. As examples of these disorders, described as causes of chronic headache, we may include septal deviations and spurs, pneumatized turbinates, paradoxical middle turbinate, and anatomical variations of unciform process, among others13. The purpose of the present study was to evaluate patients with sinonasal disorders in which headache was a predominant symptom and correlate anatomical variations with clinical picture and post-operative progression.
MATERIAL AND METHOD
We conducted a retrospective study by analyzing the medical files of 21 patients treated at the Division of Clinical Otorhinolaryngology at HCFMUSP, in the period between January 1996 and July 1999, submitted to surgical treatment for nasal affections, in which headache was the main complaint. Patients with signs and symptoms of rhinitis associated with headache were clinically treated with topic corticoids, antihistaminic, and nasal lavage. Only those that did not show improvement of headache were submitted to surgery. We excluded from the sample subjects who had chronic or acute sinusitis, nasal polyposis and nasal tumors.
Symptoms (headache and nasal obstruction) were evaluated according to a system of scores varying from 1 to 10, in which 1 represented absence of symptom and 10 referred to the most severe symptom. Quantification of symptoms was conducted during medical interviews in the pre-op and immediate post-operative situation. As the criterion indicative of improvement after surgical treatment, we considered a reduction of 50% or more in the score first attributed to the symptom.
We also analyzed the following data: age, sex, presence of associated rhinitis symptoms and performed surgical management.
RESULTS
In our study, ages ranged from 12 to 54 years, mean age of 31.57 years. Eleven patients (52.38%) were male and 10 were female subjects, (13.61%)- amounting a male/ female ratio of 1.1:1.
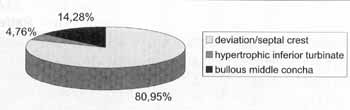
Figure 1. Anatomical variations.
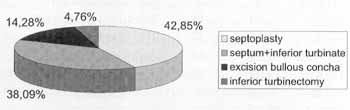
Figure 2. Performed surgeries.
Out of 21 studied patients, 13 (61.9%) had signs and symptoms of rhinitis, and all of them had already been treated with topic corticoid, antihistaminic and nasal lavage.
Among detected anatomical variations, septum deviation and/or spur was found in 17 patients (80.95%); pneumatized middle concha in 3 patients (14.28%); and hypertrophy of inferior concha in 1 patient (4.76%), as shown in Figure 1.
As to performed surgical procedure, 9 patients (42.85%) were submitted exclusively to septoplasty; 8 (38.09%), to septoplasty associated with partial inferior turbinectomy; one patient (4.76%) underwent only partial inferior turbinectomy; and 3 (14.28%) underwent endoscopic partial exeresis of bullous middle concha, as shown in Figure 2.
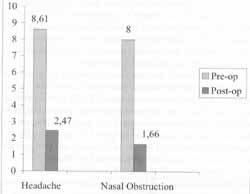
We observed that the score attributed to severity of headache before the surgical procedure varied from 5 to 10, mean of 8.61 and standard deviation of 1.53. In the first postop month, the score attributed to severity of headache had a mean of 2.47, standard deviation of 2.61. As to nasal obstruction, the score before surgery varied from 4 to 10, mean of 8 and standard deviation oA1.92, but in the first post-op month the mean was 1.66, standard deviation of 1.35 (Figure 3).
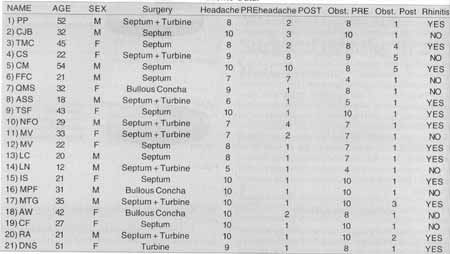
Out of the total number of studied patients (n=21), 17 (80.95%) progressed and improved headache after the surgical procedure; and 4 (19.04%) did not improve or show partial improvement of headache. Out of the patients who had improvement, they all had concomitant improvement of nasal obstruction. Out of the patients who did not experience total improvement of headache or who had only partial relief, 3(75%) had signs and symptoms of rhinitis; and 2 (50%) had only, partial improvement of nasal obstruction. Al patients submitted to partial exeresis (meatal face) of bullous middle concha progressed and improved headache in the post-op follow-up.TABLE 1- Patients' Data.
Key: Septum = Septoplasty; Turbine = bilateral inferior partial turbinectomy; Bullous Concha = exeresis of meatal face of bullous middle concha.
Figure 3. Progression of symptoms.
DISCUSSION
Pain is the symptom that most frequently motivates patients to seek for medical assistance. Craniofacial segment is one of the body segments in which pain is more frequently manifested5. Headaches of sinonasal origin without inflammatory or tumor evident cause has been object of study of various articles, despite the fact that its pathophysiological bases had been launched since 1943, when McAuliffe et al. 9 showed that nociceptive stimuli, among them mechanical pressure, applied to determined points of nasal mucosa produced pain. Headaches because of contact points of opposed nasal mucosas has been correlated to contact between septal deviation or spur and conchae, especially the middle conchae6, 7, 11, 12. Stammberger and Wolf, in 198813, published a review article in which they described anatomical variations of the lateral wall of nasal cavity that predisposes to contact point with opposed mucosa, leading to headache. As an example of these alterations, there are variations of uncinated process (anteriorly, medially or laterally curved, pneumatized), variations of middle concha (bullous concha, paradoxical curve), variations of ethmoidal bulla (exception-ally large size), variations of agger nasi (pneumatized). Clerico, in 19964, published an article reporting 3 cases of chronic) headache related to concha pneumatization.
Image 1. Computed Tomography of paranasal sinuses at coronal section, demonstrating the bullous concha in the right nasal fossa.
The pathophysiological mechanism mostly used to explain headache caused by mucosa contact points was proposed by Stammberger and Wolf in 198813: 1) the contact between opposed mucosas (mechanical pressure) would be a stimulus to nociceptors located on the nasal mucosa; 2) the activation of these nociceptors would trigger action potentials in demyelinated type C nervous fibers that innervate the nasal mucosa, whose main neurotransmitters would be neuropeptides, especially substance P; 3) these action potentials would be propagated by two paths, mainly the central and the peripheral paths; 4) central path would be that in which the nervous peptidergic fibers make synapses in the ganglia and trigeminal nuclei and reach the sensorial cerebral cortex, signaling the pain; 5) peripheral path would be that in which nervous peptidergic fibers are in contact with vessels, glands and smooth muscle fibers, releasing substance P in the tissues and causing vasodilatation, increase of vascular permeability and glandular hyper-secretion.
In our study with patients who had headache because of contact points of nasal mucosas, we observed that the most frequent anatomical variation related to the symptom was septal deviation and/or spur, amounting to 80.95% of the studied cases. This finding is compatible with the results of studies published in the literature, such as the study by Chow2, in 1994, that evaluated the causes of rhinogenic headache and found a frequency of 66.67% of septal deviations and/or spurs in studied patients. The second most frequently found variation in our patients was pneumatized middle turbinate (bullous concha), corresponding to 14.28% of the cases.
The improvement of headache after surgical treatment was obtained in 80.95% of the patients. In the articles reviewed by the authors, the relief of the symptom headache in surgically treated patients ranged from 63.6% to 100%1, 2, 3, 8, 10. It is important to point out that quantification of a subjective symptom as headache is very imprecise, since it follows subjective criteria of evaluation and depends on social and cultural characteristics of studied patients. The comparison of results among the various studies is also imprecise, since there is no standardization of criteria used to quantify headache.
According to Low8, in an article published in 1995, surgically treated patients for rhinogenic headache would have a higher likelihood of improving headache if they presented relief of associated nasal obstruction. In his study, out of the patients who had headache improvement, only 5.71% did not experience improvement of nasal obstruction. This result corresponded to what was observed in our study, in which all patients who had headache improvement, also presented improvement of nasal obstruction, whereas 50% of the patients who did not experience headache improvement did not have relief of nasal obstruction.
CONCLUSION
Headache related to contact points of nasal mucosas may be considered as an exclusion diagnosis, but it should be included in differential diagnosis and appropriately investigated, so that management is in fact effective. In our study, we concluded that septal deviations and/or spurs are the main alterations involved in the genesis of headache because of contact points, and that improvement of headache after surgical treatment is directly related to concomitant improvement in nasal obstruction.
REFERENCES
1. BRENT, A. SR.; KENNEDY, D. W.; TANABODEE, J. et al. Long-term results of functional endoscopic sinus surgery. Laryngoscope, 1998; 108: 151-157.
2. CHOW, J. M. - Rhinologic headaches. Otolaryngol. Head Neck Surg., 1994; 111: 211-218.
3. CLERICO, D. M. - Sinus headaches reconsidered: referred cephalgia of rhinologic origin masquerading as refractory primary headaches. Headache, 1995; 35: 185-192.
4. CLERICO, D. M. - Pneumatized superior turbinate as a cause of referred migraine headache. Laryngoscope, 1996; 106: 874879.
5. FINKEL, A. G.; MANN, J. D.; LUNDEEN, T. F.-Headache and facial pain. In: Bailey JB, ed. Head and Neck Surgery Otolaryngology, 2nd ed. 1998: 287-304.
6. GERBE, R. W.; FRY, T. L.; FISCHER, N. D.-Headache of nasal spur origin: an easily diagnosed and surgically correctable cause of facial pain. Headache, 1984; 24: 329-330.
7. GOLDSMITH, A. J.; ZAHTZ, G. D.; STEGNAJAJIC, A. et al. Middle turbinate headache syndrome. Am. J. Rhinol.1993; 7: 17-23.
8. LOW, W. K.; WILLATT, D. J. - Headaches associated with nasal obstruction due to deviated nasal septum. Headache 1995; 35: 404-406.
9. McAULIFFE, G. W.; GOODELL, H.; WOLFF, H. G. - Experimental studies on headache: pain reference from the nasal and paranasal structures. Am. Res. Nerve. And Ment Dis. Proc 1943; 23: 185-192.
10. PARSONS, D. S.; BATRA, P. S. - Functional endoscopic sine surgical outcomes for contact point headaches. Laryngoscop 1998; 108: 696-702.
11. RYAN, S. E. SR., RYAN, R. E. Jr. - Headache of nasal origin Headache, 1979; 19: 173-179.
12. SCHONSTED-MADSEN, U.; STOKSTED, P.; CHRISTENSE~ P. H.; KOCH-HENRIKSEN, N. - Chronic headache related to nasal obstruction. J. Laryngol. Otol., 1986; 100: 165-170.
13. STAMMBERGER, H.; WOLF, G. - Headaches and sine disease: the endoscopic approach. Ann. Otol. Rhinol. Laryngo 1988; 97 (suppl 134): 3-23.
* Resident Physician of the Division of Clinical Otorhinolaryngology of Hospital das Clinicas Faculdade de Medicina da Universidade de São Paulo (FMUSP).
** Physician, Post-Graduate studies under course at Division of Clinical Otorhinolaryngology of Hospital das Clínicas, FMUSP.
*** Assistant Physician of the Division of Clinical otorhinolaryngology of Hospital das Clinicas, FMUSP.
**** Assistant Physician, Ph.D., Division of Clinical Otorhinolaryngology of Hospital das Clinicas, FMUSP.
***** Associate Professor of the Discipline of Otorhinolaryngology at FMUSP.
Study conducted at the Division of Clinical Otorhinolaryngology of Hospital das Clinicas at FMUSP.
Address for correspondence: Christian Wiikmann - Divisao de Clinica Otorrinolaringol6gica - Hospital das Clinicas - FMUSP -Avenida Dr. Eneas de Carvalho Aguiar, 255 6° Andar - Sala 6021 - Sao Paulo /SP - Fax: (55 11) 280-0299.
Article submitted on July 27, 2000. Article accepted on September 14, 2000.