Year: 2000 Vol. 66 Ed. 4 - (4º)
Artigos Originais
Pages: 335 to 340
Clinical Analysis and Descritive Epidemiologyc of the Squamous Cell Carcinoma of the Maxilla Sinus.
Author(s):
José C. L. Geraldes Filho*,
Josias A. Sobrinho**.
Keywords: squamous cell carcinoma, neoplasm of maxillary sinus-epydemiology, paranasal sinus
Abstract:
Introduction: From among malign neoplasms in paranasal sinus, the squamous cell carcinoma is the more frequent histological kind of carcinoma, and the maxillary sinus is the more affected anatômical structure. The symptoms are insidious and confused with chronic inflammatory process, leading to a delay of diagnosis and an increase in advanced cases in first attendance. Purpose: To evaluate the patients' clinical caracteristics, the factors that delay the diagnosis and to propose measures for and earlier diagnosis. Material and method: The authors present a retrospective study of 60 patients examined and treated in the Surgery of Head and Neck Center of the Heliópolis Hospital from 1977 to 1993 and analyze it in tables and charts. Results: In terms of their professions,16,7% were tailors and dressmakers. Chronic sinusites was observed in 10% of the patients. The most common complaints were: face swelling (36,7%), nasal obstruction (23,3%) dental weakening and/or pain (21,7%). The elapsed time of complaint varied from two to eight months (81,7%) and the period between diagnosis and treatment varied from two to four weeks (20%), and even two weeks (43,3%). As a reason for delay, 61,7% didn't took the initial symptoms into account and in 20% there was lack of dentist's orientation. Patients complaining about face swelling spent four months to see a specialist physician (37,9%) and those complaining about nasal obstruction (29%), dental weakening and/or pain (25,8%) reported more than four months. Conclusion: The incidence was wider among male and textile workers. Nasal obstruction, dental weakening and/or pain were the complaints which made the patients delay in seeing a physician. Oncology teaching to professionals of health and improvement of specialized health services will contribute to decrease the delay in treatment, leading to the best prognostic.
![]()
INTRODUCTION
A number of studies showed that paranasal sinuses carcinoma is not common (Fukuda et al., 1987); if present, maxillary sinus is the most affected of them (Kenady, 1986), whereas squamous cells carcinoma is the most frequent histological type (Larsson and Martensson, 1972). Survival rates depend on early diagnosis and radical treatment, varying in each case. Due to the anatomical location of the tumor, symptoms are intense and mistaken for inflammatory process (Tabb and Barranco, 1971), leading to delays in diagnosis and an increased rate of advanced cases at the first medical visit. Symptoms like facial pain, enlargement of hemiface, epistaxis, nasal obstruction, toothache, and rhinorrhea confuse specialists of different areas, making them start a treatment that is not specific to the underlying pathology (cancer). Studies have reported that the time between onset of symptoms and diagnosis varied from 6 to 12 months (Alvarez et al.,1995), and patients had delay in diagnosis because of other hypotheses different from cancer. Different factors are involved in etiology and most of them have not been confirmed yet, requiring our full attention. The scarcity of publications about epidemiological studies of these tumors motivated our research in order to try to evaluate possible etiological factors, suggesting measures to reduce late diagnosis and consequently, improve prognosis.
MATERIAL AND METHOD
This is a descriptive non-analytical study based on the retrospective analysis of 60 medical files of patients with diagnosis of squamous cells carcinoma of maxillary sinus, assessed and treated at the Service of Head and Neck Surgery of Complexo Hospitalar Heliópolis, between 1977 and 1993. Patients were analyzed as to age, sex, ethnic group, profession, location of tumor, medical history, use of alcohol, smoking, type of initial complaint that made the patient search medical assistance, duration of complaint (in months) and reason for delay to start treatment after onset of symptoms. The time between diagnosis and treatment was analyzed for 45 out to 60 cases owing to lack of data in the medical files.
Since half of the patients had taken less than 4 months to search for a specialist after initial symptoms, we created a variable called delay and crossed it with type of complaint.
These data were analyzed in tables and graphs. Details regarding therapeutic approach and progress of cases were not object of the present study.
RESULTS
We analyzed 60 patient with diagnosis of squamous cell carcinoma of maxillary sinus. Mean age was 60vears and male/ female ratio was 2.7:1; out of 73.3% of males, 70% were white and 30% were non-white (Table 1).
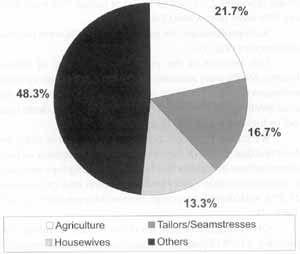
As to professions, we noticed that 16.7% were tailors or seamstresses (Fig. 1).
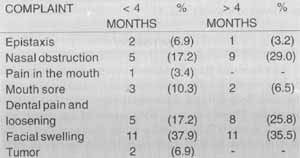
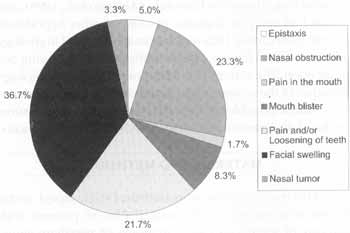
Ten percent of the patients had history of chronic sinusitis, 69.3% were smokers and 70% did not drink alcoholic beverages (Fig. 2). The most common type of complaints was facial swelling (36.7%), nasal obstruction (23.3%), dental pain and/or loosening (21.7%) (Fig. 3).
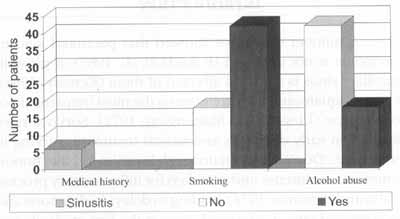
We crossed type of complaint with variable delay and observed that 37.9% of the cases had had complaint of facial edema for four months or less before searching for a specialist. In nasal obstruction (29%) and dental pain and/or loosening (25.8%), with dental extraction, time was longer than 4 months (Table 2).
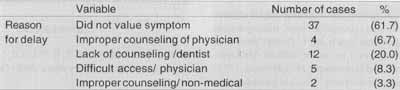
Observing the reason for delay before searching for a specialist, 61.7% of patients did not value the initial symptoms and in 20% of the cases, the dentist did counsel the patient accordingly after dental extraction (Table 3).
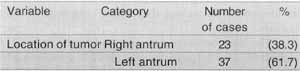
The tumor was located in the left maxillary antrum in 61.7%, and in the right antrum in 38.3% (Table 4).
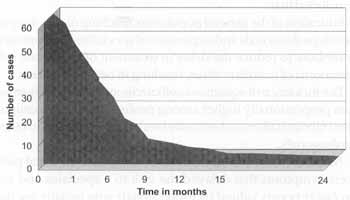
Most of the patients had a duration of complaint between 2 and 8 months (81.7%). Out of these, 10 patients (16.7%) had had it for 2 months, and 9 patients (15%) had had it for 6 months. The variation between extremes was of up to 24 months (Fig. 4).
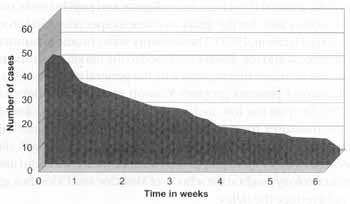
The time between diagnosis and treatment was 2 weeks for 43.3%. In 20% of the patients this time varied from 2 to 4 weeks and in 11.7% it exceeded 4 weeks and in some cases it amounted to 8 weeks (Fig. 5).
DISCUSSION
Our results showed that both patients and health professionals contribute to the delay in diagnosis, resulting in patients that come for a first visit at advanced stage, what leads to poor prognosis. There was no predominance of age range. The mean age was 60 years, similar to the data provided by the literature (Watson, 1942; Lederman, 1970; Ahmad et al., 1981; Spiro et al., 1989; Sisson et al., 1989; Alvarez et al., 1995), and predominance of male patients, a fact confirmed by different authors (Watson, 1942; Andrade Sobrinho, 1967; Lederman, 1970; Tabb and Barranco, 1971; Barbosa, 1979; Ahmad et al., 1981; Kenady, 1986; Sisson et al., 1989; Spiro et al., 1989; Fava and Carvalho,1989; Alvarez et al.,1995). We noticed predominance of white patients in our study, similar to the results of Barbosa (1979). We did not find in the literature factors relating predominance of ethic qroups. We believe that the predominance of white patients was either an accident or motivated by the exposure to a specific occupational factor.TABLE 1 - Distribution of patients according to age, sex and ethnic group.
Figure 1. Distribution of patients according to profession.
Others: administrators, retirees, bank workers, woodworkers, businesspeople, electricians, plumbers, cleaners, mechanics, general metal and steel manufacture workers, general metal manufacture workers, machine preparation operator, general services, telephone operator, manufacturer of musical instruments, carriers and ignored.
TABLE 2 - Correlation between number of patients with late diagnosis, according to type of complaint.
Figure 2. Distribution of patients according to personal history, smoking and alcohol abuse.
Figure 3. Distribution of patients according to type of complaint.
Smoking is described as one of the risk factors (Fukuda et al., 1987, Fukuda et al., 1989). We believe that this information is important if we analyze duration of smoking and type of product smoked, a fact we did not find in most of the medical files. Differently from mouth and oropharynx cancer, the abuse of alcohol does not seem to be a predisposing factor.
In 10% of our patients there was history of chronic sinusitis, similar to the data presented by Alvarez et al. (1995), despite the fact that the authors did not state the relation between sinusitis and neoplasia. Some described a strong association with chronic sinusitis (Larsson and Martensson; 1972; Barbosa, 1979; Fukuda et al., 1987; Fava and Carvalho; 1989; Shimizu et al.,1989), and if the patient does not respond to appropriate treatment, we should suspect of a malignant neoplasic process and the physician must investigate thoroughly (Sisson et al., 1963; Kagan and Steckel, 1978). Despite the low incidence in our cases, we believe that chronic inflammatory process is a predisposing factor because of metaplasia of mucosa, as confirmed by the studies of Shimizu et al. (1989) and reported by Carvalho and Andrade Sobrinho (1994).
Figure 4. Cumulative graph, showing duration of complaint (in months).
Figure 5. Cumulative graph showing the period of time between diagnosis and treatment (in weeks).
TABLE 3 - Distribution of patients according to the reason for delay to see specialist physician.
The high level of chromium in plants used for inhalation (Baumslag and Keen, 1972), workers exposed to nickel (Roush et al., 1980; Hernberg et al.,1983), polyp and papilloma (Fukuda et al., 1987), subjects exposed to wood dust and workers in furniture industry (Roush et al., 1980; Hernberg et al., 1983; Fukuda et al., 1987; Fukuda et al., 1989; Shimizu et al., 1989), manipulation of leather and shoe manufacture (Hernberg et al.; 1983) have been described as risks for the development of paranasal sinuses carcinoma. In our study, the large number of workers that manipulated fabrics made us wonder whether there was a cause-effect ratio. It would be necessary to know the population distribution of professions in Brazil in order to confirm this incidence.
Most of the patients came to our specialized clinic after a long time from the onset of symptoms to diagnosis, contributing to a high percentage of advanced cases seen in the first visit. The duration of complaints varied from 2 to 8 weeks in 81.7%, an interval observed by Alvarez et al., 1995. We noticed that patients did not know about their disease, either because they had never heard of it or due to inappropriate counseling by health professionals or laypeople. This fact has to be changed in order to increase survival rates. Careful follow-up and investigation of patients who have hypothesis of cancer would result in reduction of the time from onset of symptoms to final diagnosis (Sisson et al., 1989).TABLE 4 - Distribution of patients according to location of tumor.
In our study, 61.7% of patients did not value their initial symptoms and in 20% of them the dentist failed to counsel the patient accordingly after dental extraction. The patients visit dentists, general clinicians, neurologists and psychiatrists and that is one cause for the delay to come to specialist (Sisson et al., 1963; Harrison, 1973).The similarity with chronic inflammatory process and the disease confined to the maxillary sinus are referred as causes that explain why the general physician does not counsel patients properly (Sisson et al., 1989; Barbosa, 1979). Despite the low incidence of paranasal sinus cancer, some measures have to be taken to modify this counseling situation, especially because most of these patients will die because of delay in diagnosis. Maybe notions of basic head and neck oncology taught at the schools of Medicine and Odonthology would reduce the delay.
When crossing the variable type of complaint and delay, we noticed that facial edema made patients come to the specialist within 4 months. Nasal obstruction and previous dental extraction took more than 4 months. This fact confirms that facial edema motivates the patient to come to the specialist earlier, a fact that does not happen with nasal obstruction and pain, or dental loosening. This fact confirms the data presented here.
Nasal obstruction, in turn, an uncomfortable symptom associated with infectious and allergic diseases, makes patients come to a cancer specialist much later. Dental pain and extraction is a cause reported by many authors (Andrade Sobrinho,1967; Larisson and Martensson,1972; Barbosa,1979; Kenady, 1986). This symptom is very valuable provided that odonthologists know about clinical and epidemiological factors of cancer and suspect of the disease. Facial edema, nasal obstruction and dental pain were the most frequent symptoms; it did not surprise us that patients went first to Otorhinolaryngologists, dentists, general practitioners and nonmedical professionals. If these professionals were trained to provide proper counseling, they would contribute to early diagnosis.
The time between diagnosis and treatment took 2 weeks in 43.3% of the patients, and it took 2 to 4 weeks in 20% of the cases, taking as much as 8 weeks in some cases. In our opinion, the cause for delay is lack of beds in specialized centers and few resources available in certain regions. We suggest expansion of existing centers and decentralization to optimize therapeutic results. This fact would increase the number of beds and reduce the time between diagnosis and treatment.
Most of our patients had left maxillary sinus predominance. The same was not found in Lederman (1970) data, which did not find side predominance of maxillary sinus. We do not know if side predominance is important or if it was just a coincidence.
CONCLUSION
Based on the data collected and the literature, we concluded that:
1. Education of the general population, teaching of oncology to health professionals and expansion of specialized centers may contribute to reduce the delay in treatment of squamous cell carcinoma of maxillary sinus, resulting in better prognosis.
2. The incidence of squamous cell carcinoma of maxillary sinus was proportionally higher among professionals that manipulated fabrics (tailors and seamstresses) when compared to other professionals.
3. Nasal obstruction and dental loosening and/or dental pain were symptoms that delayed the visit to a specialist and are probably poorly valued by professionals who initially see the patient.
4. The incidence of squamous cell carcinoma of maxillary sinus was higher in male patients, in their 60's, equally distributed among white and non-white patients.
5. There was predominance of the left side (61.7%) over the right side.
6. Smoking may contribute as an additional factor for squamous cell carcinoma of maxillary sinus, as well as chronic sinusitis.
REFERENCES
AHMAD, K.; CORDOBA, R. B.; FAYOS, J. V. - Squamous cell carcinoma of the maxillary sinus. Arch. Otolaryngol., 107: 48-51, 1981.
ALVAREZ, L; SUAREZ, C.; RODRIGO, J. P.; NUNEZ, F.; CAMINERO, M. J. - Prognostic factors in paranasal sinus cancer. Am. J. Otolaryngol., 16: 109-14, 1995.
ANDRADE SOBRINHO, J. de - Tumores malignos das fossas nasais a cavidades paranasais. In: NOBRE, M. O. R.& JUNQUEIRA, A. C. C. - Cancerologia prática. São Paulo, Fundo Editorial Procienx, 1967. p.375-85. v.2
BARBOSA, J. F. - Câncer das cavidades paranasais. In:______ - Câncer da faringe. São Paulo, Manole, 1979. p.31-65.
BAUMSLAG, N. & KEEN, P. - Trace elements in soil and plants and antral cancer. Arch. Environ. Health, 25: 23-5, 1972.
BRASIL. Ministério da Saúde. Secretaria Nacional de Ações Básicas de Saúde. Divisão Nacional de Epidemiologia. - Classificação Brasileira de ocupações para o subsistema de informação sobre mortalidade. Brasília, Centro de Documentação do Ministério da Saúde, 1987. (Serie G: Estatística a Informação em Saúde, 11).
CARVALHO, M. B. & ANDRADE SOBRINHO, J. de - Câncer de seios paranasais. In: LOPES FILHO, O. & CAMPOS, C.A.H. de - Tratado de Otorrinolaringologia. São Paulo, Roca, 1994. p.470-7.
FAVA, A. S. & CARVALHO, M. B. de - Tumores malignos do nariz, cavidades nasais a seios paranasais. In: BRANDAO, L. G. & FERRAZ, A. R. - Cirurgia de cabeça e pescoço: princípios básicos. São Paulo, Roca, 1989. p.493-506. v.1
FUKUDA, K.; KOJIRO, M.; HIRANO, M.; HYAMS, V. J.; HEFFNER, D. - Predominance of squamous cell carcinoma and rarity of adenocarcinoma of maxillary sinus among Japanese. Kurume Med. J., 36 1-6, 1989.
FUKUDA, K.; SHIBATA, A.; HARADA, K. - Squamous cell cancer of the maxillary sinus in Hokkaido, Japan: a case-control study. Br. J. Indust. Med., 44: 263-6, 1987.
HARRISON, D. F. N. - The management of malignant tumours affecting the maxillary and ethmoidal sinuses. J. Laryngol. Otol., 87: 749-72, 1973.
HERNBERG, S.; WESTERHOLM, P.; SCHULTZ-LARSEN, K.; DEGERTH, R.; KUOSMA, E.; ENGLUND, A.; ENGZELL, U.; HANSEN, H. S.; MUTANEN, P. - Nasal and sinonasal cancer: connection with occupational exposures in Denmark, Finland and Sweden. Scand. J. Work Environ. Health, 9: 315-26, 1983.
KAGAN, A. R. & STECKEL, R. S. - Diagnostic oncology case studies. Am. J. Rontgenol., 131: 321-2, 1978.
KENADY, D. E. - Cancer of the paranasal sinuses. Surg. Clin. North Am., 66. 119-30, 1986.
LARSSON, L. G. & MARTENSSON, G. - Maxillary antral cancers. J. Am. Med. Assoc., 219: 342-5, 1972.
LEDERMAN, M. - Tumours of the upper jaw: natural history and treatment. I. Laryngol. Otol., 84: 369-401, 1970.
ROUSH, G. C.; MEIGS. J. W.; KELLY, J.; FLANNERY. J. T.; BURRO, H. - Sinonasal cancer and occupation: a case-control study. Am. J. Epidemiol., 111: 183-93, 1980.
SHAH, J. P. & KOWALSKI, L. P. -Advances in the management of cancer of the paranasal sinuses. Rev. Bras. Cir. Cab. Pesc., 12: 30-40, 1988.
SHIMIZU, H.; HOZAWA, J.; SAITO, H.; MURAI, K.; HIRATA, H.; TAKASAKA, T.; TOGAWA, K.; KONNO, A.; KIMURA,Y.; KIKUCHI, A.; OHKOUCHI, Y.; OHTANI, L; HISAMICHI, S. Chronic sinusitis and woodworking as risk factors for cancer of the maxillary sinus in Northeast Japan. Laryngoscope, 199: 58-61, 1989.
SISSON, G. A.; JOHNSON, N. E.; AMIRI, C. S. - Cancer of the maxillary sinus. Clinical classification and management. Ann. Otol., 72: 1050-9, 1963.
SISSON, G. A.; TORIUMI, D. M.; ATIYAH, A. - Paranasal sinus malignancy: a comprehensive update. Laryngoscope, 99: 14350, 1989.
SPIRO. J. D.; SOO, K. C.; SPIRO, R. H. - Squamous carcinoma of the nasal cavity and paranasal sinuses. Am. J. Surg., 158: 328-32, 1989.
WATSON, W. L. - Cancer of paranasal sinuses. Laryngoscope, 52: 22-42, 1942.
* Otorhinolaryngology, Master Degree in Head and Neck Surgery by Hospital Heliópolis - São Paulo/ SP.
** Doctorate Degree in Head and Neck by Universidade Federal de São Paulo. Head of the Course of Post-Graduation in Head and Neck Surgery at Hospital Heliópolis São Paulo/ SP.
Study presented at 34° Congresso Brasileiro de Otorrinolaringologia, held in Porto Alegre/ RS on November 22, 1998.
Master Dissertation for the Post-Graduation Course of Head and Neck Surgery at Complexo Hospitalar Heliópolis - São Paulo/ SP.
Financial support by CAPES.
Address for correspondence: Jose Castro Lima Geraldes Filho - Serviço de Cirurgia de Cabeça a Pescoço do Hospital Aristides Maltez.
Avenida João Vl, 332 - Brotas, Salvador/ BA - E-mail: geraldes@e-net.com.br
Article submitted on September 14, 1999. Article accepted on May 25, 2000.