Year: 2000 Vol. 66 Ed. 4 - (1º)
Artigos Originais
Pages: 310 to 314
Inlay Cartilage Tympanoplasty: First Brazilian Results.
Author(s):
José F. Lubianca Neto*,
Marcelo Mauri**,
Daniela B. da Silva**,
Josemar R. Machado**.
Keywords: tympanoplasty, cartilage, condutive hearing loss
Abstract:
Purpose: Myringoplasty techniques include either an underlay or an onlay approaches using temporalis fascia or perichondrium as grafts. Roland Eavey in 1998 described a transcanal cartilage butterlly inlay tympanoplasty technique in children. This technique was found to be effective to close tympanic membrane perfurations, more comfortable and less morbid (no external canal incisions). The aim of this study was to describe our results with Eavey's technique, with little modifications. Material and method: Cartilage butterfly tympanoplasty was carried out in seven adult patients to close small to medium tympanic membrane perfurations from March to July, 1998. We introduced three modifications into Eavey's technique: 1. we used adult patients, 2. the surgeries were performed under local anesthesia and 3. we use no skin graft over the cartilage. We evaluated the take rate and postoperative hearing results. Results: All patients had postoperative hearing gain and the take rate was 100% at short-term follow-up period (medium 22.7 months). All cartilage grafts were intact and dry at the last follow-up visit. All patients showed improvement in their audiometric postoperative results. Two of them got closure of their air-bone gap and the rest of them diminished it to 50%. Conclusion This technique described by Eavey is effective to close tympanic membrane perfuration in adults. The modifications introduced (no use of skin graft and local anesthesia) reduced even more surgery time and did not alter postoperative results of the original technique.
![]()
INTRODUCTION
Conventional techniques for closure of tympanic perforations use fascia, periosteum or meninges grafts, among other tissues, which may be placed medial or lateral to tympanic ring, requiring skin incision of auditory canal and creation of tympanic-meatal flap, what increases morbidity of surgery and need for postoperative care10,14. Gross et al.1 described the technique using fat to close tympanic membrane. Theoretical advantages included reduction of surgical time and technical facility if compared to other surgical modalities. However, some authors discussed the efficacy of this technique because of inconsistency of postoperative results6. In 1998, Roland Eavey6 described the technique of butterfly cartilaginous graft, placed over the perforation, for treatment of solution of continuity in children's tympanic membrane. This technique has shown a number of practical advantages during surgical act and in postoperative follow-up, including: 1) technical facility; 2) lower morbidity, because canal incision is not required; 3) more stability of graft, reducing postoperative care; 4) immediate post-op audiological results, because of absence of canal dressing; 5) reduction of surgical time, and above all 6) rate of graft take of 100%6.
This study aimed at presenting postoperative results of tympanoplasty described by Roland Eavey, but incorporating the following modifications: use of technique in adults, use of local anesthesia and without placement of skin graft over the cartilage.
MATERIAL AND METHOD
1. Patients
We performed 7 surgeries in patients aged 15 to 50 years, 5 female and 2 male patients. One patient had previous history of myringoplasty, performed through conventional technique 9 years before. Surgical indication was simple chronic otitis media in all patients. All surgeries were performed by the authors at Complexo Hospitalar Santa Casa de Porto Alegre, between March and July 1998.
The size of perforations varied, from 2x1mm to 4x3mm. All ears were apparently healthy, despite the fact that some of them had tympanosclerosis. Pre and postoperative hearing levels and tympanic membrane characteristics are described in Table 1. Pre and postoperative audiometric assessment was conducted in our Service and the analysis of postoperative audiometric results followed the latest recommendations by Committee on Hearing and Equilibrium guidelines for the evaluation of results of treatment of conductive-hearing loss of the American Academy of Otorhinolaryngology and Head and Neck Surgery2. We used the mean difference between air and bone thresholds in frequencies 500 Hz, 1.000 Hz, 2.000 Hz and 3.000 Hz to evaluate post-op results.
2. Surgical technique
Patients were sedated with midazolan and phentanyl and prepared for a sterile procedure, with placement of operative fields. Next, we infiltrated tragus and external auditory canal using local anesthetics associated with vasoconstrictor (lidocaine and epinephrine 1:50.000).TABLE 1 - General characteristics of patients, pre and post-op tympanic membrane status and pre and post-op audiometric gap.
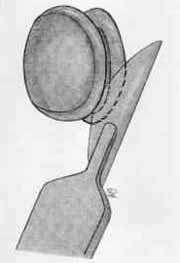
Figure 1. Cartilage graft after incision of all the circumference between perichondriums, shaping as butterfly.
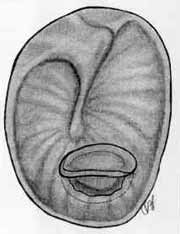
Figure 2. Aspect of cartilage graft to be placed over the tympanic perforation.
Tympanic perforation was visualized under microscopy and the margins were revitalized but avoiding increase of perforation. Next, size of perforation was carefully measured using a 2mm long hook of straight angle.
Cartilage graft was harvested from tragus through an incision of 8 to 10mm, conducted between tragus dome and external acoustic canal using a #15 knife. We made one single incision of skin, subcutaneous and cartilage. Exposure of cartilage was made using hooks and a small dissection pair of scissors to release the cartilage from adjacent tissues (dome of tragus was preserved), preserving as well the perichondrium adhered to the cartilage on both sides. After proper hemostasia, the skin was sutured with mononylon 6.0.
Next, we created the cartilaginous graft oriented by the same hook of straight angle used to measure the size of perforation. Graft molding was conducted with microsurgery knife (Beaver #6700 mini-blade®) under microscopic view, making sure that the final graft size would be 2mm larger than that of the perforation. We performed a deep incision around the circumference of the graft parallel to both perichondriums, but not totally- into medial plan. Therefore, we created two laminae of cartilage joined in the center and externally recovered by perichondriurn. The tension of the perichondrium bent instantaneously the margins of both laminae of cartilage in all its circumference. The final shape of the graft, seen in profile, looked like a butterfly (Figure 1).
The graft was placed on the perforation under microscopic view, as if it were a ventilation shunt. We were careful in order to guarantee that in all the circumference of the perforation the medial lamina of the graft was placed on the middle ear, whereas the lateral lamina of external ear was placed over the tympanic membrane (Figure 2). At that moment, auditory gain was tested subjectively. Differently from what Eavey6 recommended, we did no place a skin graft over the cartilage positioned on the tympanic membrane.
We did not place dressing in the middle ear, external auditory canal or pinna. We advised patients not to wet the ear in the first month after surgery. Antibiotic drops were used once a day in the 1st postoperative week, despite the fact that this practice is not evidence-based medicine.
RESULTS
Closure of perforation was present in 100% of the patients, followed up for an average of 19 to 24 months (mean follow-up of 22.7 months). All patients reported subject improvement of hearing on the first post-op week. No significant postoperative complications were present. During follow-up, there was a case of granular myringitis adjacent to the cartilaginous graft, which was readily treated with local chemical cauterization in one visit. Among all other patients, the graft remained dry (Figure 3). We did not observe problems in the tragus incision. Pre and post-op audiometric assessments are shown in Table 1.
Figure 3. Aspect of cartilage graft on tympanic membrane after the first week follow-up.
DISCUSSION
The use of cartilage in middle ear surgeries has been demonstrated by various authors, with good tolerability of graft in the middle ear, both in clinical and in experimental studies8,4,3 Some authors described that the cartilage was nourished by diffusion and, with time, became incorporated to the tympanic membrane6,11.
The use of cartilage grafts was widely reported for treatment of posterior and apical retraction pockets. The authors described excellent results from anatomical standpoint, reducing significantly recurrence of retractions. However, they did not describe postoperative audiometric results8,11,15. This was the reason for controversy among some otological surgeons concerned about the hearing impact of using rigid material, such as cartilage, for closing the perforations.
Lately, some authors have described their results of cartilage grafts in perforations of the tense portion of tympanic membrane, with high level of graft take and no deterioration of hearing levels4,1,12. Dornhoffer (1997) demonstrated that size of perforation, and consequently, quantity of cartilage used, did not influence significantly post-op audiometric results. The author compared also differences in audiometric results when using cartilage or perichondrium for tympanic reconstruction. He did not detect statistically significant differences between both techniques4. Finally, Eavey (1998) reported his results with the same technique used in our study. He showed an rate of graft take of 100% and hearing gain in 90% of the patients6.
In our study, we observed a rate of graft take of 100% and auditory gain in all patients, despite the introduction of modifications. The technique showed high reproducibility and promising results, even though we had a short follow-up of patients. The technical modifications we introduced did not impair the results obtained with the original technique by Eavey. In fact, they showed that this technique may also be used in adult patients and carried out under local anesthesia, without discomfort to the patient and potential complications of general anesthesia.
We demonstrated that fail to place skin graft over the cartilage did not modify post-op results, despite the fact that the graft would theoretically reduce healing time of tympanic membrane. Conversely, harvest of skin graft from the arm increases surgical time, post-op care and total morbidity of the surgery.
Local ear factors may either facilitate or hinder the success of the surgery. It is not necessary to remove tympanosclerosis plaques during surgery. In fact, such plaques make the remaining tympanic membrane more rigid and promote better sustentation of the cartilage graft without impairing the nourishment of the graft. On the other hand, granular myringitis may increase the rate of graft rejection. Because of that, we recommend very intense treatment of this affection pre and postoperatively. Eavey's technique should be avoided in cases of marginal perforation and if middle ear exploration is required.
The success rate reported by Rizer13 using underlay technique with transcanal access in 427 patients was 87.6% (374 patients). A complete closure of the gap was observed in 52% (222 patients), a gap between 0 and 15 dB in 89.2% (381 patients), and between 0 and 30 dB in 95.8% (409 patients). Other authors reported their casuistic as well - Doyle et al. (1972) using the same technique but retroauricular access, observed a success rate of 83% in the first post-op year. Audiometric results showed post-op improvement in 62% of the patients, worsening in 7% and no alteration in 31% of the patients.
Glassocock (1973), using underlay technique with retroauricular access in 180 patients - among which 75 were submitted to tympanoplasty, 88 to tympanomastoidectomy and 17 to mastoid reconstruction - had success rate of 96%7.
CONCLUSION
Eavey's technique is highly effective also for adults, with less morbidity when compared to conventional myringoplasty. Fail to use skin graft and use of local anesthesia seem to reduce even more surgical time and do not hinder the results of the original technique.
We concluded that Eavey's technique added by the modifications proposed here is effective and has excellent post-op results also in adult patients who have small to middle-sized tympanic perforations.
REFERENCES
1. AMEDEE, R. G.; MANN, W. J.; RIECHELMANN, H. - Cartilage palisade tympanoplasty. Am. J. Otol. 10: 447-450; 1989.
2. Committee on Hearing and Equilibrium - Committee on Hearing and Equilibrium guidelines for the evaluation of results of treatment of conductive hearing loss. Otolaryngol. Head Neck Surg., 113: 186-187, 1995.
3. DON, A.; LINTHICUM, F. H. - The fate of cartilage grafts for ossicular reconstruction in tympanoplasty. Ann. Otol. Rhinol. Laryngol., 84: 187-191, 1975.
4. DORNHOFFER, J. L. - Hearing results with cartilage tympanoplasty. Laryngoscope, 107: 1094-1099, 1997.
5. DOYLE, J. P.; SCHLEUNING, A. J.; ECHEVARRIA, J. Tympanoplasty: should grafts be placed medial or lateral to the tympanic membrane. Laryngoscope, 82: 1425-30, 1972
6. EAVEY, R. D. - Inlay tympanoplasty: cartilage butterfly technique. Laryngoscope, 108: 657-661, 1998.
7. GLASSCOCK, M. E. III. - Tympanic membrane grafting with fascia: overlay vs. undersurface technique. Laryngoscope, 83: 754-70.1973.
8. GLASSCOCK, M. E.; JACKSON, C. G.; NISSEN, A. J.; SCHWABER, M. K. - Postauricular undersurface tympanic membrane grafting: a follow-up report. Laryngoscope, 92: 718-727, 1982.
9. GROSS, C. W.; BASSILA, M.; LAZAR, R. H.; LONG, T. E.; STAGNER, S. -Adipose tissue plug myringoplasty: an alternative to formal myringoplasty techniques in children. Otolaryngol. Head Neck Surg., 101: 617-620, 1989.
10. KURKJIAN, J. M. - Perforations of the tympanic membrane. In: Nadol. J. B.; Schknecht, H. F. - Surgery of Ear and Temporal Bone. New York, Raven Press Ltd., 1993, 121-137.
11. LEVINSON, R. M. - Cartilage-perichondrial composite graft tympanoplasty in the treatment of posterior marginal and attic retraction pockets. Laryngoscope, 97: 1069-1074; 1987.
12. MILEWSKI, C. - Composite graft tympanoplasty in the treatment of ears with advanced middle ear pathology. Laryngoscope, 103: 1352-1356, 1993.
13. RIZER, F. M. - Overlay versus underlay tympanoplasty. Part II: The study. Laryngoscope, 107: 26-36, 1997.
14. SHEEEHY, J. L. - Tympanoplasty: outer surface grafting technique. In: Brackman, D. E.; Shelton, C.; Arriaga, M. A. - Otologic Surge. Philadelphia, WB Saunders CO., 1994, 121-132.
15. SHEEHY, J. L. - Surgery of chronic otitis media. In: English G - Otolaryngology, vol.1. (revised edition). Philadelphia: Harper and Row, 1985:1-86.
* Assistant Professor of the Discipline of Otorhinolaryngology at FFFCMPA/CHSC. Head of the Ambulatory of Otorhinolaryngology at CHSC. Ex-Fellow of the Department of Otorhinolaryngology at Massachusetts Eye and Ear Infirmary-Harvard Medical School-Boston, USA.
** Resident Physician of the Service of Otorhinolaryngology at FFFCMPA/CHSC.
Study conducted at the Discipline of Otorhinolaryngology, Fundação Faculdade Federal de Ciências Médicas de Porto Alegre and Service of Otorhinolaryngology of Complexo
Hospitalar Santa Casa (FFFCMPA/ CHSC), Porto Alegre, RS.
Address for correspondence: Dr. Jose Faibes Lubianca Neto - Rua Coronel Corte Real, 122 - Apt°. 603 - 90630-080 Porto Alegre /RS.
Tel / Fax: (55 51) 346-3831 - E-mail: jlubianca@zaz.com.br
Article submitted on August 26, 1998. Article accepted on May 19, 2000.