Year: 2003 Vol. 69 Ed. 6 - (19º)
Relato de Caso
Pages: 851 to 854
Pacinian neurofibroma: report of a rare intraoral case
Author(s):
Lélia B. Souza1,
Jamile M.B. Oliveira2,
Tarsila M. C. Freitas3,
Rejane A. Carvalho4
Keywords: neurofibroma, Pacinian corpuscle, oral mucosa
Abstract:
Pacinian Neurofibroma is a rare lesion that has been reported predominantly on the hand, including the digits, on buttocks and feet. The lesions can be solitaries or multiples as part of the Von Recklinghausen's disease. The intraoral site is unusual and just one case has been related in the world's literature. The purpose of this report is to present one case of pacinian neurofibroma and to describe its clinical and histopathological features contributing for the best knowledge about this entity.
![]()
Introduction
Pacinian neurofibroma is an uncommon benign tumor that originates from the peripheral nervous endings characterized as a histology variant of neurofibroma since it presents components that are similar to Vater-Pacini corpuscles. The purpose of the present study was to report a rare case of Pacinian neurofibroma of intra-oral location, as well as to describe its clinical and histopathological characteristics, contributing to further knowledge of this entity.
Literature Review
Benign neural tumors are lesions that originate from the peripheral nerves and represent about 45% of the neoplasms that reach the region of the head and neck, and the high incidence in this area is explained by the relatively large amount of peripheral nervous endings grouped there. Despite the fact that they show the same neural origin, they present marked microscopic and pathogenic heterogeneity that convey a varied pattern of clinical and histology presentations. Oral lesions are rare. They affect preferably the tongue (50% of the cases) and include neurofbroma, schwannoma, nervous sheath myxoma, encapsulated palisade neuroma, traumatic neuroma, granular cell tumor and mucosa neuromas of the multiple endocrine neoplasm syndrome type III 1, 2.
Neurofibroma is the most common type among these neoplasms and it can be solitary or multiple, as components of neurofibromatosis 3. The skin is the most frequent location, however, the intraoral lesions are not uncommon, and they can be peripheral, especially on the tongue, or more central 4. From a histology perspective, the tumor consists of a mixture of schwann cells, perineural and endoneural fibroblasts, and occasionally they can show structures that are similar to specialized pressure receptors named Pacini corpuscles, known as pacinian neurofibroma 5, 6.
Pacinian neurofibroma was initially described in the literature by Prichard and Custer in 1952 as a rare lesions found predominantly on the hands, including the digits, feet and buttocks region, affecting preferably adolescents and young adults. The lesion can be solitary or multiple, as components of the Von Recklinghausen's disease, characterized by multiple neurofibromas, cafe-au-lat skin spots, bone abnormalities, in addition to central nervous system lesions. In the oral cavity, pacinian neurofibroma is a uncommon finding, which can be evidenced in the gingival region as an exophitic tumor mass that is well delimited, of soft consistency and slow growth, occasionally involving the underlying bone. Radiological examination reveals a radiolucent image, plus radicular divergence 2, 6, 7.
The differential diagnosis of this entity should be conducted with lesions such as pyogenic granuloma, peripheral lesions of giant cells, and peripheral ossifying fibroma, which are all reaction lesions that affect the gingival tissue and because they show similar clinical aspects, it may hinder diagnosis 4.
As to histopathological characteristics, pacinian neurofibroma is characterized by a cell pattern of concentric lamellar arrangement, comprising spindle cell compounds, similar to Vater-Pacini corpuscles. They vary in size and comprise the extensive portion of the cell elements, being surrounded by dense stroma with hyaline areas. Pacinian corpuscles are the largest neural endings of human beings, normally found in the subcutaneous cell tissue, in submucous, subserous layers of various organs, in joints and in the mesentery around the pancreas. In these situations, such as in cases of neurofibromas, similar formations to such corpuscles can be evidenced 2, 8, 9.
CASE REPORT
R.S., female 14-year-old patient, came to the Stomatology Clinic, Program of Post-Graduation in Oral Pathology, Dental School, UFRN, complaining of gingival growth. The clinical intraoral examination revealed the presence of an exophitic lesion located in the buccal gingival region, close to elements 41 and 42, showing hyperplastic aspect, identical color to the surrounding mucosa, measuring about 1.5cm in diameter, sessile implementation and firm consistency upon palpation (Photo 1). We conducted radiological study by peri-apical and posterior-anterior view of the face, and did not find any abnormalities. According to the patient, the lesion was non-painful and presented an evolution of approximately three years, not associated with traumatic factors. Based on the diagnostic hypothesis of peripheral ossifying fibroma, we conducted excision biopsy.
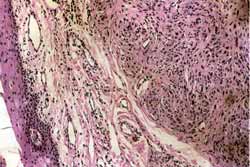
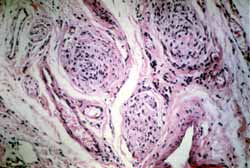
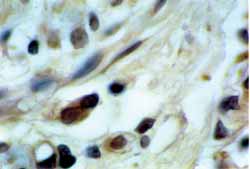
The material sent to clinical pathology analysis showed macroscopic characteristics of soft tissue, brown in color, firm consistency and we observed benign neoplasm of mesenchymal origin characterized by spindle cell proliferation with elongated nucleus and clear cytoplasm, arranged as pacinian distribution or in layers. In some areas of the lesion, the analysis showed dissociation of muscle fibers by neoplastic cells. Complementing the histology picture, we observed presence of stratified pavement epithelial tissue typical of the oral mucosa recover, as well as muscle fibers placed inside the specimen (Photos 2 and 3). Considering this histopathologic picture, we made the diagnosis of Pacinian neurofibroma. Even though it was possible to identify the lesion only with routine staining with hematoxillin-eosin, the specimen was submitted to immunohistochemistry for protein S-100, presenting positive reactivity to this neural cell marker (Photo 4).
Photo 1. Clinical aspect of the lesion of Pacinian neurofibroma showing smooth surface, located in the inserted gingival region.
Photo 2. Histology aspect of Pacinian neurofibroma evidencing proliferation of cells of concentric lamellar arrangement (H/E 100x).
Photo 3. Photomicrography in greater enlargement showing structures similar to Vater-Pacini corpuscles (H/E 200x).
Photo 4. Immunohistochemical staining for protein S-100 in pacinian neurofibroma (Estreptoavidin-biotin, 200x).
Discussion
Neurofibroma is a benign tumor that is originated from the peripheral nerve sheath which can occur as part of neurofibromatosis type I (Von Recklinghausen's disease), or more commonly, as single lesions 10. Solitary lesions occur in many anatomical locations, including the oral mucosa. A wide spectrum of histology patterns in many distinct variants has been reported in the literature, including the uncommon presence of Vater Pacini corpuscles, since they are preferably observed in subcutaneous, submucous, subserous cell tissues, joints and mesentery.
The case reported here presented a single lesion of exophitic growth, located in the vestibular gingival region adjacent to elements 41 and 42, with no evidence of neurofibromatosis type I (Von Recklinghausen's disease), confirming the findings by McCormack et al.7, who in a meta-analysis of 28 cases of pacinian neurofibroma did not find this association. The radiological examination did not show impairment of the underlying bone, differently from the findings by Toth, Long, Pleasants2, who evidenced radiolucent radiological image associated with the lesion.
The hyperplastic aspect of the lesion hindered its clinical diagnosis, since the many entities that affected the gingival mucosa showed similar patterns, which made us come up with the hypothesis of peripheral ossifying fibroma and fibrous hyperplasia. Local tumefaction, conversely, made us think about osteoma. Therefore, the consideration of the lesion is essential for differential diagnosis. The treatment adopted with the pacinian neurofibroma, as reported by the literature 2, 13, was based on local surgical incision, through an excision biopsy, and the specimen was sent to microscopy analysis.
The histopathology findings were essential for the definite characterization of the lesion, confirming the findings by Bennin, Barsky, Salgia2; McCormack et al.7; Toth, Long, Pleasants2; Wolfgang Jurecka9 , who evidenced the presence of a cell pattern of concentric lamellar arrangement, comprising spindle cells, similar to Vater-Pacini corpuscles.
In addition to histopathological examination, the immunohistochemical markers have been used as a diagnostic option to identify skin neural tumors and to determine cell line. Antigenic markers are capable of determining the neural origin, such as for example protein S-100, CD-57 and epithelial membrane antigen 1, 14. In this case, even though we had identified the lesion only with routine hematoxillin-eosin staining, the piece was submitted to S-100 protein immunohistochemistry analysis, and there was positive tumor reaction to the neural cell marker. The efficacy of this protein, as reported in the literature, was tested by Chrysomali et al.1 in their study of 77 cases of neural tumors, being confirmed that it is capable of identifying schwann cells in mesenchymal tumors of neural origin and differentiation.
The occurrence of a large percentage of neural tumors in the head and neck region (45%) is attributed to the relatively high number of peripheral nerves endings grouped in this area 2. In our opinion, the lesion reported can have been originated from the nervous ending coming from the inferior alveolar nerve by an unknown stimulus, since the patient did not report history of trauma during the anamnesis.
CLOSING REMARKS
In the literature there are few reports about pacinian neurofibroma, being that it is normally reported in the hands, feet and buttocks regions and rarely in the oral cavity. The lesion can in some situations be associated with Von Recklinghausen's disease, which is characterized by multiple skin lesions, which makes it relevant to careful clinical and physical examination of the patients. We should not forget, therefore, about the importance of the histopathology analysis, which was essential for the definition of the diagnosis by the presence of similar structure to Vater-Pacini corpuscles.
References
1. Chrysomali E et al. Benign neural tumors of the oral cavity: a comparative immunohistochemical study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997; 84: 381-90.
2. Toth BB, Long WH, Pleasants JE. Central pacinian neurofibroma of the maxilla. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1975; 39:630-4.
3. Silva FM et al. Neurofibromatose múltipla. UNIMEP 2001; 13:14-16.
4. Neville BW et al. Tumores de tecidos moles. In:___________. Patologia Oral e Maxilofacial. 2ª ed. Rio de Janeiro, Guanabara: Koogan; 1998. p. 353-404.
5. Enzinger FM, Weiss SW. Soft tissues tumors. 2ª ed. St. Louis: C.V. Mosby; 1988:1-741.
6. Regezi AJ, Sciubba JJ. Lesões do tecido conjuntivo. In:__________. Patologia bucal: Correlações clínicopatológicas. 3ª ed. Rio de Janeiro, Guanabara: Koogan; 2000:158-94.
7. McCormack K et al. Multiple hairy pacinian neurofibromas (nerve- sheat myxomas). J Am Acad Dermatol 1988; 18: 416-9.
8. Guidugli Neto J. Neurofibroma Paciniano (corpúsculos de Pacini alargados) intraperitoneal. Rev Paul Med 1990; 108:192-3.
9. Wolfgang Jurecka MD. Tactile corpuscle-like structures in peripheral nerve sheat tumors in plastic embedded material. Am J Dermatopathol 1988; 10:74-9.
10. Araújo ACPF et al. Neurofibromatose e gravidez: relato de caso. R Saúde 1998; 12:47-51.
11. Bennin B, Barsky S, Salgia K. Pacinian Neurofibroma. Arch Dermatol 1976; 112:1557-8.
12. Shimoyama T et al. Solitary neurofibroma of oral mucosa: a previously undescribed variant of neurofibroma. J Oral Science 2002; 44:59-63.
13. Campora E, Radici M, Campora L. Neurogenic tumors of the head and neck in children. Int J of Pediatric Otorhinolaryngol 1999; 49:231-3.
14. Jordan RCK et al. Advanced diagnostic methods in oral and maxillofacial pathology. Part II: Immuohistochemical and immuofluorescent methods. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 93:56-74.
1 Ph.D., Professor, Discipline of Oral Pathology, Program of Post-graduation in Oral Pathology, / UFRN.
2 Post-graduation studies in Oral Pathology under course, / UFRN (Master).
3 Post-graduation studies in Oral Pathology under course, / UFRN (Master).
4 Ph. D., Professor, Program of Post-Graduation in oral Pathology / UFRN.
Affiliation: Federal University of Rio Grande do Norte (UFRN).
Address correspondence to: Drª. Lélia Batista de Souza - Av. Salgado Filho, 1787 Lagoa Nova Natal RN 59056-000.
Tel (55 84) 215-4132/ 215-4138 - Fax: (55 84) 215-4138
E-mail: leliasouza@dod.ufrn.br/ taifreitas@ig.com.br/ jamile.marinho@bol.com.br
Study presented at III Congresso Brasileiro de Estomatologia/ XXI Jornada Brasileira de Estomatologia, Gramado-RS, July 18 - 22, 1995.
Article submitted on December 20, 2002. Article accepted on February 13, 2003.