Year: 2003 Vol. 69 Ed. 6 - (3º)
Artigo Original
Pages: 744 to 751
Comparative study of absortion of three kinds of collagen used in otologic surgery
Author(s):
Cristina Dornelles1,
Sady S. da Costa2,
Márcia Laux3,
Raimar Weber4
Keywords: collagen, chronic otitis media, otologic surgery
Abstract:
Introduction: Ethicon, Gelfoam and Lyostyp are three kinds of supporters that are made of collagen. They are used in otologic surgery as a base-suport to grafts. Some procedures demand a bigger permanence of support, others need a rapid absortion. There is not studies to prove the differences among this three kinds of supporters. The subject this study was measure the difference of absortion among three supporters. Study design: Experimental. Material and Method: We used 124 fragments of supporters measuring 5 X 5 X 1 mm. The fragments was placed in Petry's plaques with Agar-agar (62 open and 62 closed plaques) inside a stove warmed to 37º C. Each case plaque received 1 ml of total blood and each control plaque received 1 ml of 0,9% NaCl in the days 1, 7 and 14. The area measurement was done in a period of three weeks using a paquimeter with diary measurements in the first week and afterthat each 48 hours. The sample-size was determinated by the maximum capacity of stove. Statistics analisis was done using the SPSS 8.0 software, through repeated variance measurements. Results: There was not difference between blood and 0,9% NaCl in the area measurements. In closed plaques, was not statistic differences between Gelfoam and Ethicon (p=0,21), but Lyostyp absortion was statistical different from the other two supporters (p=0,001 and p=0,006). In opened plaques, was not significative differences among the three kinds of supporters (p>0,05).
![]()
INTRODUCTION
Ethicon, Gelfoam® and Lyostyp are collagen compounds used as degradable sponges that after wetted, tend to have a jelly presentation, being used as cube-shaped support-base for grafts in ear surgeries, employed as if they were a supporting blanket for the graft, or in small strips or "trails" (Costa, S.S.; Dornelles, C. and Carvalhal, L.H.S.K., 2000). In Table 1, we can find a list of the indications and contraindications for the use of these substances.
Collagen is the most abundant protein in the animal kingdom, being the main component of bones, skin and connective tissues of all mammals (Stryer, L., 1996).
The degradation of collagen in the extracellular matrix is obtained by a family of collagenase that suffers cleavage of intact fibers in smaller fragments; they can then suffer phagocytosis and later they are degraded by lysosomic enzymes, down to its constituent amino acids (Champe P.C. and Harvey R.A., 1996).
Lysosomes contain a variety of hydrolytic enzymes, including acid phosphatase, glucoronidase, sulphatase, ribonuclease and collagenase. These enzymes are produced at the rugous endoplasmatic reticulum, compacted by Golgi's system, named primary lysosome. They fuse with vacuoles linked to the membrane that contains material to be digested, and are named phagosome. The next step is the process of heterophagia, in which external materials are captured by endocytosis, submitted to phagocytosis. The cells involved in the process are neutrophils and macrophages (Cotran R.S., Kumar V., Robbins S.L., 1997).
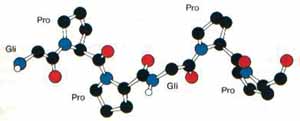
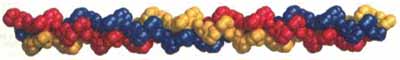
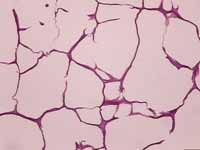
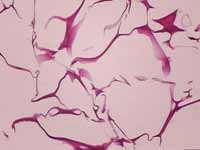
Collagen is a rod-shaped molecule forming a triple helix with about 3,000Å in length and 15Å in diameter (Okuyama, K.K. et al., 1981) (Figures 1 and 2).
The stability of the collagen triple helix is maintained by bridges of hydrogen between the filaments and by an esteric effect of prolines and hydroxiprolines (Stryer, 1996).
The temperature of dissolution of collagen is very different in each type, but in all of them it is only slightly higher than body temperature, in the case of bovine collagen it is 39oC.
In ear procedures, the sponges can be placed in the middle ear and the auditory tube orifice to occlude them completely, and at the same time they serve as support to the anterior portion of the graft (Cruz, O.L.M. and Costa, S.S., 1999).
The graft works as a replacement of the corneal stratum over which the epithelialization currents run along, in order to repair the perforation. During the process, lateral tympanic layers (epithelial) and medial (mucosa) regenerate perfectly.
Only in the 50's, based on the studies by Wullstein (1952) and Zöllner (1955) the techniques of middle ear tympanoplasty were introduced and, for the first time, the proposition of functional restoration of the middle ear started to be effectively considered. As of the 60's, Gelfoam was introduced in these surgeries, working as a support (Scheeny, J.L. and Perkins, J.H., 1975), but the research and development of this product had started in 1940 by Correll et al., in 1945, who managed to produce a spongy substance made of jell-o which they named Gelfoam.
Regardless of the different techniques of tympanoplasty and mastoidectomy, Ethicon, Gelfoam, Lyostyp or similar products are employed as facilitators of the fixation of grafts. In some other techniques, there is no need to have long time graft support permanence, whereas in other, there is the need to have quick dissolution. However, there are no studies that justify the use of Ethicon, Gelfoam or Lyostyp in different situations.
The purpose of the present study was to measure the differences in dissolution of the three brands of collagen sponges, Ethicon, Gelfoam and Lyostyp.
MATERIAL AND METHODS
This study was developed by the Bank of Ear Implants, Zone 19, Hospital de Clínicas de Porto Alegre - HCPA/UFRGS. The study was completely conducted in vitro. The object of the study was the different brands of collagen, whose outcomes are the measures of the total area of the studied sponges every 24 hours during the first week, and every 48 hours in the subsequent weeks.
Materials:
In this study we used 124 Petry plates, plastic and sterile with Agar-Agar as substrate. We used total blood with preserved enzymatic activity, previously tested and released for use, and there was no identification of donor, provided by the Blood Bank of HCPA. For controls we used sterile solution.
The three bands of sponges used were Ethicon, Gelfoam and Lyostyp, measuring 5 x 5x 1mm. The size was based on the practical use of the products.
Methods:
Technique:
After extensive literature review, we did not find references about the object of our study. Therefore, it was necessary to develop a technique through pilot testing, which was previously carried out.
The test was conducted in three batteries each one for a 3-week period. Each battery comprised 42 plates, 21 open and 21 closed, in which we equally distributed samples of Ethicon, Gelfoam and Lyostyp. The plates received new blood or sterile solution, in day one, seven and 14, distributed as shown in Table 2. The systems were maintained in heat oven at 37o C (Figure 3 and 4).
Analysis of outcomes:
We considered the sponge shape as flatly, regardless of height. The areas obtained were measured in the four sides, following the formula: Area = [(L1+ L3)/2] x [(L2+ L4)/2].
It was not possible to make the experience as a blind examiner once there were macro-morphological differences between the three tested brands, which could be easily differentiated by looking at them. Therefore, the measurements were made by two examiners, and the mean assessment was considered for the results. The checks were made using pachymeter every 24 hours in the first 6 days and every 48 hours up to day 21. Moment zero was determined as 10 minutes after adding 1ml of blood or sterile solution, in which we made the second measurement, being that the first moment was for sample sectioning.
Statistical Analysis:
We did not find literature references to use in this study, therefore it was not possible to use a statistical method to calculate the size of the sample. Regardless, the size was determined by the maximum capacity of the heat over used.
To better understand the results, the measures of the areas were converted in percentage, being that 100% was the value of moment zero. For each moment, the data were presented as mean and standard deviation. The comparison between the brands was made through analysis of variance of repeated measures, general linear model, using software SPSS 8.0 for windows. Values with p below 0.05 were considered statistically significant.
Figure 1: Conformation of a single filament of collagen triple helix.
Figure 2: Compact model of the collagen triple helix. The three filaments are shown in different colors. Extracted from L. Stryer, Bioquímica - 4ª edição, designed and coordinated reported by K. Okuyama, K. Okuyama, S. Arnott, M. Takayanagi and M. Kakudo. J. Mol. Biol. 152(1981):427.
Figure 3: Picture of a system.
Figure 4: Photo of the heat oven system.
Figure 5. = Sterile solution; Blood.
Figure 6. = Ethicon (n=9), = Gelfoam (n=13), = Lyostyp (n=16).
Figure 7. = Ethicon (n=9), = Gelfoam (n=11), = Lyostyp (n=9).
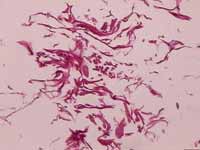
Figure 8: Histology section of sample of Ethicon. Magnification of 100x.
Figure 9: Histology section of sample of Gelfoam. Magnification of 100x.
Figure 10: Histology section of sample of Lyostyp. Magnification of 100x.
RESULTS
Out of the initial number of 124 plates, 40 were excluded because they presented growth of fungi at some time during the observation.
As to use of blood or sterile solution, there was no statistically significant difference (p=0.21) in variance of sponge measures, as shown in Table 3 and Figure 5.
In Table 4 (open plates) and Table 5 (closed plates) we present the measure of each of them at each moment. The general linear model of variation of means concerning time is graphically presented for open and closed plates in Figures 6 and 7, respectively.
The differences in mean areas are presented in Table 6 for the statistical analysis using CI=95%. In the closed plate, Ethicon had slower absorption, Gelfoam had intermediate profile and Lyostyp was faster. When we compared the extremes, that is, Ethicon and Lyostyp, we found statistically significant difference (p=0.006); the comparison of Gelfoam and Lyostyp also had statistically significant difference (p=0.001), but the comparison between Ethicon and Gelfoam had no statistically significant difference (p=0.21).
In open plates, Gelfoam maintained its intermediate profile, but there was an inversion for the performance of Lyostyp and Ethicon. There were no statistically significant differences. Compared one to one: Ethicon and Lyostyp (p=0.15), Gelfoam and Lyostyp (p=0.18) and Ethicon and Gelfoam (p=0.8).
Figures 8, 9 and 10 present photos of histological sections of samples of Ethicon, Gelfoam and Lyostyp.Table 1: Indications and contraindications of absorbable sponge use.
Table 2: Distribution of Petry plates.
Table 3: Variance of measures of the area of samples and controls.
IC = Confidence interval.
Table 4: Mean areas in Open Plate.
Data for each moment are presented as mean (standard deviation).
Table 5: Mean areas in Closed Plates.
Table 6: Difference of the means in area.
* statistically significant difference
DISCUSSION
Ear surgery has been through gradual progression up to reaching the state-of-the-art level we are in today. The journey started with the description of the middle ear physiology by Herman Hemholtz in 1868 (Sambaugh GE, Glasscock ME, 1980). However, only in the 50's, based on the studies of Wullstein and Zöllner, the techniques of tympanoplasty were introduced; for the first time, the proposition of functional restoration of the middle ear was effectively considered. That was the onset of a new and beautiful era for ear surgery: tympanoplasty.
Currently, middle ear surgeries to solve inflammatory processes (tympanoplasty, tympanomastoidectomy) or to repair the tympano-ossicle system (tympanoplasty for reconstruction, stapedectomy), employ a series of materials and organic and inorganic compounds. These materials have been used to repair the tympanic membrane (vein, fascia, perichondrium and periosteum), to reconstruct the ossicle chain (autologous or homologous ossicles, gold, steel, teflon, ceramics, titanium) and to reconstruct bone defects (bone dust, muscle flaps, hydroxiapatite).
In addition to these materials, a series of other compounds has been used as effective and indispensable adjuvant for ear surgery. Among them, we can mention hemostatic agents such as surgicel and merocel; plates that prevent intra-tympanic adherences such as silastic, and supporting substances such as absorbable sponges. As to the latter, gelfoam was introduced in 1960 with the role of providing graft support. It works as a real blanket to ensure stable support basis to the graft, up to the moment that epithelialization forces migration from the borders of the tympanic remains, which finally seals the perforations. Based on this first experience, the list of indications for this type of material in ear surgery rapidly expanded. Thus, bovine collagen has gradually become a type of "fits-all" material for temporal bone procedures. Today, in addition to its original supporting function, it may be used in small cubic shapes or trails in the external auditory canal or in open cavities of tympanomastoidectomy (supporting the stability of the graft and the repositioning of the tympanic-meatal flap); as hemostatic agent, in the obstruction of the auditory tube in tympanoplasty; as sealing agent in stapedectomies and fistulae of the oval and round window, in micro-vascular decompressions, among other applications.
At the same time indications expanded, other collagen compounds were produced and made available for ear surgery. Today in our country, in addition to Gelfoam, we also have at least two other analogous materials: Lyostyp and Ethicon. The three of them are used as absorbable sponges that after wetted, have a jelly presentation that is being fundamentally used as support-basis for transoperative grafts and flaps in ear surgeries. This type of use is only possible because of a common characteristic to all of them, that is, complete dissolution through the postoperative period.
In the literature review we found some terms that were used to describe the disappearance of the sponges, such as absorption, degradation and dissolution. We should try to understand them concerning the medical science. Absorption is a function in which specific substances penetrate in the cells by simple diffusion by action of electrical potential or pulled by solvent, whereas degradation is the disappearance of cytoplasmatic granules (lysosome) of a phagocytic cell when the granules fuse and empty the content in a phagosome; and, finally, dissolution is the act of becoming a solution, disassemble, dilute, disaggregate or melt.
Information obtained from the Brazilian distributor of these products reported that the sponges are completely absorbed when implemented in tissues, without causing excessive formation of scarring tissue, and if applied to hemorrhagic areas of the vaginal, rectal, nasal or skin mucosa, they are liquefied.
Based on the literature review, we noticed that few studies critically discussed the use of these compounds by otologists, and to our knowledge, none compared the specific dissolution indexes.
This characteristic, apparently irrelevant at first, seems to be essential for planning the many ear surgeries, obtaining maximum performance of tympanoplasty and open tympanomastoidectomy. Therefore, we have observed in the postoperative period of open cavities that especially in young adults the pace of epithelialization is very accelerated. In such circumstances, the presence of a slow dissolution collagen dressing provides formation of a thin film of fibrin, which in turn serves as a support and path for epithelial migration, that is, favoring epithelialization. The final result of this series of event is, not rarely, the formation of occult dead-end cavities. Possible niches of keratinized stratified squamous epithelium can be closed in mastoid compartments that have the potential to generate new cholesteatomas. They can grow silently for months in a shallow cavity, well epithelialized and theoretically safely, only to be clinically interrupted later by otorrhea or major complications (labyrinthine fistula, facial palsy).
Conversely, longevity of the collagen structure can be an important ally in maintaining a support to a long term graft in temporary obstruction of post-tympanoplasty auditory tube or even in closing small openings of the labyrinth (fistula, stapedectomy).
Thus, the work conducted by us aimed at developing in vitro experiment to analyze the possible differences in rates of dissolution of three collagen compounds normally and indistinctively employed in ear surgery. To that end, we tested the different compounds in two situations that tried to mimic the use in ear surgery: closed system (support of tympanoplasty or stapedectomy) and open system (filling of one cavity).
Upon analyzing the control group that used sterile solution and the tested group that used total blood, we observed there was no statistically significant difference between dissolution times of different brands, showing that at least in vitro, there is no biochemical action of blood in dissolving the sponges. Hämäläinen et al. (1998) reported that the physical-chemical and drugs effects over the sponges are not know, but he stated that they are soluble in water.
When we compared open and closed systems, we noticed that the samples of the open system had a reduction in the faster area, reaching 50% of its initial size within 48hours, whereas in closed plates, the samples reached their size only within 72 hours. This difference was expected, since the open system was more prone to evaporation than the closed one, a fact that makes the system less stable.
In closed plates, Ethicon has slower absorption, Gelfoam has intermediate profile and Lyostyp is the fastest one. We found statistically significant difference between Gelfoam and Lyostyp and between Ethicon and Lyostyp (p < 0.05), but there was no difference between Ethicon and Gelfoam (p > 0.05). Thus, Gelfoam and Ethicon are significantly slowed than Lyostyp, but they are not different one from the other.
In open plates, Gelfoam kept an intermediate profile, but there was an inversion between Lyostyp and Ethicon. In this system, the difference between the three brands did not present any significance (p>0.05). However, upon analyzing Figure 6, we can see a tendency to stabilization of degradation after 336 hours with Ethicon and Gelfoam, whereas Lyostyp tends to accelerate it, which would lead to a similar profile to that of the closed system, in case it was observed for longer time.
When we histologically analyzed the three samples (Figure 8, 9 and 10), we could notice that Lyostyp had a macromolecular structure that was more disorganized than in the other two brands, thus, probably less stable. The structure could have influenced its porosity.
In closed systems in which there is liquid condensation of the reabsorbed liquid in vitro, the instability of Lyostyp could lead to quick dissolution, being that the higher the amount of liquid, the quicker the process of sponge dissolution.
CONCLUSION
Based on the trends detected by the present study, Gelfoam and Ethicon can be preferably indicated to be used in tympanoplasty and stapedectomy because they play the role of support for longer time, but Lyostyp can be indicated to be used in cavities, which require quicker disappearance of the blanket structure.
Taking into account that Gelfoam presented an intermediate profile, both in the open and closed systems, we recommend its use as a regular routine for the different surgical techniques, since the exchange of material for each distinct procedure would lead to unnecessary work in the surgical room.
ACKNOWLEDGEMENTS
We would like to thank the Service of Otorhinolaryngology, Hospital de Clínicas de Porto Alegre, for having allowed us to use its facility to conduct the present project.
To Prof Luíse Meurer, Service of Pathology, HCPA, for her interest and constant collaboration.
To the Research and Post-Graduation Group, Hospital de Clínicas de Porto Alegre (GPPG-HCPA) for its technical support.
To Fundo de Incentivo à Pesquisa e Eventos (FIPE) for having provided financial support.
To the Blood Bank, HCPA for the attention and donation of blood to our experiment.
To Manhattan Eye and Ear Infirmary for having donated Gelfoam.
To product distributor Bbraun for having supplied us with Lyostyp.
REFERENCES
1. Champe PC, Harvey RA. Bioquímica Ilustrada. 2ª Edição. Editora Artes Médicas; 1996.
2. Correll JT, Princentice HR, Wise EC. Biologic Investigation of a New Absorbable Sponge. Surg Gynec And Obst 1945; 82: 585.
3. Costa SS, Dornelles C, Carvalhal LHSK. Manual de Condutas Pré, Trans e Pós-Operatórias; 2000. 128 p.
4. Cotran RS, Kumar V, Robbins SL. Pathologic Basis of Disease. 6th edition. W. B. Saunders; 1997.
5. Cruz OLM, Costa SS. Otologia Clínica e Cirúrgica. RJ: Ed Revinter; 1999. 317 p.
6. Davis H, Walsh TE. The limits of improvement of hearing following the fenestration operation. Laryngoscope 1950; 60: 273.
7. Hämäläinen KM, Määttä E, Piirainen H, Sarkola M, Väisänen A, Tanta V, Urtti A. Roles of acid/base nature and molecular weight in drug release from matrices of gelfoam and monoisopropyl ester of poly (vinyl methyl ether-maleic anhydride). Journal of Controlled Release 1998; 56: 273-83.
8. Okuyama K, Okuyama, Arnott S, Takayanagi M, Kakudo M. J Mol Biol 1981; 152:427.
9. Scheehy JL, Perkins JH. Stapedectomy: Gelfoam compared with tissue grafts. Laryngoscope 1975: 436.
10. Shambaugh GE, Glasscock ME. Tympanoplasty. In Surgery of the ear. 3rd ed. Philadelphia: WB Saunders; 1980.
11. Sourdille M. New techniques in the surgical treatment of severe and progressive deafness from otosclerosis. Bull New York Acad Med 1937; 13: 673-91.
12. Stryer L. Bioquímica. 4ª Edição. Editora Guanabara; 1996.
13. Wullstein H. Funktiolle Operationem in Mittelohr mit Hilfe des freien Spaltlappen-Transplantates. Arch Ohr Nas Kehlkopfheilk 1952; 161:422.
14. Zöllner F. The Principle of plastic surgery of the sound-conduction apparatus. J Laryngol Otol 1955; 69:637.
1 Biologist, Centro de Otite Média do Brasil, Hospital de Clínicas de Porto Alegre, Department of Ophthalmology and Otorhinolaryngology,
Federal University of Rio Grande do Sul. Master studies under course, Program of Post-Graduation in Pediatric Medicine, UFRGS.
2 Joint Professor, Department of Ophthalmology and Otorhinolaryngology, Federal University of Rio Grande do Sul.
3 Physician.
4 Physician.
Centro de Otite Média do Brasil - ComBr
Service of Otorhinolaryngology, Hospital de Clínicas de Porto Alegre - HCPA
Department of Ophthalmology and Otorhinolaryngology - UFRGS
Address correspondence to: Cristina Dornelles
Rua Cangussu, 1343 - Porto Alegre - RS - 90830-010 - (55 51) 32492275 - cristinadornelles@hotmail.com
Presented at 36º Congresso Brasileiro de Otorrinolaringologia - Florianópolis - SC - 2002.
Article submitted on August 11, 2003. Article accepted on October 30, 2003.