Year: 2003 Vol. 69 Ed. 5 - (17º)
Relato de Caso
Pages: 709 to 713
Subglottic stenosis as a clinical manifestation of Wegener's granulomatosis in adolescents: report of a case and review of literature
Author(s):
Márcia C. Machado1,
Erich C. M. de Melo2,
Paula M. de Sá1,
Danielle A. da Silva1,
Antônio Rafael G. Jr.1,
Osiris de O. C. do Brasil3
Keywords: Wegener's granulomatosis, larynx, subglottic stenosis
Abstract:
Wegener's Granulomatosis is a well-characterized systemic vasculitis and necrotising granulomatous inflammation of the upper, lower respiratory tracts and the kidneys. The initial manifestations of the disease usually occur in patients over than twenty years old. The otolaryngologic symptoms like rhinorrhea, recurrent sinusitis and epistaxis are commonly present in early course of the disease. It seems that subglottic stenosis is correlated to Wegener's granumatosis in adolescents. We describe a case of a patient that developed subglottic stenosis associated with Wegener's granulomatosis in childhood during the course of the disease.
![]()
INTRODUCTION
Wegener's granulomatosis is characterized by systemic vasculitis and necrotizing granulomatous inflammation of unknown etiology, which classically affects the upper respiratory tract, lungs and kidneys. The age range of highest incidence ranges from 25 to 50 years, mean age of manifestation in the 4th decade of life 1. In fact, 85% of the initial clinical manifestations occur in people older than 20 years, and the disease is rare in childhood, whose incidence is 6 to 14% 2, 3. Clinical forms can vary from localized to multi-systemic affection. Criteria to define the disease include nasal or oral impairment; characteristic radiological abnormalities, microhematuria or blood cylinders in the urine test, and compatible histology abnormalities with granulomatous inflammation of the arterial or perivascular wall. The presence of at least two criteria referred above allows sensitivity and specificity over 88% in the diagnosis of Wegener's granulomatosis 4. Laboratory tests have been used in the evolution of the pathology. Among the complementary tests, anti-cytoplasm antibody (cANCA) has been attributed to the activity of the disease, being present in 90% of the clinical cases 5, 6. Clinical treatment protocols include the use of glucocorticoids and/or immunosuppressors such as cyclophosphamide, allowing satisfactory rates of disease remission 1, 3, 5, 7, 8.
ENT manifestations have high prevalence, both in initial clinical manifestations and as part of the habitual disease course. Nasopharyngeal and laryngeal symptoms can be present in 73% of the cases 3. Rhinitis resistant to habitual medication treatment is present in 65% of the initial steps of Wegener's granulomatosis 1. Labovics et al.3 reported sinusal pathology in 85% of the patients. Other manifestations include repetitive acute otitis media, oral ulcers, epistaxis, dyspnea and hearing loss secondary to secretory otitis media.
Laryngeal obstruction is more frequent as late complication of the disease 1, 3, 5, 9, 10, however, isolated laryngotracheal forms were previously described 7, 11. The incidence of laryngeal stenosis by Wegener's granulomatosis ranges from 2% to 16% 1, 3, 5, 12. Juvenile presentations of Wegener's granulomatosis are not common. A longitudinal study comparing frequency of subglottic stenosis in two groups divided by age range concluded that the patients with Wegener's granulomatosis aged below 20 years presented 5-fold increased risk of having complications 3. The advocated clinical treatment, when started early, seems to reduce the risk of the condition, which is many times fatal 7. The differential diagnosis of subglottic stenosis can be difficult, and other pathologies should be ruled out, such as stenosis post-tracheal intubation, tuberculosis, syphilis, sarcoidosis, amyloidosis, recurrent polychondritis, Stewart's granuloma and neoplasias. 13
CASE REPORT
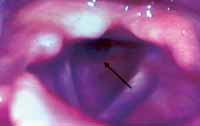
S.S.S., 15-year-old female patient, was admitted to the Service of Otorhinolaryngology/Head and Neck Surgery, Hospital do Servidor Público do Estado de Sao Paulo, in September 1998 with history of progressive dyspnea for the past four months, which had evolved to dyspnea at any physical stress, laryngeal stridor and hoarseness. We conducted a tracheotomy upon admission owing to the manifestations of acute respiratory failure. Upon examining the larynx, using indirect videolaryngoscopy, we observed that the laryngeal lumen was 80% obstructed by tissue located in the subglottis, concentric and or erythematous and friable appearance (Figure 1). Imaging studies showed absence of distal affection of the respiratory tract, and the pathology was restricted to the level of the 5th cervical vertebra.
Medical history revealed she had consecutive hospitalizations for the previous 3 years because of unspecific systemic vasculitis. The clinical picture was first detected in December 1995 as symmetrical polyarthritis of small and large joints, purpura lesions on the sole of the feet, hand palms and earlobes on the left, whose biopsy revealed the diagnosis of leukocytoclastic vasculitis. The hypothesis of juvenile rheumatoid arthritis was made, medication treatment was initiated during exacerbation episodes with glucocorticoids at high dosage and methotrexate. Recurrence of the acute episodes occurred as they attempted to progressively reduce the glucocorticoid dosage. She progressed to renal chronic failure within one year, whose renal biopsy was compatible with diffuse glomeruloslerosis. The first ENT manifestations were sneezing, nasal pruritus, coriza, nasal obstruction and epistaxis as of March 1998. There was no improvement of the clinical symptoms with the treatment with topical glucocorticoids, in view of the suspicion of allergic rhinitis. Repetitive sinusal pathology, resistant to habitual treatment, was present throughout the course of the disease. The patient also manifested epiglottitis in August 1998.
The biopsy of multiple fragments of the subglottis lesion revealed granulation tissue with absence of vasculitis and granulomas. Owing to the affection of the upper respiratory tract, other diagnostic hypotheses were made, especially of Wegener's granulomatosis. An empirical treatment with glucocorticoid and cyclophosphamide started and led to general clinical improvement and substantial and progressive reduction of subglottic narrowing in the subsequent months. Laboratory tests showed leukocytosis with neutrophilia, elevation of hemosedimentation rate, rheumatoid factor, alpha-1 glucoprotein and C reactive protein (CRP). Thorax x-rays were normal. The values of anti-cytoplasm antibody (cANCA) and anti-nuclear factor were within the normal range. Hematuria could be observed in the urine analysis. Later, a biopsy of the paranasal sinuses, from fragments of the right maxillary sinus mucosa, was conducted using endoscopic access whose clinical pathology result was compatible with the typical findings of Wegener's granulomatosis.
After one year of treatment, during the attempt to progressively reduce the medications in use, the patient presented recurrence of laryngeal stenosis and we conducted manual dilation, with no clinical complications. Glucocorticoids and cyclophosphamide at doses for active disease were reintroduced. We decided to maintain the tracheotomy with metallic canulla up to complete remission of the acute phase of the underlying disease. Since then, in the videolaryngoscopic exams, she has presented only 10% residual narrowing of the posterior laryngeal subglottic inferior wall (Figure 2). The remission of the disease activity was reached with clinical treatment. In March 2000 we removed and closed the tracheotomy.
Figure 1. Indirect videolaryngoscopy through rigid larynx telescope at 70º, in hospital admission of the patient, evidencing subglottic stenosis. Point orifice indicated by the arrow.
Figure 2. Retrograde view of the larynx obtained with the introduction of the flexible nasofibroscope of 3.2 mm through the metallic canulla of the tracheotomy after clinical treatment. Inferior borders of the vocal folds are free from impairment. Residual stenosis below 10% in the posterior subglottic wall indicated by the arrows.
DISCUSSION
Patients in the initial phases of Wegener's granulomatosis report, most of the times, symptoms of the upper respiratory tract. Rhinitis, sinusitis, otitis and epistaxis are initial manifestations of the disease in 75% of the cases14. Fauci et al.1 reported the impairment of the paranasal sinuses in 91% of the cases. Dyspnea was present in 7% of the patients as initial symptom of the disease. Seventeen in 108 patients with Wegener's granulomatosis presented subglottic or tracheal stenosis during some period of the disease 15. Similar incidence in percentage was found by another study with 158 patients 3.
The diversity of clinical presentations of the disease contributed to the difficulties in diagnostic confirmations. In the present case report, differently from the classical presentation, joint and dermatological manifestations represented the initial clinical picture. The interval between initial symptoms of the disease and development of ENT pathology was of 40 months. Arthralgia as initial manifestation of Wegener's granulomatosis occurs in 38% f the cases, being that arthritis is responsible for 28% 1. During the course of the disease, up to 70% of the patients will present some articular impairment in the form of symmetrical polyarthralgia of large or small joints, with out without arthritis,. Carrigton et al.2 reported that in 16 patients with Wegener's granulomatosis only one presented arthritis. Dermatological manifestations include papules, purpura, blisters, ulcers, and subcutaneous nodules as previously described 16. Studies revealed the incidence of 2% to 15% of dermatological forms as initial signs of the disease 1, 9.
Laryngeal obstruction can clinically present as hoarseness, progressive dyspnea, laryngeal stridor and, in severe cases, acute respiratory failure. The early diagnosis prevents severe complications in most cases. The incidence of laryngeal impairment in Wegener's granulomatosis ranges from 2% to 16% 1, 3, 5, 9. It is observed that subglottic stenosis is frequently associated with pulmonary pathology. Fauci et al.1 reported that 7% of subglottic stenosis in 85 patients with Wegener's granulomatosis being that all of them presented pneumopathology associated with the laryngeal manifestation. Four in 17 patients with laryngeal obstruction presented pulmonary impairment 9. We observed disagreement with the literature data since our patient presented a report of disease followed up for 6.5 years, but had had no pulmonary impairment symptoms.
Initial clinical presentations of Wegener's granulomatosis are uncommon in childhood and adolescence. Few studies reported subglottic stenosis in children and adolescents as clinical manifestations of the disease. Hellmann et al.7 concluded that isolated laryngeal affection in Wegener's granulomatosis was detected in younger age ranges than multisystemic cases. It is difficult to determine whether there is a correlation between the juvenile forms of the disease and subglottic stenosis. Lebovics et al.3 stated that in patients with initial presentations of Wegener's granulomatosis below the age of 20 years they have a 5-fold significant higher risk of developing subglottic stenosis compared to the group aged older than 20 years. McDonald et al.9 reported three patients with laryngeal obstruction and ages below 9 years in 17 patients with the disease. At the age of 12 years, our patient started presenting the manifestations of Wegener's granulomatosis in an early age range. Tracheotomy was required owing to acute respiratory failure. The period of decanullation was of 1.8 years. We decided to maintain the pervious airways using the metallic canulla up to complete remission and control of the underlying disease, since she presented an episode of recurrence in the first year after the tracheotomy, and later manual dilation of the stenotic segment was performed. Since then, she has not presented obstructive symptoms up to present. The duration of decanullation, according to the literature, varies a lot and depends on the control of Wegener's granulomatosis by clinical treatment. Other therapeutic modalities are used if there is no regression of stenosis with clinical treatment 3. Manual dilation is a simple procedure to be performed and leads to satisfactory results.
The diagnosis of subglottic stenosis in Wegener's granulomatosis is made by visualization of concentric laryngeal lumen narrowing, diffuse or restricted to the posterior wall, localized and limiting the subglottis with no significant distal extension. The mucosa infiltrate has erythematous aspect. Ulcerations are not uncommon. The biopsy of laryngeal tissue, differently from samples of suspected pulmonary tissue, rarely confirms the diagnosis of Wegener's granulomatosis 5, 7, 9. Clinical pathology analyses reveal chronic inflammatory tissue in the cases, with absence of fundamental elements such as the presence of vasculitis and granulomas in the studied material 1, 5, 7, 9. The lungs are the sites that produce the highest amount of positive responses in the clinical pathological analyses 1.
The clinical treatment can sometimes be delayed owing to difficulty to confirm the diagnosis, be it because of absence of the classical clinical picture or of reliable complementary methods. In a review of the literature, Gans et al.17 stated that 50% of the performed biopsies are not conclusive. Van der Woude et al.18 concluded that the presence of cANCA is a specific marker of the disease in activity. Anti-cytoplasm antibodies are absent or at non-detectable levels in the localized forms of the disease, or when the clinical control is reached in the acute phase 6. The reduction of serum levels is considered a signal of control of the activity. cANCA can be present in patients with other pathologies such as microscopic polyarteritis, rheumatoid arthritis and systemic lupus erythematosus 19. In this case, the differential diagnosis should take into consideration the clinical picture, as well as other characteristic findings of the disease. In the case reported here, we did not detect antibodies type cANCA during the disease evolution, despite the systemic impairment, even in initial phases. The treatment with glucocorticoid in years that preceded the diagnostic confirmation may have caused a reduction in undetectable serum levels of cANCA. Hellman et al.7 suggested that the localized forms of Wegener's granulomatosis can progress to disseminate the disease when the treatment of the disease is made only with glucocorticoids; they also observed that when associated with immunosuppressors, such as cyclophosphamide, four out of eight patients presented improvement.
CLOSING REMARKS
Morbidity and mortality of Wegener's granulomatosis are related to presence of severe disease in the lower respiratory tract and rapidly progressive glomerulonephritis. Clinical treatment with immunosuppressors and corticoids increase the survival of these patients. Early diagnosis allows the definition of the appropriate therapy in initial steps of the disease, reducing the risk of severe complications such as subglottic stenosis.
There is correlation between the initial presentation of the juvenile disease and development of subglottic stenosis, be it an isolated manifestation or during the course of the pathology.
REFERENCES
1. Fauci AS, Haynes BF, Katz P, Wolff SM. Wegener´s Granulomatosis: Prospective Clinical and Therapeutic Experience With 85 Patients for 21 Years. Ann Intern Med 1983; 98:76-85.
2. Carrington CB, Liebow AA. Limited Forms of Angiitis and Granulomatosis of Wegener´s Type. Am J Med 1966; 41:497-527.
3. Lebovics RS, Hoffman GS, Leavitt RY, Kerr GS, Travis WD, Kammerer W, Hallahan C, Rottem M, Fauci AS. The Management of Subglottic Stenosis in Patients With Wegener´s Granulomatosis. Laryngoscope 1992; 102:1341-5.
4. Leavitt RY, Fauci AS, Bloch TA, et al. The American College of Rheumatology 1990 Criteria for The Classification of Wegener´s Granulomatosis. Artriths and Rheumatism 1990;33:1101-7.
5. Herridge MS, Pearson FG, Downey GP. Subglottic Stenosis Complicating Wegener´s Granulomatosis: Surgical Repair as a Viable Treatment Option. J Thorac Cardiovasc Surg 1996;111:961-6.
6. Savage COS, Jones S, Winearls CG, Marshall PD, Lockwood CM. Prospective Study of Radioimmunoassay for Antibodies Against Neutrophil Cytoplasm in Diagnosis of Systemic Vasculitis. Lancet 1987; i:1389-93.
7. Hellmann D, Laing T, Petri M, Jacobs D, Crumley R, Stulbarg M. Wegener´s Granulomatosis: Isolated Involvement of the Trachea and Larynx. Ann Reum Dis 1987; 46:628-31.
8. Reza MJ, Dornfield L, Goldberg LS, Bluestone P, Pearson CM. Wegener´s Granulomatosis: Long-Term Follow-up of Patients Treated With Cyclophosphamide. Arthritis Rheum 1975; 18:501-6.
9. McDonald TJ, Neel H B III, DeRemee RA. Wegener´s Granulomatosis of the Subglottis and The Upper Portion of The Trachea. Ann Otol Rhinol Laryngol 1982;91:588-92.
10. Okamura HO, Anzai T, Misawa T. Recurrent Wegener´s Granulomatosis With Subglottic Granulation. Fukushima J Med Sci 2000;46:25-30.
11. Talerman A, Wright D. Laryngeal Obstruction Due to Wegener´s Granulomatosis. Arch Otolaryngol 1972; 96:376-9.
12. Waxman J, Bose WJ. Laryngeal Manifestations of Wegener´s Granulomatosis: Case Reports and Review of The Lieterature. J Rheumatol 1986;13:408-11.
13. Hoare TJ, Rhys Evans PH. Antineutrophil Cytoplasmic Antibody Assay in Diagnosis of Recurrent Subglottic Stenosis. Lancet 1988; i:1360.
14. Hoffman GS, Kerr GS, Leavitt RY, et al. Wegener´s Granulomatosis: An Analysis of 158 Patients. Ann Intern Med 1992;116:488-498.
15. McDonald TJ. Nasal Manifestations of Wegener´s Granulomatosis. Laryngoscope 1974;84:2101-11.
16. Fauci AS, Wolff SM. Wegener´s Granulomatosis: Pathology and Review of The Literature. Medicine (Baltimore) 1973;52:535-61.
17. Gans R, Vries N de, Donker AJM, Goldschmeding R, Hoorntje SJ. Circulating Anti-neutrophil Cytoplasmic Autoantibodies in Subglottic Stenosis: a Useful Aid in Diagnosing Vasculitis in This Condition? Quarterly Journal of Medicine 1991;291:565-74.
18. Van der Woude FJ, Rasmussen N, Lobatto S, et al. Autoantibodiy against Neutrophils and Monocytes: Tool for Diagnosis and Marker of Disease Activity in Wegener´s Granulomatosis. Lancet 1985;i:425-9.
19. Freehally J, Wheeler DC, Walls J, Jones S, Lockwood CM, Savage COS. A Case of Microscopic Polyarteritis Associated With Anti-neutrophil Cytoplasmic Components in Systemic Vasculitides. Clin Nephrol 1987 (in press).
1 Resident Physician, Service of Otorhinolaryngology, Head and Neck Surgery, Hospital do Servidor Público do Estado de Sao Paulo.
2 Collaborating Physician, Division of Clinical Otorhinolaryngology, Hospital das Clínicas, Medical School, University of Sao Paulo.
3 Ph.D. in Medicine, Federal University of Sao Paulo - Escola Paulista de Medicina.
Affiliation: Service of Otorhinolaryngology, Head and Neck Surgery, Hospital do Servidor Público do Estado de Sao Paulo.
Address correspondence to: Márcia Costa Machado - Rua das Biobedas nº 39 apt. 43
Parque Imperial - Sao Paulo 04302-010
Tel (55 11) 5587-4638 / 9670-8206 - E-mail:macmachado@hotmail.com / macmacma@terra.com.br
Article submitted on September 17, 2002. Article accepted on December 12, 2002.