Year: 2003 Vol. 69 Ed. 5 - (6º)
Artigo Original
Pages: 622 to 627
A study of 26 cases of Paracoccidioidomycosis evaluated at the Oswaldo Cruz Foundation (FIOCRUZ) Otorhinolaryngology Service
Author(s):
Francisco X. Palheta-Neto1,
João S. Moreira2,
Ana C. da C. Martins3,
Fabrycia J. Cruz4,
Edwin R. Gomes5,
Angélica C. Pezzin-Palheta6
Keywords: Paracoccidioidomycosis, Paracoccidioides brasiliensis, mouth, nose, otorhinolaryngology, stomatology
Abstract:
Paracoccidioidomycosis (PCM) is an acute systemic mycosis caused by a dimorphous fungus, Paracoccidioides brasiliensis (Pb), whose appearance under the microscope is similar to a ship rudder's wheel. Cases of PCM are restricted to the American continent and the disease affects mostly male individuals, with no marked tendency to affect any race in particular. Clinical symptoms are varied. Objective: To carry out a thorough epidemiological analysis of 26 cases of PCM evaluated at the Oswaldo Cruz Foundation (FIOCRUZ) Otorhinolaryngology (ENT) Sector. Study design: Clinical retrospective. Material and Method: A retrospective study was carried out on 26 medical charts of patients with otorhinolaryngological manifestations of PCM who were attended to from October 1998 to September 2001. Aspects taken into account: sex, age, occupation, number of years of schooling, smoking and drinking habits, main complaints, parts of the body presenting most lesions, the presence of co-infection, complementary examinations done, prescribed treatment. Results: 23 patients (88.5%) were male and 3 (11,5%) were female, their ages ranging from 32 to 72. 11 patients (42.3%) were farm workers and 21 (80.8%) were heavy smokers and/or drinkers. The most affected parts were the epiglottis and the lateral nasal wall. Sulphonamide derivatives were used to treat 14 patients (53.9%) and imidazoles were used for 12 cases (46.1%). Discussion: Pulmonary lesions may be mistaken for tuberculosis due to clinical and radiological similarities. Malnutrition may lead to clinical conditions of extreme gravity. Conclusion: The detailed medical histories of PCM carriers reveal important aspects such us the patients' origins and personal habits. Interdisciplinary actions, especially involving doctors and dentists, contribute to an early diagnosis and adequate treatment and follow-up of patients.
![]()
Introduction
Paracoccidioidomycosis (PCM) is a systemic deep mycosis caused by the dimorphous fungus known for causing primary disease in men, presenting a microscopic aspect similar to a ship rudder's wheel, Paracoccidioides brasiliensis (Pb)1-4. Its period of incubation can last from 15 days to 40 years 4. It presents varied symptoms: moriform stomatitis of Aguiar-Pupo, South-American blastomycosis, and Lutz-Splendore-Almeida mycosis1,3.
PCM is more frequently present in male rural workers, between the 4th and 5th decades of life, especially those that chew or clean dental interstitial cavities with small vegetal fragments 1, 2, 5, 6. Oliveira et al. (1997)3 reported greater incidence between the 4th and 7th decades of life. Construction workers also represent a frequently affected occupational group5. There can be dissemination of the disease to many organs and system, determining secondary lesions of mucosa, lymph nodes, skin and adrenal glands 2, 5.
The high incidence of PCM in Brazil, added to the severity of the clinical picture in some cases, would justify the academic interest for such topic. This is the rationale for our present study, in which we report a series of 26 patients seen in the Service of Infectology in Otorhinolaryngology at FIOCRUZ, addressing the different aspects of the disease.
Literature Review
PCM was initially described by Adolfo Lutz, in 1908, in two patients hospitalized at Santa Casa de Misericórdia de Sao Paulo. Alfonso Splendore, in 1912, was responsible for the isolation of Pb, and Floriano Paulo de Almeida for the description of this new genus 1-3,6-9.
All races seem to be equally susceptible to the disease, occurring about nine times more in men than in women 6. This fact is attributed to women's dedication to home chores, whereas men are out in the field and in contact with the soil. Another justification would be female hormone protection preventing the progression of the infection to the disease, inhibiting or hindering the adaptation of Pb to the host body 3, 4. These aspects would justify the reason why there are no gender preferences among the rare cases of PCM in children 6.
PCM has geographic distribution restricted to the American continent, endemic in some areas of South America, in which it is estimated to have 10 million infected people. In Brazil, there is incidence of the disease in the states of Sao Paulo, Minas Gerais, Rio de Janeiro, Paraná, Goiás, Santa Catarina and Rio Grande do Sul2,5,10.
Factors such as latitude, altitude, weather, geological structure, type of soil and raining rates are important elements for the confinement of the disease. It is known that Pb inhabits regions with high humidity and abundant vegetation, warm temperatures and high rain levels 3, 8.
No inter-human distribution of PCM has been confirmed, admitting that the infection occurs after accidental exposure to Pb 8. Franco (1987)11 defended two probable routes of contamination: inhalation route - primary lesion would be pulmonary, associated with lymphadenopathy 1; or, tegumentary route, through trauma or preexisting continuum solution of the oral cavity, such as aphthous ulcers, periodontal disease and deep tooth decay processes.
Similarly to deep mycosis, it has a number of clinical manifestations, as a result of the penetration of Pb into the host. The anamnesis reveals the origin and habits of the patients, who normally report abundant salivation, painful sensation upon swallowing, hoarseness and breathlessness. There is also general status impairment, translated into nonspecific symptoms: anemia, weakness, weight loss, headache, lack of appetite and fever 5, 7, 8.
Clinically, it presents a juvenile form (acute or sub-acute) that affects young subjects, with a quick course and presenting marked involvement of the reticular-endothelial system, representing 3% to 5% of the cases; and the adult or chronic form, which is localized and normally affects the lungs and respiratory tract 3, 6, 8, 9, 12.
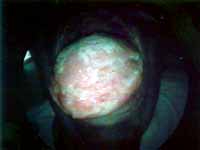
There are cutaneous-mucosa lesions, regional lymph nodes and tendency to lymphatic and/or hematogenic dissemination, which is sometimes fatal in the absence of early and appropriate therapy 1-3, 6, 7, 12. Cutaneous-mucosal lesions are characterized by ulceration with granulous and reddish fundus, followed by characteristic hemorrhagic tracing, named moriform stomatitis (Photo 1). Nasal and oral mucosas are almost always affected 5 (Photos 2 and 3), being that the lips present diffuse tumefaction 2. There are laryngeal lesions, with destruction of epiglottis (Photo 4). Ulceral-hemorrhagic gingivitis, periodontitis, mobility and dental loss are frequent 2, 3 (Photo 5). Pulmonary lesions predominate in the medium and base thirds, with nodules, infiltration and fibrosis 7.
The diagnosis can be made through isolation of the fungus, serological tests and histopathology analysis. Thorax simple x-ray is also very useful.
The differential diagnosis is wide and important, being frequently mistaken by neoplastic lesions, such as in the case described by Lodi, in 198513, whose definite diagnosis of primary PCM of the larynx was determined only after the second biopsy, replacing the mistaken first diagnosis of carcinoma. The frequency in which the primary lesion is located in the oral cavity differs it from North-American blastomycosis (Gilchrist's disease), rarely observed in this region 2. We should include in the differential diagnosis tuberculosis, lupus erythematosus, sarcoidosis, syphilis, Wegener's granuloma, inguinal granuloma, actinomycosis and leishmaniosis 5.
Sulphonamide derivates, Amphotericin B and imidazole derivates such as Cetoconazole, Itraconazole and Fluconazole are described to yield good therapeutic results, considering good tolerability, fewer side effects and easy administration, allowing increase in survival of affected patients, since in the past the natural course of the disease was death 10, 12.
Material and Method
We retrospectively studied the medical charts of 26 patients with confirmed diagnosis of PCM seem by the Service of Otorhinolaryngology, FIOCRUZ, in the period between October 1998 and September 2001. All patients were submitted to serology, mycological and histopathology analyses after incision biopsy. We analyzed gender, age, occupation, level of education, whether they were alcohol users and/or smokers, symptomatology, lesion site, presence of co-infection, complementary tests and management.
The references used to conduct the present study were collected from a survey at the website www.bireme.br on the internet and direct search in the annals of the II Congress of Sociedade de Otorrinolaringologia do Rio de Janeiro (Otorhinolaryngology Society of Rio de Janeiro)- Cariocão ORL 2002.
Photo 1. Moriform stomatitis in the palate.
Photo 2. Septal affection of the left nasal fossa.
Photo 3. Paracoccidioidomycosis lesion in the tongue.
Photo 4. Laryngeal lesion with destruction of the epiglottis.
Photo 5. Teeth and gum abnormalities.
Results
Out of 26 studied cases, 23 (88.5%) were male and only three (11.5%) were female subjects. The minimum age of patients was 32 years and the maximum was 72 years, being the 5th and 6th decades of life the most affected ones, respectively, in 11 patients (42.3%) and 9 patients (34.7%) (Graph 1).
A total of 11 cases (42.3%) reported agriculture-related occupation (Graph 2).
As to education level, only one of them had complete college level. Conversely, 15 (57.8%) had not finished elementary school (Graph 3).
The main sites of lesions were epiglottis and nasal lateral wall in 38.5% of the cases, lips, vocal folds and nasal septum in 34.7%. Seven cases (26.9%) had associated lung affections (Table 1).
Dysphonia, weight loss, dyspnea, dysphagia and nasal obstruction were the main reported complaints (Table 2).
As to complementary tests, we had positive responses in 21 cases (80.8%) in biopsy, 15 (57.8%) in serology tests and 9 (34.7%) in mycological analyses (Graph 4).
Out of the assessed patients, 16 (61.1%) were smokers and alcohol users, five (19.3%) were only smokers and four of them (15.3%) did not have any addictions. Only one patient was only a heavy drinker, without smoking (Graph 5).
Some patients presented co-infection: five (19.3%) cases of tuberculosis, two (7.7%) of Hansen's disease, one case of syphilis and one of gonorrhea. Cases of associated neoplasm were diagnosed in three patients (11.5%) affecting the tongue, larynx and upper lip.
Sulphonamide derivates (sulphametoxazole-thrimetropin) were used in the treatment of 14 (53.9%) patients, whereas 12 (46.1%) patients used imidazole derivates (fluconazole in 11 patients and cetoconazole in one case). Amphotericin B was not used in any case.
Graph 1. Distribution of cases by age range.
Graph 2. Type of occupation of the patients.
Graph 3. Level of education of patients.
Graph 4. Results of complementary tests.
Graph 5. Distribution of patients concerning smoking and alcohol abuse.
Table 1. Most frequent lesion sites.
Site / % of cases
Epiglottis - 38.5%
Lateral nasal wall - 38.5%
Lips - 34.7%
Vocal folds - 34.7%
Nasal septum - 34.7%
Palate - 26.9%
Lungs - 26.9%
Gingival region - 23.1%
Internal aspect of the cheeks - 23.1%
Tongue - 19.3%
Arytenoid - 15.4%
Uvula - 11.6%
Tonsil - 7.7%
Table 2. Main reported complaints.
Main complaints / % of cases
Dysphonia - 30.8%
Weight loss - 30.8%
Dyspnea - 19.3%
Dysphagia - 19.3%
Nasal obstruction - 19.3%
Cough - 15.4%
Sialorrhea - 15.4%
Odynophagia - 15.4%
Fever - 7.7%
DISCUSSION
Agreeing with the literature, we observed that male patients were more affected, in an approximate proportion of eight men to one woman, which represented results quite identical to that reported by Hassessian et al., in 20006, who reported a proportion of 9:1.
The affected age ranges among our patients were 5th and 6th decades of life, according to what was proposed by Oliveira et al. (1997)3.
As to occupation, 11 (42.3%) of the patients referred activities related to agriculture and three (11.5%) were construction workers, confirming what was proposed by Botelho and Campos (1989)1, Bisinelli et al. (1998)2, Pagliari et al. (1995)5 and Hassessian et al. (2000)6. Unfortunately, it was not possible to assess our patients concerning the habit of chewing vegetation and picking the teeth with small tree branches.
Pulmonary lesions are frequent in PCM and when they occur in chronic disease, they can be mistaken by tuberculosis owing to the clinical and radiological similarities of the disease 3. In our study, we observed pulmonary involvement in seven cases (26.9%). We agreed with Pagliari et al. (1995)5 about the affection of the nasal and oral mucosa.
The low educational level observed, in which 16 out of 26 patients were illiterate or had incomplete elementary education, markedly evidenced the social-economic and cultural differences. The lack or poor access to general, prophylactic and therapeutic information about this and other diseases, and the difficulty to access medical care were reported by the patients. Only one patient had complete college level.
No clinical observation was different from what had been reported in the literature. Malnutrition and reduction of immune defenses of the body that can result from alcohol intake make alcohol abuse a predisposing factor 3. Seventeen of the 26 patients in the study were heavy alcohol drinkers.
CONCLUSION
It is extremely important to conduct thorough anamnesis and physical examination of the patients, involving different health professionals, especially physicians and dentists, aiming at collecting information about origin of patients, who may come from endemic regions, as well as to detect the existence of localized and systemic lesions.
REFERENCES
1. Botelho MR, Campos HR. Paracoccidioidomicose:uma doença sistêmica com repercussões bucais. Arq Bras Med Nav 1989; 50(3):59-63.
2. Bisinelli J, Marzola C, Ferreira MLS, Toledo Filho JL, Pastori CM, Zorzetto DLG. Manifestações estomatológicas da Paracoccidioidomicose (Paracoccidioide Brasiliensis ou Enfermidade de Lutz-Splendore-Almeida): considerações gerais e apresentação de casos. Rev Fac Odontol Bauru 1998; 6(1):1-11.
3. Oliveira PT, Yurgel LS, Lorandi CS, Moraes ACS. Estudo de 54 casos de paracoccidioidomicose diagnosticados no Serviço de Estomatologia do Hospital São Lucas da PUCRS. R Med PUCRS 1997; 7(4):161-6.
4. Padula DH. Paracoccidioidomicosis. Estudio sobre 284 pacientes en la provincia de Misiones. Rev Asoc Odontol Argent 1999; 87(3):251-3.
5. Pagliari AV, Arce GAT, Piazzetta CM. Aspectos clínicos das lesões de paracoccidioidomicose na mucosa bucal. DENS 1995; 11:41-8.
6. Hassessian A, Ishikawa EN, Alencar FI, Marcucci G. Estudo da prevalência de lesões bucais em pacientes portadores de paracoccidioidomicose na região de Campo Grande - Mato Grosso do Sul. RPG Rev Pós Grad 2000; 7(3):214-8.
7. Fernandes PD, Fernandes LT. Paracoccidioidomicose. Rev Bras Otorrinolaringol 1986; 52(4):23-5.
8. Souza KM, Paiva MCP, Rodrigues EM, Quintão EF, Passomani LFC. Paracoccidioidomicose de Laringe. Rev Soc Otorrinolaringol Rio de Janeiro 2002; 2(1):37-9.
9. Ronquillo TEF. Contribuição ao estudo da Paracoccidioidomicose na República do Equador. Rev Pat Trop 1983; 12(3):345-419.
10. Araújo MS, Sousa SCOM. Análise epidemiológica de pacientes acometidos com paracoccidioidomicose em região endêmica do estado de Minas Gerais. RPG Rev Pós Grad 2000; 7(1):22-6.
11. Franco M. Paracoccidioidomycosis: a recently proposed classification of its clinical forms. Rev Soc Bras Med Trop 1987; 20(2):129-132.
12. Sortino AMF, Guariglia CC, Stabenow E, Lopes JMA, Khouri Z, Paciullo VH. Paracoccidioidomicose: revisão bibliográfica e discussão da terapêutica através do relato de um caso tratado com fluconazol. Rev Med (São Paulo) 1998; 77(1):55-64.
13. Lodi M, Azevedo JPM, Kós AO, Portinho FS, Paes VMC, Procópio ES, Damasceno DF, Tognon N, Martins OM. Blastomicose de laringe. An Hosp Sider Nac 1985; 9(1):43-5.
1 Master in Otorhinolaryngology, Federal University of Rio de Janeiro -UFRJ. Substitute Professor of Otorhinolaryngology, Federal University of Pará -UFPA.
2 Full Researcher, Fundação Oswaldo Cruz - FIOCRUZ.
3 Master in Otorhinolaryngology, Federal University of Rio de Janeiro -UFRJ.
4 Resident physician in Otorhinolaryngology, University of Rio de Janeiro - UNI-RIO.
5 Resident physician in Otorhinolaryngology, University of Rio de Janeiro - UNI-RIO.
6 Master in Otorhinolaryngology, Federal University of Rio de Janeiro -UFRJ.
Affiliation: Fundação Oswaldo Cruz - FIOCRUZ/ Instituto de Pesquisas Clínicas Evandro Chagas/ Service of Otorhinolaryngology.
Address correspondence to: Francisco Xavier Palheta Neto - Avenida Gentil Bittencourt, 808 ap. 3001 - Nazaré Belém PA 66040-000
Tel (55 91) 212-0874/ 224-6517/ 9116-0508 - E-mail: franciscopalheta@hotmail.com
Article submitted on November 18, 2002. Article accepted on August 08, 2003.