Year: 2003 Vol. 69 Ed. 5 - (4º)
Artigo Original
Pages: 606 to 610
The use of expanded polytetrafluoroethylen by type I thyroplasty
Author(s):
Francisco Veríssimo de Mello-Filho1,
Lílian Ricz2,
Leonardo de S. Kruschewsky3
Keywords: vocal cord paralysis, thyroplasty, gore-tex, polytef, expanded polytetrafluoroethylene
Abstract:
The Unilateral Vocal Fold Paralysis (UVFP), abducted, is a medical pathology that gives a lot of discomfort to the patient especially because of the speech impairment. Nowadays it is offered a variety of scientific methods for its treatment. Aim: To study the efficacy, advantages and disadvantages in using expanded Polytetrafluoroethylene (e-PTFE)'s band to medialize a paralyzed and abducted vocal fold. Study Design: Longitudinal Cohort. Material and Methods: Four patients with medical-laryngoscope diagnosis of disphonia by UVFP, abducted for at least one year. They were submitted to speech pathology evaluation and so, to e-PTFE type one thyroplasty medialization and followed by videolaryngoscopy, computed tomography and speech pathology therapy. Results: All four patients were satisfied with the thyroplasty results, videolaryngoscopy was used to document the vocal fold medialized and its function was studied by speech pathologist. One patient had e-PTFE band extrusion during surgery, being submitted of another procedure six months after without complications. Conclusion: PTFE band is an efficient treatment for UVFP abducted without important risks.
![]()
Introduction and Objective
Vocal fold unilateral paralysis in abduction is an important cause of dysphonia and manifests varied clinical presentations, depending on how much it affects glottic closure. The more abducted the paralyzed vocal fold position, the greater the glottic incompetence and the more frequent the negative consequences for the phonation of the patient 1, 2.
The paralysis may originate from central or peripheral origin and can have different etiologies 2, 3. Central unilateral paralysis is resultant from tumors, vascular accidents and trauma. Peripheral unilateral paralysis is normally caused by iatrogenia resultant from cervical-thoracic surgery, cervical-thoracic neoplasm with recurrent laryngeal nerve and/or vagus nerve involvement, trauma or idiopathic origin.
Phonosurgery with techniques that promote medialization of the abducted paralyzed vocal fold has shown great advance in past years. We currently count on a considerable number of surgical options and materials that allow vocal fold medialization 4-13. Among the therapeutic options we can include endoscopic access 14, with injection of different types of materials in the vocal fold 2, 3, 6-10, or open cervical access, with performance of thyroplasty, modification of the laryngeal cartilaginous framework and rotation of the arytenoid 4, 5, 15-17.
Among them, type I thyroplasty has proved to be one of the best options for medialization of the vocal fold 15, 18, 19, however, what is still questionable is which material would be the best implant between the thyroid cartilage and the soft tissues in the glottic region. It is possible to use synthetic material such as silicone, teflon and PTFE tape 4-9, 14, 18-20, or biological material such as cartilage, muscle fascia or fat 1-4, 10-12, 21, 22, with the same purpose, being that the two last ones, together with teflon, are used for medialization by injection.
In order to check the efficiency, advantages and disadvantages of the use of PTFE-e tape in medialization of paralyzed vocal fold, we tested its use associated with type I thyroplasty advocated by Isshiki for the treatment of four patients with unilateral vocal fold paralysis in abduction.
Material And Method
Between July 2001 and April 2002, at HC-FMRP-USP, four patients with unilateral vocal fold paralysis were treated with type I thyroplasty and medialization of the vocal fold in abduction with the use of PTFE tape (6mm diameter by 50cm length).
We adopted the inclusion criteria as follows:
a) Diagnosis of unilateral vocal fold paralysis (UVFP) in abduction for over one year;
b) No previous treatment for medialization of the paralyzed vocal fold;
c) Preoperative voice therapy with no success in reaching the appropriate vocal compensation;
d) Informed consent term signed by the patient agreeing to undergo the proposed surgery under local anesthesia.
All patients were submitted to clinical, laboratory, speech and vocal assessments and videolaryngoscopy before the surgery.
After the surgery the patients underwent speech and voice therapy, videolaryngoscopic follow-up every two months and imaging analysis with computed tomography up to 6 months.
To analyze vocal quality, we recorded the voice of patients in cassette tapes by regular commercial brands using a Sony tape recorder, with a portable microphone coupled to the tape recorder, placed 10cm from the speakers' mouth, in an acoustic booth. We asked the patients to produce prolonged vowels /a/ /i/ and /u/, numbers from 1 to 30, and to sing "Happy Birthday". They were instructed to produce voice and speech at habitual intensity and frequency.
The samples were analyzed by speech and voice pathologists specialized in voice. They conducted an auditory perceptive assessment using the GRBAS scale, validated by Hirano, in 1981, which characterizes the grade of dysphonia (G-grade), scoring from 0 to 3, R-roughness, B-breathiness, A-asthenicity and S-strain, before and after the medialization of the paralyzed vocal fold using a PTFE-e tape. We applied the GRBAS scale with grades described as absence of dysphonia (0), mild affection (1), moderate (2) and severe impairment (3).
Patients
Patient 1: R. C. M. S., female, aged 16 years old, with tricuspid atresia, submitted to heart surgery to perform left atrium-pulmonary anastomosis. She presented left UVFP after the surgery.
Patient 2: J.R.L., male, aged 22 years old, victim of a stab on the left cervical region, which led to left UVFP.
Patient 3: J.R., male, aged 51 years old, with mesenchymal tumor, left carotid artery paraganglioma, operated in November 2000 and presenting left UVFP.
Patient 4: L.A.C., male, aged 48 years old, with vagus nerve trunk paraganglioma located at its onset, in the right jugular foramen, operated in February 2001; the vagus nerve was sectioned and the tumor segment was removed, leading to right UVFP.
Surgical technique
As to preoperative preparation, we used mild venous sedation administered by the anesthesiologist and topical anesthesia with lidocaine spray at 10%, sprayed in the nasal mucosa and oropharynx. In the cervical region, we injected lidocaine 2% with adrenalin 1/200,000U in the lower border of the thyroid cartilage on the affected side. Next, the nasofibroscope was introduced through the nose and positioned right above the larynx to provide good visibility of the vocal folds during the whole procedure.
The technique used was type I thyroplasty by Isshiki4,5,15. After detachment of the internal perichondrium of the thyroid cartilage we started the introduction of the PTFE-e tape through the opening of the window close to the thyroid cartilage. In a continuous fashion, the tape was progressively inserted and pushed the vocal fold to the medial position, under visualization provided by videolaryngofibroscopy. When the vocal fold reached the midline, we asked the patient to produce sounds to check vocal quality. At that time, together with the speech and voice therapist, we started to module the patient's voice by introducing anteriorly or posteriorly the PTFE-e tape, up to satisfactory phonation and appropriate three-dimensional positioning of the vocal fold.
Results
Vocal outcomes were excellent in the four patients. There were no manifestations of bleeding or dyspnea in the patients while they were hospitalized, allowing discharge on postoperative day one. There was no infection in the surgical wound, fever, granulomatous reaction or biological rejection to PTFE-e during the follow-up.
Patient 4 presented as complication the accidental rupture of the pyriform sinus during the placement of the PTFE-e tape in the first surgery, which was immediately identified and the procedure was interrupted. The patient progressed well with clinical treatment based on oral fasting, venous hydration for three days and antibiotic therapy followed by introduction of liquid diet, after negative blue methylene test four days later.
Six months after, the patient was once again submitted to the procedure of vocal fold medialization with PTFE-e without any complications and he presented the same level of satisfaction as the other patients.
The speech and voice and laryngoscopic findings are shown in Tables 1 and 2 comparing pre and postoperative results.
Laryngoscopy images with the patient producing phonation at maximum adduction of vocal folds are shown preoperatively (Figure 1) and postoperatively (Figure 2).
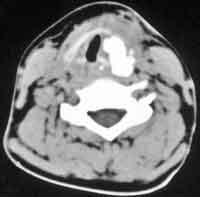
In Figure 3 we can see the laryngeal imaging study with computed tomography six months after vocal fold medialization with PTFE-e.Table 1. Description of the results obtained with the auditory perceptive analysis in patients treated with vocal fold medialization with Gore-Tex tape based on the GRBAS scale.
Table 2. Laryngology findings describing medialized vocal fold aspects, pre and postoperative.
Figure 1. Preoperative laryngoscopy, patient at maximum adduction.
Figure 2. Postoperative laryngoscopy, satisfactory glottic closure.
Figure 3. Postoperative computed tomography image showing Gore-Tex implant located in the paraglottic space, medializing the vocal fold.
Discussion
Even though it had been reported in a number of series 2, 8, 19, 23 unilateral vocal fold paralysis (UVFP) with idiopathic etiology was not found in our small sample, in which all the four cases presented clear etiological factors.
The diversity of etiologies for UVFP is quite surprising, even though in our study most of the cases resulted from surgical procedures.
We defined the minimum clinical follow-up period of 1 year to check absence of spontaneous restoration of vocal fold mobility 19. This period, however, can be shortened especially in clinical situations in which UVFP creates discomfort or anxiety to the patient. In such cases it is recommendable to conduct electromyography study of the larynx, but we should always bear in mind that medialization of the vocal fold with PTFE-e tape can be reverted at any time, which only requires removal of the implant.
The patients in this study had not been submitted to any type of procedure to medialize the vocal fold, or to any other additional measure besides the use of PTFE-e. We wanted to try to assess only the results obtained with the use of PTFE-e. It is possible to associate other measures such as substance injection in the vocal fold or rotation of the arytenoids to get good vocal adjustment, but such measures were not necessary in our cases.
Preoperative speech and voice therapy was applied as an attempt to have vocal compensation and also to assess the grade of dysphonia. Postoperatively, the speech and voice therapy contributed to promoting vocal adaptation and to assessing vocal quality.
The predominance of left vocal fold paralysis in our series is also repeated in other reports 23-25. It is possible that such fact is resultant from anatomical peculiarities of the recurrent laryngeal nerve on the left, but no studies have scientifically confirmed it.
The use of silicone blocks or cartilage to medialize the vocal fold has many inconveniences. They have to be molded and handled at the moment of the surgery 14, 15 to reach the ideal form, that is, a measure capable of fitting it in the thyroid cartilage window and produce complete medialization of the vocal fold, which is laborious and time consuming, extending the duration of the surgery.
The use of PTFE-e tape proved to be easy to handle especially by the characteristics of the tape malleability, making it easier and quicker 19. Even though it is possible to have good medialization of the vocal fold with a solid block of silicone, many times it is necessary to have lengthening, rectification of some deformity and leveling of the vocal fold, which is not possible with a silicone block. The PTFE-e tape allows micro adjustment to the vocal fold after applying a variable amount of the tape to the laryngeal compartment and manage to have medialization, which then requires fine adjustment of the anatomical position of the vocal folds under endoscopic vision and sound feedback by the patients' vocal production 15, 18-21. If there is vocal fold deformity, creating concavity, convexity or non-leveling, it is possible to introduce or extract small amounts of the tape in the anterior, medium or posterior region of the vocal fold, so as to reach symmetry and alignment. It is possible to lengthen the vocal fold by applying PTFE-e closer to the posterior commissure, pushing the arytenoid cartilage to the posterior region, a maneuver that is used in practically all patients; in one case (case 4), during the maneuver, we perforated the pyriform sinus with the emergence of the PTFE-e tape through the hypopharynx.
As to injectable substances to medialize the vocal fold, we can use biological substances such as fat, collagen or fascia, which are unpredictably absorbed by the body 2, 3, 14, 18, 21, 23, 24. Injectable synthetic substances such as teflon can migrate and it is practically impossible to remove them in face of a problem 6, 7, 18, 27, 28. Moreover, such substances can have the inconveniences of imprecise control of the injected amount.
In our opinion, the only disadvantage of the use of PTFE-e tape is to be associated with the cervical access to execute type I thyroplasty, since like all types of thyroplasty, the patient gets a neck scar, which would be avoided in the case of injecting technique.
In addition to the complication of accidental perforation of the pyriform sinus during manipulation of the paraglottic space, which is possible to happen with any substance used in type I thyroplasty, there were no other observed complications. Currently, all patients preset good and stable vocal quality, which encourages us to recommend the use of this method to treat UVFP.
Conclusion
We can conclude that PTFE-e tape proved to be a very satisfactory material for medialization of the vocal fold through the technique of type I thyroplasty, with the advantage of being easier and quicker in its manipulation, allowing better adjustment of the vocal fold with corresponding improvement in vocal quality and low rate of complications.
REFERENCES
1. Weber RS, Neumayer L, Alford B. Clinical restoration of voice function after loss of the vagus nerve. Head and Neck Surgery 1985; 7:448-57.
2. Hill DP, Meyers AD, Harris J. Autologous fat injection for vocal cord medialization in the canine larynx. Laryngoscope 1991; 101:344-8.
3. Lewy RB. Experience with vocal cord injection. Annals of Otology 1976; 85:440-50.
4. Isshiki NI, Morita H, Okamura H. Thyroplasty as a new phonosurgical technique. Acta Otolaryngology 1974; 78:451-7.
5. Isshiki NI, Okamura H, Ishikawa T. Thyroplasty tipe I for disphonia due to vocal cord paralysis or atrophy. Acta Otolaryngology 1975; 80:465-73.
6. Arnold GE. Alleviation of aphonia or dysphonia through the intracordal injection of teflon paste. Annals of Otology Rhinology & Laryngology 1963; 72:384-95.
7. Dedo HH, Urrea RD, Lawson L. Intracordal injection of teflon in the treatment of 135 patients with dysphonia. Annals of Otology Rhynology & Laryngology 1973; 82:661-7.
8. Rubin HJ. Pitfalls in treatment of dysphonias by intracordal injection of synthetics. Laryngoscope 1965; 75:1381-97.
9. Schramm VL, May M, Lavorato AS. Gelfoan paste injection for vocal fold paralysis: temporary rehabilitation of glottic incompetence. Laryngoscope 1978; 88:1258-73.
10. Ford CN, Bless DM. Clinical experience with injectable collagen for vocal fold augmentation. Laryngoscope 1986; 96:863-9.
11. Crumley RL. Update: Ansa cervicalis to recurrent laryngeal nerve anastomosis for unilateral paralysis. Laryngoscope 1991; 101:384-288.
12. Mikaelian DO, Lowry LD, Sataloff RT. Lipoinjection for unilateral vocal cord paralysis. Laryngoscope 1991; 101:465-8.
13. Brandenburg JH, Kirkham W, Koschkee D. Vocal cord augmentation with autologous fat. Laryngoscope 1992; 102:495-500.
14. Zaretsky LS, Shindo ML, Rice DH. Autologous fat injection for unilateral vocal fold paralysis. Ann Otol Rhynol Laryngol 1996; 105:602-6.
15. Isshiki N. Progress in laryngeal framework surgery. Acta Otolaryngol 2000; 120:120-7.
16. Kojima H, Hirano S, Isshiki N. Anatomic study for posterior medialization thyroplasty. Ann Otol Rhynol Laryngol 1999; 108:373-7.
17. Isshiki N, Tanabe M, Sawada M. Aryteniod adduction for unilateral vocal cord paralysis. Arch Otolaryngol 1978; 104:555-8.
18. Zeitels SM, Casiano RR, Gardner GM, Hogikyan ND, Koufman JA, Rosen CA. Management of common voice problems: Committee Report. Otolaryngology-Head and Neck Surgery 2002; 126:333-48.
19. Giovanni A, Vallicioni J.M, Grass R, Zanaret M. Clinical experience with Gore-Tex for vocal fold medialization. Laryngoscope 1999; 109:284-8.
20. McCulloch TM, Hoffman HT, Andrews BT, Karnel MP. Arytenoid adduction combined with Gore-Tex medialization thyroplasty. Laryngoscope 2000; 110:1306-11.
21. Ford CN. Advances and refinements in phonosurgery. Laryngoscope 1999; 109:1891-900.
22. Duke SG, Salomon J, Blalock D, Postma G.N, Koufman JA. Fascia augmentation of the vocal fold: Graft yield in the canine and preliminary clinical experience. Laryngoscope 2001; 111:759-64.
23. Brandenburg JH, Unger JM, Koschkee D. Vocal cord injection with autologous fat: A Long-Term Magnetic Ressonance Imaging Evolution. Laryngoscope 1996; 106:174-80.
24. Laccourreye O, Crevier-Buchman L, Le Pimpec-Barthes F, Garcia D, Riquet M, Brasnu D, Recovery of function after intracordal autologous fat injection for unilateral recurrent laryngeal nerve paralysis. The Journal of Laryngology and Otology 1998; 112:1082-4.
25. Abdel-Aziz MF, Gad El-Hak NA, Carding PN. Thyroplasty for functional rehabilitation of the incompetent larynx. The Journal of Laryngology and 1998; Otology 112:1172-5.
26. Saccogna PW, Werning JW, Setrakian S. Lipoinjection in the paralyzed freline vocal fold: a preliminary clinical study. Otolaryngology & Head & Neck Surgery 1997; 117:465-70.
27. Kasperbauer JL, Slavit DH, Maragos NE. Teflon granulomas and overinjection of teflon: a therapeutic challenge for the otorhinolaryngologist. Annals of Otology Rhinology & Laryngology 1993; 102:748-51.
28. Nakayama M, Ford CN, Bless DM. Teflon vocal fold augmentation: failures and management in 28 cases. Otolaryngology & Head & Neck Surgery 1993; 109:493-8.
1 Ph.D., Professor, Discipline of Head and Neck Surgery, Department of Ophthalmology, Otorhinolaryngology and Head and
Neck Surgery, Hospital das Clínicas, Medical School, University of Sao Paulo, Campus Ribeirão Preto.
2 Speech therapist, coordinator of the Division of Speech and Hearing Pathology, Hospital das Clínicas, Medical School, University of Sao Paulo, Campus Ribeirão Preto.
3 Hired physician, Discipline of Head and Neck Surgery, Department of Ophthalmology, Otorhinolaryngology and Head and Neck Surgery,
Hospital das Clínicas, Medical School, University of Sao Paulo, Campus Ribeirão Preto.
Address correspondence to: Francisco Veríssimo de Mello-Filho - Rua Salvador Delloiagono, 70 Jardim Canada Ribeirão Preto SP
Tel/Fax (55 16) 623-6169 / 602-2353 - E-mail:fdmfilho@yahoo.com
Article submitted on November 18, 2002. Article accepted on August 08, 2003.