Year: 2003 Vol. 69 Ed. 4 - (14º)
Artigo Original
Pages: 527 to 532
Osteoma of external acoustic meato: report of nine cases and literature review
Author(s):
José Ricardo G. Testa1,
Gilberto U. Pizarro2,
Isabela M. De Vuono3,
Maria Eugênia L. R. B.
Valeriano Neto3,
Fernando Barros4
Keywords: osteoma, meato, acoustic, external, hipoacusia
Abstract:
The osteoma of external acoustic meatus corresponds to an abnormal and benign bony growth, that is developed under the skin of the auditory canal and that can cause total or partial obstruction of the external acoustic meatus. Study design: Serie study. Material and method: We reported in this study nine cases of osteoma of external acoustic meatus. The patients' ages varied between 23 and 70 years old, being the average age 40,6 years. These patients were 5 of the feminine sex and 4 were of the masculine sex. Results: The more common symptoms were hipoacusia, caused by the partial or total obstruction of the canal, appealing external otitis and also the accumulation of cerumen deep in the external auditory canal with difficult removal. Conclusion: We recommended in the presented cases surgical treatment, which had good evolution, with no recidivism.
![]()
Introduction
The authors presented nine cases of external acoustic canal osteoma, which are considered slow growing benign neoplasm.
We conducted clinical otorhinolaryngologic examination, radiological imaging with computed tomography (CT scan) that showed dense and single images obstructing partially or completely the external acoustic canal. We also conducted audiometry tests that revealed hearing losses.
All patients were submitted to surgical treatment for the removal of the osteoma. Out of the nine patients operated on, three presented epithelial build-up such as obliterating external acoustic canal cholesteatoma, medially to the osteoma. In all patients, we proceeded with detachment of the epithelium over the osteoma to recover the area of insertion of the external acoustic canal. In one case, there was stenosis of the canal that required a second procedure with skin graft.
In all cases, we conducted clinical pathology analysis that confirmed the diagnosis. To present, there have been no recurrences of the osteomas.
Literature review and differential diagnosis
External acoustic canal (EAC) osteoma corresponds to an abnormal bone growth that is benign, which develops as a semi-spherical mass under the skin of the canal and can cause obstruction. The mass is hard and non-painful. Osteomas are sessile and solitary with a narrow basis that connects the osteoma to the EAC bone. Normally, they are fixed to tympanomastoid or tympanosquamous sutures. They are benign tumors but present progressive growth causing obstruction of the EAC. Upon causing obstruction, there is conductive hearing loss and also recurrent external otitis.
Osteoma of the external auditory canal is not a frequent lesion and it can occur at any age, being three more times common in male patients1.
As to diagnosis, it is made through the clinical history of the patient, clinical ENT examination and imaging techniques such as CT scan of the temporal bones. CT scan intends to enumerate and localize the calcifications of the walls, assessing the impairment of the EAC size, studying the depth of the osteoma and investigating the presence of associated pathologies, both to the EAC and the middle ear 2.
As differential diagnosis of the bone lesion of the external acoustic canal, we can include exostosis. Morrison in 1948 conducted the first clinical differentiation between osteoma and exostosis 3. Clinically speaking, exostosis is characterized as a bone elevation with widened basis, normally multiple and bilaterally, affecting the tympanic bone 1. Exostoses are the most frequently found tumors in the EAC. They are rare in childhood and more frequent in males. They present as etiological factor prolonged and repetitive exposure to cold and salty water in the EAC.
Clinical staging for osteoma was proposed by Graham in 1982: stage 1 - tumor visible to the examiner but asymptomatic to the patient; stage 2 - symptomatic but controlled with conservative treatment; stage 3 - symptomatic requiring surgical treatment 4.
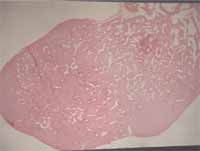
Histologically, osteoma of the EAC is recovered by squamous epithelium with subjacent periosteum. Internally, it presents sparse fibrovascular canals, surrounded by bone lamellae with few osteocytes 5.
Exostosis of the external acoustic canal is over the periosteum and it is recovered by squamous epithelium. It is characterized by the presence of concentric laminas of subtemporal bone, with innumerous osteocytes and few fibrovascular canals 6.
The treatment of osteomas can be conservative or surgical. Conservative treatment prevents external otitis and also conductive hearing loss, caused by the accumulation of desquamated squamous epithelium. It can be made by removing desquamated epithelium and also by using topical antibiotics. Surgical treatment conducted in patients with conductive hearing loss caused by bone obstruction and also in external otitis that are difficult to control clinically 4. Normally, the osteoma can be removed via transmeatal route under local anesthesia 5. Retroauricular approach is indicated when the osteoma is located medially to the isthmus and when it is greater than the isthmus 7. Surgical removal intends to restore the normal size of the external auditory canal using burs and curettes via transmeatal approach under local anesthesia. It is very important to preserve the skin of the external acoustic canal to be placed on the same area and allowing scarring and preventing stenosis of the canal. The surgery can be extremely risky, including risk of tympanic membrane, facial nerve, inner ear and jugular bulb damage, requiring experienced surgeons and enough practice in the procedure 8.
Recurrence of osteoma after complete surgical removal has not been reported yet.
Figure 1. Bone neoformation occupying the EAC.
Figure 2. Osteoma originated from the bony portion of the EAC.
Figure 3. Osteoma on the right, occupying the whole EAC.
Figure 4. Bone neoformation impairing the lumen of the EAC.
Figure 5. Osteoma obliterating the lumen of the EAC.
Figure 6. Osteoma partially obstructing the lumen of the right EAC.
Figure 7. Clinical pathology of an osteoma: internally, we can see the presence of sparse fibrovascular canals, surrounded by bone lamellae.
Case Reports
Case 1
D.C, 31-year-old female patient, she reported sensation of obstruction of the external acoustic canal for 6 years, with hearing loss, intermittent otorrhea and auricular pruritus on the left. She reported past history of suppurated otitis at the age of 4 years.
The physical examination of the left ear detected neoformation, hard upon touching with the knife, occupying the EAC, with hyperemia and epithelial desquamation and otorrhea (Figure 1).
The audiogram showed conductive hearing loss on the left of approximately 20dB.
Computed tomography of the mastoid presented hypopneumatization and sclerosis of the left mastoid cells, left EAC with poorly defined contours and dense areas inside it.
We conducted surgical procedure under general anesthesia, via retroauricular approach. We proceeded with detachment of the skin that recovered the osteoma and we drilled the canal for its removal. Using transmeatal access, we made aspiration of the secretion and lamella of the epithelial desquamation. The tympanic membrane was retracted, thickened and with hyperemia. Lastly, we made a dressing with ointment and gelfoam.
The clinical pathology revealed dense bone recovered by squamous epithelium.
Periodical reviews revealed stenosis of the external acoustic canal that required a new intervention with skin graft to restore permeability. Subsequent controls revealed no abnormalities. Postoperative audiometry was normal.
Case 2
R.S.P, 27-year-old female patient, reported hearing loss on the right for 8 years, associated with repetitive otalgia and otorrhea.
At the otoscopy on the right, we observed hardened neoformation obstructing the whole EAC. The physical examination on the left was normal.
The audiogram presented conductive hearing loss on the right of approximately 40dB and normal left ear.
The CT scan showed presence of implanted bone lesion on the soft tissue of the EAC on the right. Through coronal section, it was possible to observe the stem of the osteoma originating from the bone portion of the auditory canal (Figure 2).
We conducted surgical treatment under general anesthesia via retroauricular access, conducting detachment of skin of the osteoma and drilling of the bone tumor. Through the EAC we aspirated the epithelial mass desquamation. The tympanic membrane was thickened and retracted.
In postoperative controls we did not observe abnormalities. The control audiogram showed a small residual gap of 10 dB.
The clinical pathology analysis detected dense trabecular bone with medullar fibrosis partially recovered with squamous epithelium.
Case 3
I.V, 62-year-old male patient, referred hearing loss for 15 years, with difficult to remove wax. He did not report otorrhea.
Otoscopy on the left revealed obstructed EAC with hard tumor, fixed on the anterior portion.
The audiogram presented mixed hearing loss on the left ear with sensorineural hearing loss in high frequencies after 2kHz and 25dB gap. On the right, there was sensorineural hearing loss in high frequencies after 2kHz.
CT scan showed a single bone mass obstructing the left EAC.
We conducted surgical treatment under local anesthesia with sedation, via transmeatal access. We removed the tumor through a small skin incision, after fracturing it with a curette from its base and drilling the residues. We applied EAC dressing with ointment and gelfoam. Postoperative follow up was uneventful. Control audiogram showed closure of the gap.
The clinical pathology analysis confirmed the diagnosis of osteoma, describing benign bone neoplasm in trabeculae of mature lamellar bone recovered with squamous epithelium without atypia.
Case 4
J.P.S, 28-year-old male patient, with complaint of bilateral hearing loss for 10 years, referring build-up of difficult to remove cerumen. He occasionally presented otorrhea and auricular pruritus.
At otoscopy, we detected a hardened tumor recovered by normal skin on both external auditory canals.
The audiogram presented bilateral conductive hearing loss on the left at about 30d B and on the right at about 20dB.
CT scan showed bone formations originated from the bony portion of the EAC bilaterally, occluding the canal lumen.
The patient was submitted to surgical procedure under general anesthesia and we removed the osteoma with partial detachment of the skin of the left EAC and rupture of the basis. We also proceeded with aspiration of the accumulation of epithelial desquamation. Two months later, we removed the osteoma on the right EAC using similar procedure.
Postoperatively, we followed up both sides for 1 year and did not observe recurrence. There was closure of the hearing gap bilaterally.
The clinical pathology analysis revealed dense trabecular bone recovered with squamous epithelium.
Case 5
O S, 60-year-old female patient, presented complaint of hearing loss on the right for 15 years, presenting repetitive otorrhea since childhood.
At otoscopy on the right ear, we observed a hardened tumor occupying the external acoustic canal on the right fixed to the anterior and superior walls (Figure 3).
She presented right side hearing loss of approximately 20dB in the audiogram, whereas the left ear was normal.
The CT scan confirmed the presence of the right EAC tumor fixed to the bone part of the EAC.
We conducted surgical procedure under local anesthesia plus sedation, and removed the osteoma with partial detachment of the skin via transmeatal access.
Periodical reviews in the postoperative period for 2 years did not present recurrence. The control audiogram showed gap closure.
The diagnosis was confirmed by the clinical pathology.
Case 6
G.G, 32-year-old male patient, had presented hearing loss on the right for 5 years. He reported auricular pruritus, build-up of wax that was difficult to remove, and repetitive external otitis.
At otoscopy, he presented obstruction of the right EAC by subepithelial irregular rounded thickness with normal tympanic membrane.
The audiometry was normal.
The CT scan showed bone neoformation impairing the lumen of the right EAC (Figure 4).
The preferred treatment was removal of the neoformation under local anesthesia, via transmeatal access, with detachment of the skin of the EAC and drilling for the careful removal of the bone thickness so as not to damage the tympanic membrane.
The clinical pathology confirmed diagnosis of osteoma of the right EAC.
There was no recurrence detected in the postoperative follow-up.
Case 7
E.V, 33-year-old male, complaining of left hearing loss for 10 years.
The otoscopy presented hardened tumor partially occupying the left EAC.
At audiometry, we observed mild conductive hearing loss on the left.
We also conducted CT scan confirming the diagnosis of bone tumor originated from the EAC.
The proposed treatment was tumor removal under local anesthesia and via transmeatal access.
The diagnosis of osteoma was confirmed by the clinical pathology. There were no recurrences.
The postoperative control audiometry revealed closure of the gap.
Case 8
S.V.S, 23-year-old female patient, complaining of right hearing loss, with impaction of wax difficult to remove. The case worsened and she manifested repetitive external otitis.
She presented hardened tumor mass partially obstructing the right EAC.
The audiogram showed conductive hearing loss on the right at 40dB.
The bone constitution of the tumor was observed in the CT scan, partially obstructing the right EAC (Figure 5).
We conducted surgery under general anesthesia via retroauricular access, observing a sessile osteoma of the posterior-inferior portion of the right EAC, confirming the diagnosis of osteoma in the clinical pathology study.
In the postoperative 10-month follow-up, there was closure of the gap and no recurrence.
Case 9
N.AS.L, 70-year-old female patient, presented bilateral hearing loss, worse on the left (anacusis). She had used hearing aids on the right for 10 years. She referred episodes of external otitis and difficulty to adapt to the hearing aids (it was not possible to fit the mould).
At otoscopy, we detected a hardened tumor in the right EAC obstructing almost completely its lumen.
The audiogram showed left anacusis and mixed hearing loss on the right with 25dB gap. In the CT scan, we observed a bone lesion that markedly reduced the lumen of the EAC on the right (Figure 6).
After the surgical removal of the tumor, under local anesthesia, via transmeatal access, we confirmed the diagnosis of osteoma in the clinical pathology analysis (Figure 7).
There was closure of the gap postoperatively and no recurrence.
Discussion
According to the literature, osteomas of the EAC can be diagnosed at any age range and they are 3 times more common in men 1.
Miziara et. al (1995) stated that such tumors are not frequent before puberty. Ohhashi et al (1984) referred the more common occurrence among women in the proportion of 2:1 9. In our study, out of 9 studied patients, we had a mean age of 40.6 years, being the minimum age of 23 and the maximum of 70 years. Out of the 9 patients, 5 were female and 4 were male subjects.
As to etiology of osteomas, it is believed that they are a response to the reduction in temperature of the EAC 10.
All the reported cases were osteomas of the EAC. Osteomas located outside the EAC are rare. Eggston and Wolff reported osteomas located in the mastoid 11. Denia et al presented 8 cases of osteoma being that the most common location was the mastoid 12. Osteomas located in the middle ear have already been reported 13, 14. In 1995, Miziara et al reported a case of osteoma located in the internal acoustic canal (IAC).
All patients were submitted to surgical treatment and there was no recurrence detected during the postoperative follow-up. Only in 1 case there was stenosis of the EAC, requiring a new surgical intervention to place a skin graft. After complete removal of the osteoma, recurrences have not been reported 7, 15.
Closing Remarks
External acoustic canal osteoma is an infrequent pathology, benign but with progressive growth that can become symptomatic. The most frequent symptoms related are hearing loss and repetitive otitis that can or not be controlled only with clinical treatment. In cases resistant to clinical treatment, we decide for the surgical approach. The diagnosis should be confirmed by the clinical pathology analysis to rule out other tumors of the region.
References
1. Noordzij JP, Arriaga MA, Stone AB. Differentiating Bony Lesions of the External Auditory Canal. Ear Nose Throat J 1995;74(1):49-51.
2. Bokowy C, Cadot M, Lelièvre G. Patología adquirida del oído externo. Encyclopédie Médico-Chirurgicale, Otorrinolaringología. París: Editions Scientifiques et Médicales Elsevier; 2001. p.1.
3. Morrison WW. Disease of the Ear, Nose and Throat. New York: Appleton-Century Crofts; 1948.
4. Graham MD, Kemink JL. Osteomas and exostoses of the external auditory canal-medical and surgical management. J Otolaryngol 1982;11(2):101-6.
5. Graham MD. Osteomas and exostoses of the external auditory canal. A clinical, histopathological and scanning electron microscopic study. Ann Otol Rhinol Laryngol 1979;88:566-72.
6. Miziara ID, Ianase MM, Bento RF. Osteoma de Conduto Auditivo Interno Associado a Surdez Súbita Contralateral. Rev Bras Otorrinolaringol 1995;61(5):396-8.
7. Sheehy JL. Diffuse exostoses and osteomata of the external auditory canal: A report of 100 operations. Otolaryngol Head Neck Surg 1982;90 (3 pt 1):337-42.
8. Pulec JL, Deguine C. Osteomas of the external auditory canal. Ear Nose Throat J 1993;72(2):112.
9. Ohhashi M, Terayama Y, Mitsui H. Osteoma of the temporal bone - a case report. Nippon Jibiinkoka Gakkai Kaiho 1984;87:590-5.
10. Michaels L, Coucek S. Growth and pathology of the osseous ear canal and its epithelium. J Pathol 1988;154:100 A.
11. Eggston A, Wolff D. Histopathology of teh Ear, Nose and Throat. Baltimore: Williams and Wilkins; 1947. p.471.
12. Denia A, Perez F, Canalis RR, Graham MD. Extracanalicular osteomas of the temporal bone. Arch Otolaryngol 1979,105:706-9.
13. Thomas R. Familial osteoma of the middle ear. J Laryngol Otol 1964;78:805-7.
14. Glassock ME, McKennan KX, Levine SC. Osteoma of the middle ear: a case report. Otolaryngol Head Neck Surg 1987;97:64-5.
15. DiBartolomeo JR. Exostoses of the external auditory canal. Ann Otol Rhinol Laryngol 1979;88(6)[suppl]61:1-20.
1 Ph.D., Professor, UNIFESP- EPM; Head of the Medical Residence Service, Hospital Paulista de Otorrinolaringologia.
2Post-graduation under course, Discipline of Pediatric Otorhinolaryngology, UNIFESP-EPM.
3Resident Physician, Hospital Paulista de Otorrinolaringologia.
4Otorhinolaryngologist.
Affiliation: Hospital Paulista de Otorrinolaringologia.
Rua Dr. Diogo de Faria, 780 - 04037-00 - Tel/Fax: (55 11) 50878700
Study presented at 36o Congresso Brasileiro de Otorrinolaringologia, held on November 18 - 23, 2002 in Florianópolis - SC.
Article submitted on December 12, 2002. Article accepted on March 13, 2003.