Year: 2001 Vol. 67 Ed. 5 - (18º)
Relato de Casos
Pages: 722 to 725
Epiglottis chondrosarcoma: review of the literature and report of one case
Author(s):
José V. Tagliarini 1,
Carlos E. Bacchi 2,
Seizo Yamashita 3,
Cristiane G. Cançado 4
Keywords: chondrosarcoma, larynx, supracriccoid laryngectomy
Abstract:
Chondrosarcoma is the most frequent sarcoma of the larynx. It is more prevalent in the cricoid and less prevalent in the other laryngeal cartilages. Chondrosarcoma is rarely located in the epiglottis. We reported a case of epiglottis chondrosarcoma that was treated with a supracricoid laryngectomy with cricohyoidopexy.
![]()
INTRODUCTION
Chondrosarcoma is a malignant tumor characterized by the formation of cartilage by tumor cells. It normally grows slowly and is rarely found in the head and neck, but the most affected area in the region is the larynx1.
In the larynx, chondrosarcoma is frequent, normally present in patients aged 50 to 70 years, but it may also affect younger people. Man: woman ratio is 3:1. It is normally originated from the cricoid cartilage (75%). However, there have been reports of tumors originated in the thyroid, arytenoid, epiglottis and accessory laryngeal cartilages. The observation of some epiglottic chondrosarcomas goes against the observation that the tumor originates only from hyaline cartilage and not elastic cartilage2,3,5,6,7,12,14.
We report a case of epiglottic chondrosarcoma in a patient aged 35 years and present the review of literature on tumors at this anatomical location.
CASE REPORT
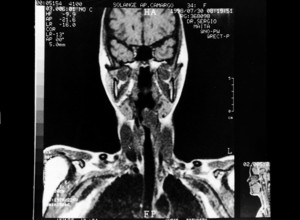
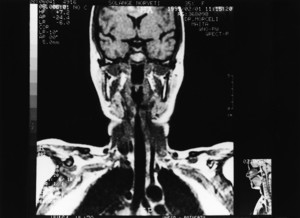
S. A. N. C., female 35-year-old patient, smoker for two years, came to the hospital complaining of muffled voice for four months and difficulty to swallow solids, presenting progressive worsening. At the physical examination, she presented a submucous vegetating lesion that occupied the laryngeal side of epiglottis, extending into the ariepiglotlic and left vestibular folds. The lesion attached the petiole of the epiglottis, but did not affect the glottis or laryngeal mobility. The voice was muffled and the tone was slightly low. Upon palpation, there were no lymph nodes in the neck. At endoscopy, the lesion affected the two anterior thirds of the vocal folds, sparing the rest of the vocal folds and arytenoids and laryngeal mobility was preserved. We conducted a biopsy that confirmed the diagnosis of low grade malignant chondrosarcoma. After the biopsy, we assessed the extension of the tumor with magnetic resonance imaging. The test at T1 axial and coronal sections with and without contrast showed solid evident lesion with hyposignal. There was peripheral enhancement after intravenous injection of contrast and the borders were irregular. The tumor was restricted to the supraglottis, located in the epiglottis, and had an apparent distortion of the pyriform sinus on the left. It was an asymmetrical lesion measuring 3-3.5cm in diameter. As to T2 protons density, it presented increase in signal intensity. Since the lesion was restricted to the supraglottis and laryngeal mobility was preserved, a supraglottic laryngectomy was scheduled. During the surgery, we expanded the resection and performed a subtotal laryngectomy with cricohyoidopexy. We removed the preepiglottic space and thyroid cartilage and preserved both arytenoids, all the cricoid cartilage and hyoid bone. Next, we conducted the pexy of the cricoid at the hyoid bone, with sutures that reconstructed the larynx. On the 11th postoperative day, we removed the tracheotomy cannula. Since the first week after the surgery, the patient was submitted to swallowing rehabilitation. She presented an episode of aspiration pneumonia on the 20th postoperative day and after 30 days, it was possible to remove the nasogastric tube. Pathology showed at macroscopy that the lesion compromised the whole epiglottis, had a bocellated aspect, white color and myxoid areas with cartilaginous consistence. It measured 3.7x2.5x2,5cm. Microscopic analysis showed that it was a well differentiated chondrosarcoma of low malignancy grade. Thirty days after surgery, the patient had no tracheotomy, was eating normally and had an acceptable voice, although low in tone. In the control MRI test carried out six months after surgery there were no signs of recurrence. Currently, she has good health status, no signs of recurrence in the clinical examination, normal swallowing and, despite vocal rehabilitation, she still has a low voice.
Figure 1. Surgical piece of epiglottis tumor. The tumor mass is bocellated and the external surface is smooth, glossy and had areas of focal hemorrhage.
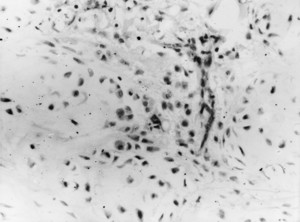
Figure 2. Histology section of chondrosarcoma showing lobulated growth pattern and moderate cellularity. Neoplasic cells have a lacumnar aspect and hyperchromic nuclei (hematoxyllin: 200x).
DISCUSSION
Chondrosarcomas are submucous lobulated masses, rounded or oval tumors recovered by intact laryngeal mucosa. In general, it has hardened consistency, but there may be soft portions and some areas with cystic degeneration. It tends to progress within a cartilage and it rarely extends outside the external perichondrium, invading the surrounding tissues4, except in cases of recurrence.
Chondrosarcomas may be of low grade (Grade I), middle grade (Grade II) or high grade (Grade III). The histology pattern of low grade chondrosarcoma is similar to that of a benign chondrosarcoma. In grade I, the neoplasia consists of abundant basophilic and metachromatic matrixes, in which cells present small and hyper-stained nuclei. In some cases, there are binucleated or multinucleated cells. Nuclear irregularities and prominent nucleoli are indications of malignancy. Mitoses are generally absent4. Middle grade chondrosarcomas present growing cellularity, especially in the periphery of lobules. Mitoses are scarce. High grade chondrosarcomas have pronounced cellularity with large binucleated and multinucleated cells. Mitoses are frequent1.
Laryngeal chondrosarcoma is locally aggressive, although it may suffer metastases by hematogenic or lymphatic routes. Metastases are more frequently found in the lungs and regional lymph nodes. There may be metastases in the kidney, spleen and cervical vertebrae3.
Chondrosarcoma is the most frequent malignant mesenchymal neoplasia of the larynx11. In a recent review, Nicolai et al. listed approximately 200 cases of laryngeal chondrosarcoma reported in the literature11.
The symptoms presented in patients with such a tumor consist of progressive hoarseness, dyspnea and dysphagia, varying according to tumor location. Dyspnea is predominant if the neoplasia has anterior extension into the lumen of the airways. If the tumor develops posteriorly into the pharynx, it may cause dysphagia. Since neoplasias are usually of slow growth, patients get adapted to the progressive narrowing of the airways, until an episode of acute dyspnea leads them to emergency tracheotomy. As described in the literature, the first clinical sign may be vocal fold paralysis apparently not associated with laryngeal and non-laryngeal lesions, denominated idiopathic lesions. Vocal fold paralysis is an early sign of chondrosarcoma of the cricoid cartilage and it may be related to the involvement of the recurrent nerve or fixation of cricoarytenoid joints8,11.
Figure 3. Axial section of magnetic resonance imaging test showing the supraglottic tumor.
Figure 4. Coronal section of magnetic resonance imaging study showing the extension of the tumor.
Figure 5. Coronal section of control magnetic resonance imaging showing appropriate laryngeal lumen, with no signs of tumor recurrence.
Laryngeal chondrosarcoma is rarely described in the literature as a primary epiglottic affection3,5,6,7,14. If originated from the epiglottis, involving the supraglottic region, supraglottic resection is the preferred treatment option3,6. Laryngeal chondrosarcoma should be treated with a wide incision, with preservation of the larynx and partial laryngectomy, and if possible, preservation of the laryngeal framework to prevent stenosis4. In the present case, supraglottic resection was not possible because of the invasion of the epiglottis petiole. Since both vocal folds were free from lesion in their anterior third and presented normal mobility, with intact arytenoids, we decided for a wider resection (subtotal laryngectomy, with cricohyoidopexy according to the technique described by Laccourreye)9. We believe that this technique is safe for resection of chondrosarcomas restricted to the supraglottis. We did not perform neck resection in the patient because most reports informed that cervical metastases are of low incidence and the procedure is indicated in case of clinically compromised lymph nodes11.
The prognosis of neoplasia depends on the extension of the tumor, its degree of differentiation and also appropriate primary treatment. Grade I chondrosarcoma normally shows local malignancy with minimal tendency of metastases. Metastases are more common in grade II and III chondrosarcomas1.
REFERENCES
1. FERLITO, A. - Cartilaginous and osteogenic neoplasm 305-26. Ferlito, A.: Neoplasm of the larynx. 1st edition Churchill Livingstone, 1993.
2. FERLITO, A. - Laryngeal fibrosarcoma: an over-diagnosed tumor. ORL J. Otorhinolaryngol. Relat. Spec, 52:194-5, 1990.
3. FERLITO, A.; NICOLAI, P.; MONTAGUTI, A.; CECCHETTO, A.; PENNELLI, N. - Chondrosarcoma of the larynx: review of the literature and report of three cases. Am. J Otolayngol., 5:350-9, 1984.
4. FINN, D. G.; GOEPFERT, H., BATSAKIS, J. G. - Chondrosarcoma of the head and neck. laryngoscope, 94:1539-44, 1984.
5. GRAY, S.D.; BLANKE, S.B.; BABIN, R.W.; ROBINSON, R.A. Chondrosarcoma of the epiglottis with pulmonary metastases. Abstract, Scientific Poster. Presented at the Annual Meeting of the American Academy of Otolaryngology-Head and Neck Surgery, Inc, Las Vegas, 1984.
6. JACOBS, R.D.; STAYBOLDT, C.; HARRIS, PJ. - Chondrosarcoma of the epiglottis with regional and distant metastasis. Laryngoscope, 99: 861-4, 1989.
7. KASANZEW; JOHN, D.G.; NEWMAN, P.; LESSER, T. J. H.; THOMAS, P.L. - Chondrosarcoma of the epiglottis. J. Laryngol. Otol., 102:374-7, 1988.
8. KRAMER, D.S.; BROWN, G.P.; SCHULLER, D.E. - Proximal airway obstruction presenting as dyspnea. A case of chondrosarcoma of the larynx. Posgrad. Med., 5.133-5, 1983.
9. LACCORREYE, H. et al. - Supracricoid laryngectomy with cricohyoidopexy: a partial laryngeal procedure for selected supraglottic and transglottic carcinomas. Laryngoscope, 100:735, 1990.
10. LEONETTI, J.P.; COLLINS, S.L.; JABLOKOW, V.; LEWY, R. - Laryngeal chondrosarcoma as late-appearing cause of "idiopathic" vocal cord paralysis. Otolaryngol. Head Neck Surg., 97:391-5, 1987.
11. NICOLAI, P.; FERLITO, A.; SASAKI, C.T., KIRCHNER, J.A. - Laryngeal Chondrosarcoma: Incidence Pathology, Biological Behavior, and Treatment. Ann. Otol. Rhinol. Laryngol., 99.515-23, 1990.
12. R$THI, A. Quoted by BRONZINI, E. - Condrosarcoma della laringe. Ann Laringol Otol Rinol Faringol., 58:497-509, 1959.
13. SHEARER, J.E.; GOLDBERG, A.L.; LUPENTIN, A.L.; ROTHFUS, W.E. Chondrosarcoma of the larynx. Report of a case with characteristic computed tomography findings. J. Comput. Tomogr, 12.292-4, 1988.
14. WILKINSON, A.H. III; BECKFORD, N.S., BABIN, R.W., PARHAM, D.M. - Extraskeletal myxoid chondrosarcoma of the epiglottis: case report and review of the literature. Otolaryngol. Head Neck Surg., 104:257 60, 1991.
1 Professor of the Department of Ophthalmology, Otorhinolaryngology and Head and Neck Surgery, Faculdade de Medicina de Botucatu - UNESP.
2 Professor of the Department of Pathology, Faculdade de Medicina de Botucatu - UNESP.
3 Professor of the Department of Radiological Diagnosis, Faculdade de Medicina de Botucatu - UNESP.
Resident Physician, Department of Pathology, Faculdade de Medicina de Botucatu - UNESP.
Address correspondence to: Jose Vicente Tagliarini - Departamento de Oftalmologia, Otorrinolaringologia a Cirurgia de Cabeça a Pescoço - Faculdade de Medicina de Botucatú - UNESP - Distrito de Rubião Junior, s/n - 18618-000 Botucatu /SP - Te/ Fax. (55 14) 6802-6256.
Article submitted on April 24, 2000. Article accepted on February 6, 2001.