Year: 2001 Vol. 67 Ed. 5 - (14º)
Artigos Originais
Pages: 695 to 700
Surgical treatment for aspiration
Author(s):
Dayse Manrique 1,
Rogério B. Bühler 2,
Erich C. M. Melo 2
Keywords: surgery, aspiration, dysphagia
Abstract:
Introduction: Alteration of normal laryngeal function may result in life threatening aspiration and may cause pulmonary complications. Aim: The aim of this paper is to report 15 cases of surgical treatment of chronic aspiration, including surgical techniques, results and complications. Study design: Retrospective chart review. Material and method: 15 patients were treated between 1997 and 2000, who underwent surgical treatment of aspiration at AACD - São Paulo /SP. Surgical procedures were: supraglottic, glottic or subglottic closure. We analyzed sex, age, primary diagnostic, prior tracheotomy, oral or nonoral feeding, incidence of pneumonia, followup and complications. Results: eight patients were male and seven were female. The mean age was nine years and two months. The most frequent primary diagnostic was chronic encephalopathy. Prior tracheotomy were performed in ten patients. Nine patients were able to eat after surgery at least 50% of them required intake. All 15 patients reduced the incidence of pneumonia. The follow-up ranged from four to 36 months. One patient had a separation of the epiglottis from the larynx postoperatively. Conclusion: Surgical treatment of chronic aspiration with laryngeal closure is to be considered in reducing the incidence of pneumonia and improving quality of life.
![]()
INTRODUCTION
The human larynx is responsible for three very important functions: protection of airways, respiration and phonation. If the protective laryngeal mechanism is functionally blocked, the patient may experience aspiration. The degree of aspiration and its clinical repercussions indicate the need for clinical or surgical treatment. The first clinical description of aspiration was credited to Hippocrates and the first scientific investigation was made by Hunter14.
Before selecting the technique to control the process of aspiration, it is important to consider which anatomical and functional alterations are present. The factors that protect the lower airways from aspiration are basically: apnea during breathing, elevation of larynx and action of aryepiglottic folds directing the bolus laterally to the pyriform recesses. Among the intrinsic mechanisms of the larynx, the protection of lower airways is performed by approximating the vocal folds, followed by adduction of vestibular folds and anterior-posterior contraction of the arytenoids towards the epiglottis. The closure of vocal and vestibular folds derives from the contraction of the thyroarytenoid muscle. Glottic closure has a function of laryngeal protection which is phylogenetically very important16,25.
These mechanisms, together with preserved sensitivity, appropriate contraction of constrictors, inhibition of cricopharyngeal contraction and esophageal integrity, enable an aspiration-free swallowing. Any variation of the process may lead to minor or catastrophic aspiration.
Etiology of aspiration may be distributed in four categories: neurological affections, laryngeal or pharyngeal tumors, secondary anatomical alterations after surgery (head and neck tumor resections) and traumas.
Indications and moment of surgery
Since the indications for surgical intervention do not directly depend on etiology of aspiration, the best moment to perform the surgery and the technique to be employed should be considered according to the affection and the prognosis of the underlying disease6.
After extensive head resections, the reconstruction should be planned so as to prevent aspiration in its primary procedure, such as for example, laryngeal suspension.
Surgical intervention should be considered when no further resolution or clinical improvement is expected in the short run. Surgical approach should not be considered until all conservative methods have been exhaustively employed for at least six months, because behavioral measures and speech therapy may rehabilitate 80% of the patients with oropharyngeal dysphagia10. The same does not apply to patients who present severe pulmonary infections with high risk of asphyxia and death, or when a quick deterioration of pulmonary conditions is noticed. Surgery is indicated when the patient is unable to control aspiration of its own secretions and saliva, with respiratory repercussions and pulmonary infections3,7,12,28.
Clinical assessment
The assessment will be considered complete after the ENT examination, emphasizing the exploration of cranial nerves and laryngeal examination. Nasofibrolaryngoscopy will provide information, especially if complemented with functional assessment of swallowing21.
Radiological assessment consists of swallowing videofluoroscopy (VF), using barium sulfate. The dynamic process and the motor functions of the muscles involved in swallowing are studied.
Clinical treatment of aspiration
The most significant measure to control aspiration is to prevent it, restricting oral feeding and minimizing gastric reflux to the esophagus, pharynx, larynx and lower airways, preventing aspiration pneumonia26. Nutritional support required is made by alternative feeding routes.
Feeding through nasoenteral tube is maintained for up to 6 months23. From then on, the risks of complications are minimized by percutaneous gastrostomy. Gastroesophageal reflux disease should be well evaluated, defining early clinical, or surgical treatment, since the incidence of pulmonary infection is higher when the aspirated content is acid2,6.
Saliva aspiration may be minimized by using anticholinergic drugs, prescribed 30 minutes before the first meal14. Other measures include dental and periodontal treatment, spontaneous elimination of saliva from the oral cavity, aspiration of the oral cavity and oropharynx. Radiotherapy of the parotid and submandibular glands, at 1,500rads, may prevent the production of saliva by these glands2.
Surgical treatment of aspiration
A number of surgical techniques may be employed to control aspiration, with more conservative or radical interventions. Among the conservative procedures, we may list medialization of vocal folds, laryngeal suspension, epiglotoplasty, translaryngeal resection of cricoid lamina, application of toxin botulinum in the pharyngoesophageal segment, or myotomy of the cricopharyngeal muscle. Radical procedures include temporary or permanent tracheostomy, the use of cannula with insufflated balloons, glottic prostheses (endolaryngeal molds), and separation of air and digestive routes: glottic, supraglottic and subglottic occlusion. Laryngectomy was the only therapeutic option for clinically intractable aspiration in the past, but it is rarely employed today, because other techniques may be used with low morbidity, high levels of success and reversibility potentials14.
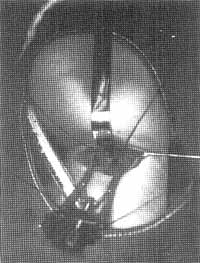
Figure 1. Glottic occlusion, laryngofissure and vocal fold debridment.
Figure 2. Subglottic occlusion. Laryngotracheal separation.
Figure 3. Subglottic occlusion. Transversal section at the level of the third tracheal ring.
Figure 4. Tracheoesophageal fistula. Wide communication between the trachea (anterior) and the esophagus (posterior).
The purpose of the present study was to report 15 cases of surgical treatment to control aspiration, the underlying etiology of the patients submitted to treatment, the employed surgical techniques, its uses, results and complications.
MATERIAL AND METHOD
Fifteen patients were submitted to surgery to control aspiration, and one of the patients was submitted to two procedures, amounting to 16 surgeries, from April 1997 to April 2000, performed by the authors, at Hospital AACD.
Surgeries were conducted under general anesthesia with orotracheal intubation or via tracheostomy, in patients previously submitted to the procedure.
The surgical techniques employed were divided into: supraglottic laryngeal occlusion - Kitahara17, in which the closing suture happens between the vestibular folds, by laryngofissure; glottic occlusion - Montgomery22 (Figure 1), in which the suture is made with the vocal folds after deepithelization, with access through laryngofissure; subglottic occlusion - Lindeman19,20 (Figures 2 and 3), in which laryngotracheal separation with section at the level of the second tracheal ring, implantation of the distal skin stump, and closure in itself of the proximal stump. The selection of the technique was based on the underlying disease and prognosis of the recovery of cognitive and laryngeal functions.Table 1. Distribution of the 15 subjects according to etiology of underlying disease.
Table 2. Feeding route of the 15 studied patients before surgery to control aspiration.
Table 3. Feeding route of the 15 studied patients after the surgery to control aspiration.
Table 4. Surgical techniques to control aspiration used with the 15 studied patients.
Indication of the surgery was one of the last therapeutic resources, after long and tiring clinical treatments that did not improve the clinical condition of the patient.
RESULTS
Out of 15 patients submitted to surgery, eight were male (53.3%) and seven were female patients (46.7%). As to underlying disease, five patients presented neurological diagnosis of non-progressive chronic encephalopathy, four patients of encephalic vascular accident, two of cranial-encephalic traumatism (CET), two with progressive chronic encephalopathy, one with Arnold Chiari's syndrome and one with Rett's syndrome (Table 1).
Ages ranged from two years and 6 months to 19 years and 3 months, mean age of 9 years and 2 months. Out of 15 patients, 10 were submitted to tracheotomy before surgery, within an interval that varied from 12 months to 64 months, mean of 39 months. All patients had complete restriction of oral feeding at the time of surgery and 12 used gastrostomy, and 3 cases had nasoenteral tube (NET) (Table 2).
After the surgery, 7 patients started to be fed exclusively through the oral route, and three of them had postoperatively used NET, whereas 4 used gastrostomy. Two patients had combined diet divided into 50% of daily content through oral route and 50% through gastrostomy. One patient had combined diet as follows: 10% oral feeding and 90% gastrostomy. Five patients progressed with an exclusive diet through gastrostomy, because of the neurological affection and oral motor compromise that prevented the patient from feeding himself orally (Table 3).
Follow-up of patients varied from 4 to 36 months, and weekly visits were scheduled in the first month, followed by monthly visits after that. All patients were submitted to complete ENT. examination, functional nasofibrolaryngoscopy of swallowing and videofluoroscopy (VF)of swallowing. Complementary tests showed absence of tracheal aspiration in 14 patients and the authors noticed the presence of contrast in the subglottic region and trachea of patients submitted to supraglottic occlusion. In a patient submitted to glottic occlusion, food contrast and barium were identified in the supraglottic region. In 10 patients submitted to subglottic occlusion, VF revealed that there was barium in the proximal segment of the trachea.
All patients referred to surgery were submitted to routine preoperative tests, evaluated by a multidisciplinary team and discharged when clinical conditions were appropriate. They were submitted to swallowing functional nasofibrolaryngoscopy and VF to evaluate the degree of aspiration and any other alterations related to oropharyngeal transit: extra-oral leak, residue of contrast in the oral cavity and pharynx, early leak of contrast into the pharynx, and effective cough after aspiration.
The surgical techniques employed were: Kitahara17 (five cases), Montgomery22 (one case) and modified Lindeman19,20 (ten cases) (Table 4).
As to complications, one patient presented tracheocutaneous fistula after surgical laryngotracheal separation, with complete resolution after clinical treatment (oral antibiotic and NET feeding). One patient presented tracheoesophageal fistula (Figure 4), preoperatively diagnosed and surgically corrected at the same time. One patient presented partial dehiscence of the suture of the posterior vestibule, when using the supraglottic occlusion technique. Three patients presented pulmonary infection sometime during the procedure, progressing with outpatient treatment.
Patients presented preoperatively an average of one episode/month of antibiotic use for pulmonary or tracheobronchial infection, requiring hospitalization 50% of the time. After the surgery, the 15 studied patients started to control the number and frequency of pulmonary infections, using antibiotics once/3 months, complying with outpatient treatment in 90% of the times.
DISCUSSION
Morbidity related to tracheal aspiration is frequently seen in patients with severe dysfunction of upper airways and digestive tract, even when all support measures have already been adopted3,4,27. The use of drugs to reduce salivary secretion has partial success because of side effects, such as drying of mucosas and tachycardia. According to the report by Lawless18, even in the presence of reduced aspirated volume, the number of episodes of aspiration does not decrease. The control of gastroesophageal reflux disease (GERD) may be obtained through surgery, which happened in seven of our patients (43.75%) submitted to open Nissen type fundoplication.
Previous tracheostomy as an initial treatment measure for aspiration reduces the incidence of pulmonary infections, if we use a cannula with balloon, which will serve as a mechanical protection barrier. However, there may be an aggravation of aspiration because of the alteration of laryngeal elevation during swallowing, leading to worsening of aspiration13. In addition, the use of the insufflated balloon promotes esophageal compression, which may lead to ischemia and tracheal necrosis, progressing to tracheoesophageal fistula, which happened with one of our patients. Therefore, if there is clinical treatment failure, despite the performance of tracheostomy, the surgery to control aspiration should be considered.
A number of surgeries to control aspiration have been described since the beginning of the century, in cases of vocal fold paralysis, such as medialization of folds with injections of paraffin, described by Bruningo in 19115; Teflon, in 1962, described by Arnold1; or Gelfoam paste, in 1978, described by Schranm24. Other surgical treatments include myotomy of cricopharyngeal muscle, when there is sustained contraction of the muscle. Procedures that reduce saliva are described, such as: exeresis of submandicular or parotid glands, ligation of parotid ducts or use of radiation, as described by Diamant8.
The most effective surgeries are related to laryngeal closure, which can be: glottic, supraglottic or subglottic, as initially described by Montgomeryzz, Habal and Murray15 and Lindeman19, respectively. The techniques we used were supraglottic occlusion by Kitahara17; subglottic occlusion by Lindeman19,20 modified by the author, leaving a subglottic reservoir, and the technique described by Montgomery22.
The selection of type of occlusion was related to potential of technical reversibility, the facility to perform it in each age range, and the success rate in controlling aspiration. The technique described by Montgomery22, despite the reversibility considered by the author, is the most technically difficult in children, and it was used in only one case, which had no prognosis concerning recovery of laryngeal functions.
Lindeman's19,20 technique is the one that has the highest likelihood of being reversed, employed in 10 cases. None of the patients presented enough neurological improvement to use oral communication that justified the attempt to reverse the procedure, although ii was possible, as reported by Lindeman20.
Three patients died during the follow-up and in no cases there was pulmonary disease or associated surgical complications, and the death causes were related to the underlying etiology9. Some authors reported that in the follow-up of laryngotracheal separation, the formation of tracheocutaneous fistula is uncommon and self-limited10,11. In our follow-up, only one patient presented early postoperative fistula, improving after clinical treatment.
There was marked control of frequency and severity of pulmonary infections, and in less than 10% of the times they required hospitalization, reflecting the exclusion of an important aggressive pulmonary factor, that is, aspiration. However, the degree of pulmonary sequelae of repetitive infections supported the development of mild and lower risk pulmonary complications.
CONCLUSION
The surgeries to control pulmonary aspiration with the three used techniques were effective to prevent aspiration with low intra and postoperative morbidity, with precise indications.
The complete restoration of oral feeding was observed in 4 cases that previously used gastrostomy, and partial restoration (50%) was obtained in two cases that still maintained gastrostomy. In the other cases, owing to significant impairment of motor oral functions, there was no rehabilitation of oral feeding.
All the 15 studied patients progressed with significant reduction of number and severity of episodes of pulmonary infections, observed by absence of hospital admissions and use of antibiotics, reflecting an improvement in the clinical picture of patients, as well as in the quality of life of patients and family members.
REFERENCES
1. ARNOLD, G. - Vocal Rehabilitation of Paralytic Dysphonia. Arch Otolaryngol 73:290-4, 1961.
2. BARTELETT J.G., GORBACH S.L. - The Triple threat of aspiration pneumonia. Chest 68:560-6, 1975.
3. BAUER, M.L.; FIGUEROA-COLON, R.; GEORGESON, K. et al. - Chronic Pulmonary Aspiration in Children. South Med J 86:789-95, 1993.
4. BLASCO, P.A.; ALLAIRE, J.H. - Drooling in the Developmentally Disabled: Management Practices and Recommendations. Dev Med Child Neurol, 34:849-62, 1992.
5. BRUNINGS, W. - Ueber Eine Neue Behanddlungsmethode der Recurrenslahmung, Verh Dtsch Laryng 18.151(583), 1911.
6. BUCHHOLZ, D.W.; ROBBINS, J. - In Perlman, A.L.; DELRIEU, K.S. Deglutition and its Disorders, 1st ed., San Diego, Singular Publishing Group, 1997.
7. COOK, S.P.; LAWLESS, S.T.; KETTRRICK, R. - Patient Selection for Primary Laryngotracheal Separation as Treatment of Chronic Aspiration in the Impaired Child. IntJPed Otorhinolaryngol 38: 103-6, 1996.
8. 1997 DIAMANT, H. - Ligation of the Parotid Duct in recurrent parotitis. Acta Otolaryngol (Stock) 49:375-80, 1958.
9. EIBLING, D.E; SNYDERMAN, C.H.; EIBLING, C. - Laryngotracheal Separation for Intractable Aspiration: A Retrospective Review of 34 Patients. Laryngoscope, 105: 83-5, 1995.
10. EISELE, D.W. - Surgical Approaches to Aspiration. Dysphagia 6: 71 8, 1991.
11. EISELE, D.W.; YARINGTON, C.T.; LINDEMAN, R.C. - Indication for the Tracheoesophageal Diversion Procedure and the Laryngotracheal Separation Procedure. Ann Otol Rhinol Laryngol, 97.471-5, 1988.
12. ELIDEMIR, O.; FAN, L.L.; COLASURDO, G.N. - A Novel Diagnostic Method for Pulmonary Aspiration in a Murine Model. Am. J. Respir. Crit. Care Med 161: 622-626, 2000.
13. GILBERT, R.W.; BRYCE, D.P.; MCILLWIN, J.C. - Management of Patients with Long term Tracheotomies and Aspiration. Ann Otol Laryngol, 96561-4, 1987.
14. GOODE, R.L; LEVINE, P.A. - Surgery for Aspiration. In: Surgery of the larynx. Bayley and Biller. W.B. Sauders Company, 399-416, 1985.
15. HABAL, M.B.; MURRAY, J.E. - Surgical Treatment of Life Endangering Chronic aspiration Pneumonia: Use of an Epiglottic flap to the Arytenoids. Plast, Reconstr Surg., 49:305-11, 1972.
16. KIDDER, T.M. - Esophago/Pharyngo/Laryngeal Interrelationships: Airway Protection Mechanisms. Dysphagia 10: 228-31, 1995.
17. KITAHARA, S.; IKEDA, M; OHMAE Y; NAKANOBOH, M; INOUYE, T; HEALY, G. - Laryngeal closure at the level of the false cord for the treatment of aspiration. J Laryngol Otol, 107.826-8, 1993.
18. LAWLESS, S.T.; COOK, S.; LUFT, J.; JASSANI, M.; KETTRICK, R. - The Use of a Laryngotracheal Separation in Pediatric Patients. Laryngoscope 105:198-202, 1995.
19. LINDEMAN, R.C. - Diverting the Paralyzed Larynx: a Reversible Procedure for Intractable Aspiration. Laryngoscope 85: 157-180, 1975.
20. LINDEMAN, R.C.; EISELE, D.W. et al. - The Tracheoesophageal Diversion and Laryngotracheal Separation Procedures for Treatment of Intractable Aspiration. Am. J. Surg. 157: 230-6, 1989.
21. LOGEMANN, J.A. - In: Evaluation and treatment of swallowing disorders. Pro-ed - 2nd ed., 1998.
22. MONTGOMERY, W.W. - Surgery to Prevent Aspiration. Arch Otolaryngol, 101:679-82, 1975.
23. MORRIS, S.E. - Development of oral-Motor Skills in the Neurologically Impaired Child Receiving Non-Oral Feedings. Dysphagia 3:135-54, 1989.
24. SCHRAMM, V.L. et al - Gelfoam Paste Injection for Vocal Cord Paralysis: Temporary Rehabilitation of Glottic Incompetence. Laryngoscope 88:1268-73, 1978.
25. SHAKER, R.; DOODS, W. J.; DANTAS, R.O.; HOGAN, W. J. - Arndorfer, R.C. Coordination of Deglutive Glottic Closure with Oropharyngeal Swallowing. Gastroenterology 98:1478-84, 1990.
26. TANIGUCHI, M.H.; Moyer, R.S. - Assessment of Risk Factors for Pneumonia in Children Significance of Videofluoroscopic Swallowing Evaluation. Dev Med Child Neurol 36: 495 502, 1994.
27. TERRY, P.B. - Pulmonary Consequences of Aspiration. Dysphagia, 3:179-83, 1989.
28. ZURICK, N. J.; HENDERSON, A.J.W.; LANGTON-HEWER, S.C. - A Method for Bronchoscopic Evaluation of Salivary Aspiration in a Disabled Child. Eur Respir J., 15: 424-5, 2000.
1 Doctorate studies under course at the Discipline of Otorhinolaryngology and Human Communication Disorders, Universidade Federal de São Paulo - Escola Paulista de Medicina; Assistant Physician, Hospital do Servidor Público Estadual - Francisco Morato de Oliveira - São Paulo /SP; Otorhinolaryngologist with the Clinic of Dysphagia at AACD - São Paulo /SP.
2 Resident Physician, Service of Otorhinolaryngology and Head and Neck Surgery, Hospital do Servidor Público Estadual Francisco Morato de Oliveira - São Paulo /SP;
Volunteer Otorhinolaryngologist, Clinic of Dysphagia at AACD = São Paulo
Address correspondence to: Dayse Manrique - Rua Canário, 112 - apt°. 61 - Moema - 04521-005 São Paulo /SP. E-mail: daysemanrique@uol.com.br
Article submitted on April 10. 2001. Article accepted on June 18. 2001.