Year: 2002 Vol. 68 Ed. 5 - (25º)
Relato de Caso
Pages: 761 to 766
Otoacoustic emissions in early diagnosis of cochlear lesions in Ménière's disease
Author(s):
Antonio M. C. M. Aquino 1,
Carolina A. M. Massaro 2,
Juliana B. Tiradentes 3,
Juan C. V. Garzón 4,
José A. A. Oliveira 5
Keywords: Ménière, otoacoustic emission, cochlea, endolymphatic hypertension
Abstract:
Fluctuating deafness predominating in low frequencies can occur in the early phase of Ménière disease, together with changes in otoacoustic emissions (OAE) at the frequencies corresponding to the fluctuating ones, which are not correlated with the auditory thresholds detected in tone audiometry. In experimental studies, these changes are not related to the loss of outer hair cells (OHC) in the cochlear apex and their cause is still unclear, possibly corresponding to alterations in the hydrodynamic and biomechanical micromechanism of the cochlea. The OAE observed in the present case showed cochlear alterations in the early compensated phase of Ménière disease which cannot be detected by tone audiometry or standard examinations. Thus, this examination can reveal early lesions due to alterations of the cochlear micromechanism only.
![]()
INTRODUCTION
Otoacoustic emissions (OAE) were initially observed by the Englishman David Kemp, in 1978, who defined them as the release of sound energy from the cochlea, prolonged into the middle ear up to the external auditory canal. He demonstrated that evoked otoacoustic emissions are present in all functionally normal ears and that they are no longer detected when the auditory thresholds are greater than 20 30 dB (Kemp et al., 1986).
OAE are subliminal sounds detected in the external auditory canal, generated by outer hair cells, and serve as a test indicated for the diagnosis of various cochlear pathologies, including Meniere disease. It has been useful in high risk nursery for hearing screening, as a complementary test to ABR for topodiagnosis of retrocochlear affections and in research studies. It is a promising technique for auditory diagnosis because it is simple, quick and non-invasive (Isaac and Aquino, 1998).
The recent discovery of OAE contributed substantially for the formation of a new concept about cochlear physiology, showing that it is capable not only of receiving sounds, but also of producing acoustic energy through the active electrobiomechanical process of the cochlea. This phenomenon has recently been attributed to the rapid and slow contractions of outer hair cells and it is controlled by means of efferent auditory pathways (Oliveira, 1997).
Otoacoustic emissions are considered a clinical instrument to monitor cochlear function. There is evidence that a small abnormality in cochlear functioning can be detected by otoacoustic emissions, even before any audiogram abnormalities are detected (Carnicelli, 1997). Otoacoustic emission detection threshold is below the subjective threshold in about 10dB (Oliveira, 1997). Thus, otoacoustic emissions are indicated for short, medium and long term monitoring. (Carnicelli, 1997).
Since it is a more sensitive test than pure tone audiometry, auditory monitoring through evoked otoacoustic emissions is indicated in noise induced hearing loss (NIHL), ototoxicity and Meniere disease. In endolymphatic hydrops or Meniere disease, the presence or absence of OAE distortion product (OAE-DP) help define whether the disease is compensated (with fluctuating loss) or uncompensated (definite hearing loss) (Lopes Filho et al., 1997).
Patients with Meniere disease present symptoms related to the involved of vestibular and auditory systems. Even though different theories have been proposed to explain the changes in sensitivity of the disease, the cochlear abnormalities responsible for them have not been clearly defined yet. The dominating theory in Meniere disease research is that it is caused by increased pressure owing to accumulation of endolymph. This condition can be experimentally created in animals by the obstruction of the endolymphatic sac, which generally leads to endolymphatic hydrops, with results similar to those found in humans. However, the underlying mechanisms of sensitivity abnormalities experimentally detected have not fully explained yet (Harris and Probst, 1991).
Rapid abnormalities of sensitivity in low frequencies are noticed in the first days after onset of hydrops in guinea pigs, with affection of OAE thresholds in corresponding frequencies. Since the hair cells are not destroyed during the first stages of the disease, the authors proposed that it is a result of the both hydrodynamic and biomechanical micromechanisms that affect the transmission of the stimulus through the outer hair cells of Corti's organ. It is likely that many factors be responsible for the mechanical complexes responsible for the hearing loss found in Meniere disease, even though we know that increased endolymphatic pressure acts directly or indirectly on outer hair cells, it is still difficult to correlate experimental findings in animals with the symptoms found in humans (Horner and Cazals, 1989).
Our objective was to show that initial Meniere disease could manifest fluctuating hearing loss predominantly in low frequencies and also late abnormalities of OAE in the corresponding fluctuating frequencies that were not correlated to the hearing thresholds of the pure tone audiometry. Thus, OAE can show early cochlear affection in initial Meniere disease that is not detectable yet by means of pure tone audiometry and conventional tests.
CASE REPORT
NN, 32-year-old male physician, married, presented one year before an episode of mild sudden hearing loss, continuous low frequency tinnitus and left ear fullness, concomitant with rotation dizziness that lasted some minutes and worsened with head movement. The patient did not report use of drugs, prolonged exposure to noise, metabolic diseases, allergies or viral disease symptoms the days before the episode. At that time, physical examination was normal, except for Romberg test, which showed slight lateral pulse. Pure tone audiometry revealed mild sensorineural hearing loss in low frequencies on the left. Tympanometry, stapedial reflex and speech recognition index were within normal ranges in both ears.
After 10 days, there was complete remission of clinical symptoms and also normalization of pure tone thresholds, characterizing it as a fluctuating deafness typical of initial Meniere disease (Figure 1 A).
The patient was diagnosed as having initial Meniere disease on the left year confirmed by an Otorhinolaryngologist based on clinical criteria optimized by the hearing fluctuation in pure tone audiometry. Complete blood count revealed: red blood cells - 5.36 (million/mm3), HGB - 14.5 g/dl, HTC: 42.9% and erythrocyte sedimentation rate - 6 mm/h; total leukocytes - 6.1 million/mm3, segmented - 65.8%, eosinophils - 1.3%, basophils - 0.1%, lymphocytes - 23%, monocytes - 9.8%. Glycemia - 85.1mg/dl, cholesterol - 181mg/dl, triglycerides - 50 mg/dl, TSH - 2,8UIU/ml and free T4 - 1.5µg/ml.
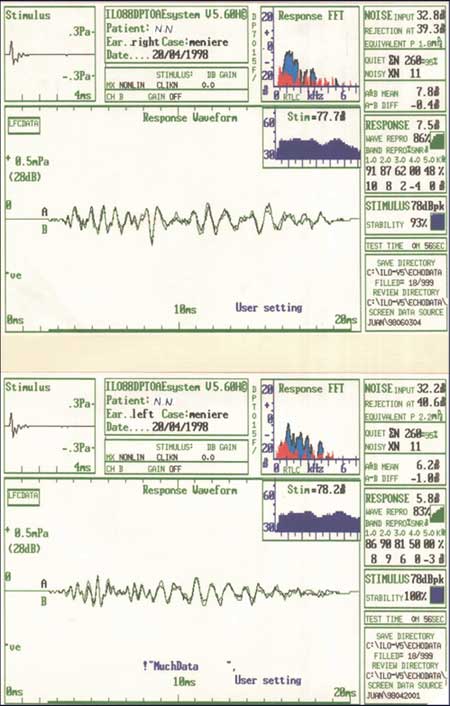
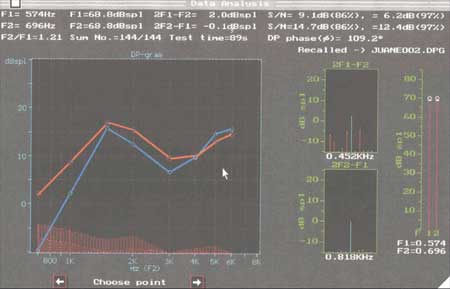
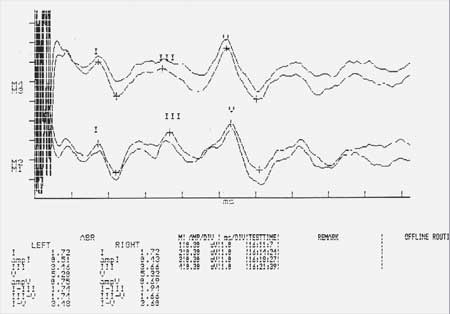
The patient is currently asymptomatic with normal auditory thresholds in pure tone audiometry (Figure 1B) and has not presented any new episodes, but the OAE on the left shows clear asymmetry when compared to the right ear (Figures 2 and 3), with abnormalities in low frequencies corresponding to those related to sensorineural fluctuation observed in pure tone audiometry. ABR on the right and left ears showed normal latency and amplitude (Figure 4).
In the case reported here, the patient is a physician and he refused to undergo many subsidiary tests that caused unpleasant symptoms, such as dizziness at electronystagmography or diarrhea in the glycerol test.
Figure 1 A. Pure tone audiometry conducted during the vertigo episode showing hearing loss in low frequencies with ascending curve on the left. Immitanciometry, acoustic stapedial reflex and speech recognition index were normal.
Figure 1 B. Pure tone audiometry conducted 10 days after the first one, under the same technical conditions, showing clinical improvement of vertigo and normal thresholds. The audiometry conducted after one year is exactly like this one.
Figure 2. TOAE on the right and left ears, showing low response in 7.5 dB on the right ear and 5.8 dB on the left ear. In the FFT, floor noise is shown in red and cochlear echo in blue.
Figure 3. DPOAE on the right (red) and left (blue), showing clear asymmetry in low frequencies and absence of response below 800 Hz, evidencing cochlear abnormalities in the frequencies that correspond to the auditory fluctuation recorded in pure tone audiometry.
Figure 4. Normal ABR tracing for both right and left ears.
COMMENTS
The diagnosis of this disease is essentially clinical, and the anamnesis is critical, together with the comprehensive ENT examination. A number of subsidiary tests can be ordered when there is suspicion of Meniere disease, but none can provide a definite diagnosis, so symptomatology set and the clinical evolution are the best way to follow the diseases (Lopes Filho, 1994).
The criteria for the diagnosis of Meniere disease, according to Harris and Probst (1992) are: idiopathic unilateral hearing loss observed in the audiometry, episodes of vertigo and tinnitus, without retrocochlear abnormalities in objective tests, no conductive abnormalities in the tympanometry or bone conduction tests, no neurological abnormalities both in the clinical history and in the physical and lab tests. These criteria are optimized by audiometry with ascending curve in low frequencies, reaching high frequencies as the disease progresses; transient or intermittent hearing loss shown by repetitive audiometry, worsening of hearing loss or tinnitus associated to exacerbation of dizziness; sensation of ear fullness on the affected ear or on both. Not all criteria are always present, but the association of two or more can reinforce the suspicion.
Patients with Meniere disease present symptoms related to the involvement of vestibular and auditory systems. Even though different theories have been proposed to explain the changes in sensitivity of the disease, the cochlear abnormalities responsible for them have not been fully defined yet. The cause and pathogenesis of Meniere disease are also controversial and not defined. Most of the times, the etiological agent of the disease is not identified and recent research studies have attributed the disease to inflammatory, multifactorial and immune-mediated mechanisms (Ruckenstein, 1999). Herpes simplex type I virus and enterovirus have been considered responsible for the triggering mechanism in the formation of this type of auto-immune response of the labyrinth (Ruckenstein, 1999). Food and inhalation allergy have also been largely commented as etiological factors of the disease and the treatment of such conditions can result in improvement of Meniere disease (Bryan, 1972).
The dominant theory in the studies of Meniere disease is that it is caused by the increase in pressure owing to accumulation of endolymph. This condition is experimentally caused in animals by the obstruction of the endolymphatic sac, which generally causes endolymphatic hydrops, with results similar to those found in humans. However, the underlying mechanisms to the sensitivity abnormalities detected experimentally have not been clearly defined yet (Harris and Probst, 1992).
Quick abnormalities of sensitivity in low frequencies are seen in the first days of hydrops in guinea pigs, with abnormal OAE thresholds in frequencies that correspond to those with reduced sensitivity. Provided that the hair cells are not destroyed during the first stages of the disease, the authors proposed that it happens as a result of the abnormality in the hydrodynamic and biomechanical micromechanisms that affect the transmission of the stimulus from the outer hair cells to the Corti's organ. It is likely that many factors are responsible for the complex mechanisms that cause hearing loss in Meniere disease. Even though it is known that increase in endolymphatic pressure acts directly and indirectly on the outer hair cells, it is still difficult to correlate the experimental findings in animals and symptoms found in human beings (Horner and Cazals, 1989).
A slight decrease in outer hair cells restricted to the apex region of the cochlea can be experimentally checked after approximately 2 months of hydrops and can not justify the auditory decrease that is observed. An anatomic pathologic picture that presents excellent correlation with hearing loss in low frequencies is selective atrophy of short and middle stereocilia in the region (Horner and Cazals, 1989).
The studied patient presented a clinical picture diagnosed as typical of Meniere disease at early stage, as experimentally described in guinea pigs, with fluctuating deafness in low frequencies on the left, as confirmed by pure tone audiometry, with recovery after 10 days. The tests were conducted again after one year (pure tone and speech reception) and they showed normal audiometry with air and bone thresholds at 30dB in 125Hz frequency, compared to the first test. The DPOAE showed reduced frequencies corresponding to the hearing fluctuation, probably caused by abnormalities of the hydrodynamic and biomechanical micromechanisms, as previously described by Horner and Cazals (1989), and normal ABR.
In the case of such patient, the abnormalities found in otoacoustic emissions on the left were not yet detectable in the pure tone audiometry and ABR, which can point to cochlear stereocilia abnormalities, without destruction of OHC in the apical region, as experimentally shown in guinea pigs.
An issue that still has to be addressed is: what protects the basal cochlear region from threshold abnormalities in initial hydrops when the apical spirals are affected? Trying to answer this question, Horner (1990) argued that pathologies of the upper portion of the cochlea can be favored by the largest size of the OHC stereocilia that increase progressively up to the apex. This abnormality can occur resulting from break of the interciliar bridges. The presence of hydrops in the endolymphatic space can force the basilar membrane downwards or the tectorial membrane upwards, introducing tension and breaking the interciliar bridges. A second mechanism that should be considered to explain these abnormalities is the efferent feedback mechanism that can control and protect selectively the basal spiral of the cochlea, where most medially crossed fibers end (Horner, 1990).
Despite the existence of various studies showing that the cochlea can be affected in the initial stage of Meniere disease without the affection of OHC in guinea pigs, it has not been correlated yet with sensitivity abnormalities found in human beings. It is probably owing to different facts, such as that the clinical diagnosis of Meniere disease is always polemical, the medical interventions vary from patient to patient, and that it is difficult to define the diagnosis in initial stages of the disease. This study is the first one to show Meniere disease documented in an initial stage in humans correlating experimental data and pure tone audiometry and OAE findings. A greater number of subjects have to be investigated to confirm such data in the future, because if it happens, OAE can become an extremely important test to follow up patients with endolymphatic hydrops.
The patient presented in this study had a clinical picture diagnosed as typical of Meniere disease with fluctuating hearing loss in low frequencies on the left, confirmed by pure tone audiometry, with remission after 10 days. Pure tone audiometry conducted one year later was normal. OAE was abnormal in the frequencies that corresponded to the hearing fluctuation observed on the left ear. According to experimental studies, these abnormalities are not related to loss of OHC in the cochlear apex, but the causes are not yet very clear and can be attributed to cochlear hydrodynamic and biomechanical micromechanisms, by interciliar bridge breakage owing to distension of membrane and cells inside the cochlear duct (Horner and Cazals, 1989).
REFERENCES
1. Bryan WTK, Bryan MP. Clinical examples of resolution of some idiopathic and other chronic disease by careful allergic management. Laryngoscope 1972;82:1231-1238.
2. Carnicelli MVF. O uso das emissões otoacústicas no diagnóstico e prevenção da perda auditiva induzida por ruído (PAIR). In: Nudelmann AA, Costa EA. Seligman J, Ibañez RN. PAIR. Porto Alegre (RS): Editora Bagagem Comunicação Ltda.; 1997. p. 237 245.
`3. Harris FP, Probst R. Transiently evoked emissions in patients with Ménière disease. Acta Otolaryngol (Stockh) 1992;112:36 44.
`4. Horner CK. Hypersensitivity of hydropic ears, at frequencies with normal thresholds, to temporary threshold shifts. Hearing Research 1990;48:281 286.
`5. Horner CK. Distortion products in early stage experimental hydrops in the guinea pig. Hearing Research 1989 (4 3):71 80.
`6. Isaac ML, Aquino AMCM. Audiometria Eletrofisiológica. In: Sih T. Otorrinolaringologia Pediátrica. Rio de Janeiro: Revinter; 1998. cap. 41 p. 214-216.
`7. Kenip DY, Bray P, Alexander L, Brown AM. Acoustic Emission Cochleography. Practical aspects. Scand Audiol Suppl 1986;25:71 95.
`8. Lopes Filho O et al. Tratado de Fonoaudiologia. São Paulo: Editora Roca; 1997. p. 222 237.
`9. Oliveira JAA. Fisiologia clínica da audição - cóclea ativa. In: Nudelmann AA, Costa EA, Seligman J, Raul NI. PAIR: Perda auditiva induzida por ruído. Porto Alegre (RS): Ed. Bagagem Com. Ltda.; 1997. p. 109 110.
10. Ruckenstein MJ. Immunologic aspects of Ménière disease. American Journal of Otolaryngology 1999;20(3):161-165.
1 Ph.D. in Otorhinolaryngology, Professor at University of Franca and University of Ribeirão Preto.
2 Speech and Language Pathologist and Audiologist, specialized in Audiology.
3 Speech and Language Pathologist and Audiologist, specialized in Audiology.
4 Master in Otorhinolaryngology.
5 Faculty Professor, Department of Otorhinolaryngology and Ophthalmology, Hospital das Clinicas, Medical School of Ribeirão Preto - USP.
Address correspondence to: Av. Itatiaia, 639 - Alto da Boa Vista
Ribeirão Preto SP 14025-170 - Tel. (55 16) 623-7651 - E-mail: amclaret@usp.br
Article submitted on July 17, 2001. Article accepted on August 15, 2001