Year: 2002 Vol. 68 Ed. 5 - (22º)
Relato de Caso
Pages: 744 to 748
Sigmoid and transverse sinus' phlebitis & Bezold's mastoiditis: case report and literature review
Author(s):
Sérgio Bittencourt 1,
Ulisses J. Ribeiro 1,
Paulo A. S. Vichi Jr. 2,
Fabrícia D. Colombano 2,
Lys M. A. Gondim 2,
Elaine M. Watanabe 2
Keywords: Bezold's mastoiditis, sigmoid sinus' phlebitis, transverse sinus' phlebitis, otitis media's complications
Abstract:
Aim: to describe two rare complications of acute otitis media inadequately treated. Method: description of a case of two simultaneous complications of acute otitis media in a 12-year-old boy and a posterior literature review of the theme. Results: a 12-year-old white boy was referred to our ENT Department presenting 'otitis' for two months without improvement with the clinical treatment and evolving to a right cervical mass. At the clinic examination the otoscopic findings were a thickened and opaque tympanic membrane with a discreet increase on its vascularization. The radiologic exams showed an inflammatory/infectious process involving the mastoid region, with multiple abscesses aspect extending extra-cranially to the right cervical area and presence of suggestive alterations of phlebitis in the transverse and sigmoid right sinus. After surgical procedure and parenteral antibiotic therapy, the patient had a good evolution, with a low morbidity. Conclusions: despite the low incidence of the acute otitis media complications, due to the evolution and high spectrum of the antibiotic therapy, we must not forget they still exist.
![]()
INTRODUCTION
Otitis media is one of the most prevalent infections. As a result of broad-spectrum antibiotic therapy, its approach has been modified from mainly surgical treatment to clinical treatment. The incidence of complications has decreased a lot and it is currently infrequent1, 2, 3. In the pre-antibiotic era, intracranial complications were noticed in 2.3% of the cases and extracranial ones in 0.45% of them4, and they were drastically reduced to 0.15 - 0.04%, respectively, after the introduction of antibiotics. Despite the reduction in incidence and in absolute number of complications, distribution and frequency remain similar to pre-antibiotic days.
Complications of middle ear infectious processes are basically due to an extension of the infection into other regions of the temporal bone (mastoid, petrous region) and to the skull (meninges, meningeal space, parenchyma) by contiguity and, less frequently, by hematogenic access. Out of the predisposing factors, there are: experience of the physician, change in virulence, and susceptibility to bacteria, general status of the patient, development of imaging diagnostic techniques, clinical pictures masked by previous inappropriate antibiotic therapy, leading to late diagnosis of affections and reduction of temporal bone pneumatization.
Both acute otitis media (AOM) and chronic otitis media can lead to such complications, as follows: acute mastoiditis, Bezold's mastoiditis, chronic mastoiditis, petrositis, labyrinthitis, facial palsy, labyrinthic fistula, extra and subdural, cerebral and cerebellum abscesses, otitic hydrocephalus, meningitis, which is the most common affection, followed by sigmoid thrombophlebitis.
In the present study, the authors reported a case of AOM inappropriately treated in a child that presented simultaneously intracranial complications (transversal and right sigmoid sinuses phlebitis) and extracranial complications (Bezold's mastoiditis) and reviewed the literature about the topic.
CASE REPORT
HMP, 12-year-old, male Caucasian, born in Sao Paulo, presented in January 2001 a complaint of earache on the right and fever (39o C), after water had been trapped in his ears, diagnosed by an otorhinolaryngologists in another unit as having AOM and medicated with Amoxicillin. On the same day, he experienced severe otalgia and the mother went to another ENT unit, and there, after the examination, the child was prescribed a new medication - Cefalexin (seven days) and nasal drops.
At the beginning of February 2001, the patient still reported pain on the right, had no fever and reported retroauricular and neck pain on the right, hearing loss and headache. The patient was treated with non-steroidal antiinflammatory drugs (NSAID) and after the treatment, there was still retroauricular pain and trismus.
On 18/02/01, a new assessment was conducted by another ENT service that noticed hyperemia of external acoustic canal and thickened right tympanic membrane and the physician conducted in the examination room Cephalotin, tenoxican and hydrocortisone succinate. There was no clinical improvement and the child was hospitalized and an examination from the service of oral-maxillo surgery was requested owing to suspicion of temporomandibular joint disorders as diagnostic hypothesis. The patient was transferred to the hospital of his medical care plan and was discharged the next day, with prescription of NSAID and analgesic, since otoscopy was normal.
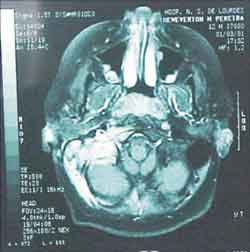
One week later, there was right neck bulging. He went again to the same ENT service on 25/02/01 and hospitalization for further assessment was requested. Complete blood count was ordered, resulting in mild leukocytosis, no deviation to the left, and Computed tomography (CT scan) of the head and neck (without contrast) showed signs of osteomastoid pathology on the right (inflammatory?), suggesting the correlation with temporal bone CT scan (Figure 1). Temporal bone and neck CT scans showed a lesion of mixed aspect, on the skull base and right deep neck region (abscess? other etiology?). (Figures 2 and 3). The possibility of meningeal extension was not ruled out, added by the signs of otomastoid pathology on the right.
Later, audiometry was conducted and the result was moderate conductive hearing loss on the right (gap of 30dB) and impedanciometry resulted in curve type B on the right, with bilateral absent reflexes.
The otorhinolaryngologist at the hospital suggested the conduction of a magnetic resonance imaging (MRI) in our hospital (Hospital Nossa Senhora de Lourdes) to reassess. Our radiological team sent the patient to the ENT team to reassess the mastoid MRI, which showed presence of inflammatory/infectious process, involving the region of the right mastoid, extending extracranially to the neck region (figure 4 and 5) and venous angiography that showed absence of flow inside the right transverse and sigmoid sinuses, which presented marked enhancement to contract suggesting phlebitis (Figures 6 and 7). We did not observe abnormalities indicative of extension of the process into the pericerebellar or pericerebral space.
The patient was hospitalized in our unit with right retroauricular pain, bulging and pain on the lateral and posterior right neck region, no fever, good general status, normal breathing and color. At otoscopy, TM was thickened and opacified on the right, with mild increase in vascularization and normal fundus exam. We diagnosed Bezold's mastoiditis and right sigmoid and transversal sinuses phlebitis.
Owing to the intra and extracranial complications, we decided to use Ceftriaxone and Clyndamicin and planed mastoidectomy on the right ear. During surgery, we detected the presence of abundant granulation tissue on the mastoid cortex and presence of fistula on the tip of the mastoid, through where a large amount of purulent exsudate was drained, especially by compression of the neck bulging. We also found a large amount of secretion on the middle ear, and we decided for tympanotomy with ventilation tube on the right. We aspirated 50ml of exsudate sent to bacteriological study. The abscess site was left with a Penrose drain.
As to early postoperative condition, the patient progressed with marked dizziness and nausea, and we prescribed Pentoxiphillin and Dimenidrate, Vitamin B6, Glucose, D-fructose. On the second postoperative visit, the patient had no dizziness and there was absence of secretion in the drain. He had no neurological complications and absence of secretion in the drain; we removed the drain and the patient was discharged on the third postoperative visit, with IM Ceftriaxone and PO Clyndamicin. One week later, the patient came back to the outpatient unit with no symptoms, and we conducted temporal bone CT scan (Fig. 8 and 9), which showed signs of partial mastoidectomy, with bone continuity communication with the region of the sigmoid sinus. There was hypodense content inside the tympanic complex, involving the ossicle chain. Compared to the previous exam, there was absence of collection.
Currently, the patient is being followed up in the ambulatory, with no apparent signs of process recurrence and normal audiometry.
Figure 1. Head CT scan (axial section).
Figure 2. Temporal bone CT scan (coronal section).
Figure 3. Temporal bone CT scan (axial section).
Figure 4. MRI (coronal section).
Figure 5. MRI (axial section).
Figure 6. Venous angiography.
Figure 7. Venous angiography.
Figure 8. Temporal bone CT scan - axial section (postoperative).
Figure 9. Temporal bone CT scan - axial section (postoperative).
DISCUSSION
Sigmoid sinus thrombophlebitis is an inflammatory process around the sigmoid sinus, at the extradural space, which ends up stimulating the formation of the thrombus, being the second most common intracranial complication. The patient can be asymptomatic or, if there is spread to the internal jugular vein and jugular bulb, it leads to jugular foramen syndrome, resulting in intracranial hypertension. The association of sigmoid thrombophlebitis and extradural abscess is common. Mortality by thrombosis of the sigmoid sinus, owing to ear infection, at the antibiotic era ranged from 2 to 3%, followed by significant improvement with the advent and development of surgical approaches.
As to extracranial complications, as presented by this patient, Bezold's abscess was described in 1908 by Friedrich Von Bezold, a Dutch ophthalmologist5.
Bezold's abscess is a complication of otitis media, defined as spread and exteriorization of the middle ear infectious process, through fistulization of the mastoid tip, forming a subsequent neck purulent collection to the sternocleidomastoid muscle. If the purulent collection moves towards the internal aspect of the sternocleidomastoid muscle, it may result in anterior mediastinitis 1.
At the beginning of the 20th century, 50% of all cases of AOM progressed to mastoiditis. By 1959, this incidence had already fallen to 0.4% and fortunately today it affects only 0.24 -0.36 % of the cases1, 6. From 1988 to 1998, only 20 cases of lateral cervical abscesses were reported in the world literature, including immunosuppressed patients and Mouret's abscesses (jugal-digastric).
The diagnosis should be based on clinical history and physical examination and many times the duration of the symptoms ends up being an important factor for the severity of the clinical presentation. There are some oligosymptomatic cases at times, apparently with no severity and indolent. The cases may be considered "masked", especially owing to no previous treatment or inappropriate use of antibiotics.
As to microbiology, they can be caused by the same microorganisms responsible for the OM (Streptococcus pneumoniae and Haemophilus influenzae). In subacute and chronic cases, we should consider Staphylococcus aureus and gram-negative bacteria (Escherichia coli, Proteus sp, Pseudomonas aeruginosa), keeping in mind that immunosuppressed patients can have as possible agents also Mycobacterium avium, Fusobacterium, and others1,3,5,7.
Complementary tests, therefore, are not complementary in fact but rather indispensable for the diagnosis (determining exact location and real extension of the process) and therapeutic planning.
CT with contrast can strongly suggest the diagnosis. A characteristic finding is the presence of Delta sign (caused by the inflammation of soft tissues adjacent to the dura mater that recovers the lateral sinus, soaked in contrast). Angiography of the venous phase, MRI and angiography with digital subtraction are the most sensitive tests for the diagnosis3.
At bacterioscopy, we identified moderate gram positive and abundant leukocytes. The culture and the yeast test were negative. The results obtained were probably due to the previous use of antibiotics1.
Among the predisposing factors to infections, we found in our patient a little pneumatized mastoid, which stresses the information in the literature8.
As to treatment, broad-spectrum antimicrobial therapy and with good penetration of the blood-brain barrier should be chosen. Indication of immediate surgical drainage, mastoidectomy and posterior CT scan follow-up are mandatory. Taking into account that in 1938 the number of mastoidectomies performed owing to mastoiditis and its complications was of 20%, it decreased to about 2.8% in 1948, reducing mortality to 90% during this period.
CLOSING REMARKS
Despite the rare occurrence, it is important to bear in mind that these complications are still present in our routine, especially because the absolute number of mastoiditis cases, as mentioned, has decreased, but the proportion of Bezold's abscesses present in the cases has increased (from 20% at Bezold's time to 50% currently). It is due to frequently late diagnosis, most of the time owing to masking consequent from previous antibiotic therapy and absence of symptoms and/or otoscopy abnormalities.
Extracranial complications are more common than intracranial ones, but the latter remain as an important cause of mortality from otitis media2, 8.
In cases of suspicion of otogenic complications, radiological tests become essential and surgical treatment should be conducted as quickly as possible.
REFERENCES
1. Gaffney RJ, O'Dwyer TP, Maguirre AJ. Bezold's abscess. The Journal of Laryngology and Otology 1991;105:765-66.
2. Kangsanarak J, Fooanant S, Ruckphaopunt K, Navacharoen N, Teotrakul S. Extracranial and intracranial complications of supurative otitis media. Report of 102 cases. The Journal of Laryngology and Otology 1993;107:999-1004.
3. Saffer M, Lubianca JFN, Arrarte JLF, Brinckmann CA, Ferreira P. Tromboflebite do seio lateral e abscesso cervical como complicação de otite média crônica. Jornal de Pediatria 1997;74(4):269-72.
4. Spiegel JH, Lusting LR, Lee KC, Murr AH, Schindler RA. Contemporary Presentation and Management of a Spectrum of Mastoid Abscesses. Laryngoscope 1998;108:822-28.
5. Pappas DG. Friedrich Von Bezold (1842-1908) - ENT-Ear, Nose & Throat Journal 1996;75:74-75.
6. Gower D, Mcguirt WF. Intracranial complications of acute and chronic infectious ear disease: a problem still among us. Laryngoscope 1993;93:1028-33.
7. Nadal D, Herrmann P, Baumann A, Fanconi A. Acute mastoiditis: clinical, microbiological, and therapeutic aspects. Ear J Pediatr 1990;149:560-64.
8. Kangsanarak J, Navacharoen N, Fooanant S, Ruckphaopunt K. Intracranial complications of supurative otitis media: 13 years experience. The American Journal of Otology 1995;16:104-09.
9. Monday LA. A propos d'une observation d'abcés de Bezold. L'union Médicale du Canada 1979;108:55-58.
10. Smouha EE, Levenson MJ, Anand VK, Parisier SC. Modern Presentation of Bezold's abscess. Arch Otolaryngol Head Neck Surg 1989;115:1126-29.
1 Head of the Service of Otorhinolaryngology, Hospital Nossa Senhora de Lourdes.
2 Resident Physician, Service of Otorhinolaryngology, Hospital Nossa Senhora de Lourdes.
Address correspondence to: Hospital Nossa Senhora de Lourdes
Rua das Perobas, 344 04321-120 São Paulo - SP - Tel. (55 11) 5018-4730 - Fax: (55 11) 5011-0206 - E-mail: cehnsl@uol.com.br
Article submitted on December 04, 2001. Article accepted on March 14, 2002