Year: 2014 Vol. 80 Ed. 2 - (16º)
Relato de Caso
Pages: 178 to 179
Keratocystic odontogenic tumor in the maxillary sinus: a rare occurrence
Author(s): Marcelo Bonifácio da Silva Sampieri1; Eduardo Sanches Gonçales1; Victor Tieghi Neto1; Alexandre Simões Nogueira2; Eveline Turatti3; Roberta Barroso Cavalcante3; Virgílio Mendes Maia Júnior4
DOI: 10.5935/1808-8694.20140035
![]()
INTRODUCTION
In 2005, the World Health Organization revised and updated the classification of odontogenic tumor, and some terminologies were modified. Due to its neoplastic nature, the odontogenic keratocyst, which was previously classified as a cyst, had its name changed to keratocystic odontogenic tumor (KCOT). The prevalence of KCOT in the maxillary sinus is only 1%.1 KCOT has high rate of recurrence,2 and numerous surgical modalities such as marsupialization, saucerization, Carnoy's solution, and enucleation have been used for the treatment of KCOT with different results.3 This article reports a case of KCOT in maxillary sinus treated with descompression and enucleation.
CASE PRESENTATION
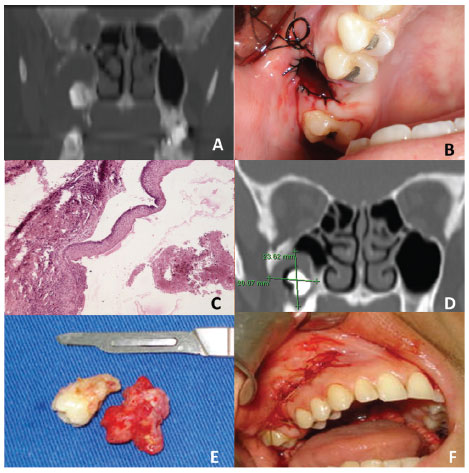
A 28-year-old woman was referred for evaluation of an infection in the first upper molar area, which had been extracted 30 days before. Extraoral examination showed pus drainage through the right nasal fossa. Intraoral examination revealed no swelling, but the area corresponding to the upper right first molar was also draining pus. In the coronal view of computed tomography, it was possible to observe an obstruction of the right maxillary sinus by a lesion of cystic aspect associated with a molar tooth. The bone walls were preserved (Fig. 1A). After remission of the acute phase of the infection with the use of a systemic antibiotic, an incision with the removal of the buccal mucosa was performed in order to decompress the lesion under local anesthesia (Fig. 1B). At the same time, the intra-lesional material was removed for analysis. The histopathologic diagnosis was compatible with KCOT. The histological sections presented fragments of cystic capsule coated in focal area by stratified squamous epithelium in continuity with parakeratinized rather than stratified epithelium (Fig. 1C).
Figure 1 A, Coronal view of computed tomography showing the obstruction of the right maxillary sinus by a lesion of cystic aspect associated with a molar tooth. B, Decompression of the lesion under local anesthesia. C, Coating epithelium parakeratinized H&E with 100 × magnification. D, Coronal view at 18 months postoperative. E, Removal of cyst and the associated tooth. F, Primary closure of wound
The patient had no complications in the postoperative period. Monthly follow-ups were performed for irrigation and cleaning of the surgical cavity. After 18 months postoperative, a coronal view of computed tomography showed a considerable regression in the size of the lesion (Fig. 1D). The removal the of cyst and the associated tooth was performed under general anesthesia (Fig. 1E), and primary closure of the wound was attained (Fig. 1F). No signs of recurrence have been observed in three years of follow-up.
DISCUSSION
KCOT is a pathological entity that requires special attention due to its aggressive behavior and high rate of recurrence. The presence of multiple KCOT can be associated with Gorlin-Goltz syndrome.4 An important radiographic feature is the buccolingual growth without cortical expansion in nonsyndromic cases.5
Six treatment modalities were described: resection; enucleation with peripheral ostectomy and Carnoy's solution; enucleation with peripheral ostectomy; enucleation; decompression; and enucleation with Carnoy's solution. The rate of recurrence ranged from 0% to 50%, with an average of 23.15%.3
Few occurrences of KCOT in the maxillary sinus have been described, and the treatment consists of total lesion removal and bone curettage.2,4,6 The previously mentioned peripheral ostectomy included additional removal of bone tissue; the execution of this procedure in this case report would not be possible due to the thinness of the maxillary sinus walls. In the present case, decompression was chosen in order to preserve the surrounding anatomical structures (orbital cavity, maxillary sinus, nasal cavity, and teeth) and avoid a more aggressive surgery. Later, a total lesion enucleation was performed, followed by bone curettage. The lesion capsule presented as less friable than the first surgical intervention, facilitating total removal of the KCOT.
FINAL REMARKS
KCOT has a specific course and high rates of recurrence. Its occurrence in the maxillary sinus is rare, and computed tomography is essential to determine the lesion extensions and establish the treatment plan. Follow-up must be continued for at least for five years, and must be based on clinical and radiographic signs.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
REFERENCES
1. Press SG. Odontogenic tumors of the maxillary sinus. Curr Opin Otolaryngol Head Neck Surg. 2008;16:47-54.
2. Vencio EF, Mota A, Pinho CM, Dias Filho AA. Odontogenic keratocyst in maxillary sinus with invasive behavior. J Oral Pathol Med. 2006;35:249-51.
3. Kaczmarzyk T, Mojsa I, Stypulkowska J. A systematic review of the recurrence rate for keratocystic odontogenic tumour in relation to treatment modalities. Int J Oral Maxillofac Surg. 2012;41:756-67.
4. Silva GCC, Silva EC, Gomez RS, Vieira TC. Odontogenic keratocyst in the maxillary sinus: Report of two cases. Oral Oncol EXTRA. 2006;42:231-4.
5. MacDonald-Jankowski DS. Keratocystic odontogenic tumour: systematic review. Dentomaxillofac Radiol. 2011;40:1-23.
6. Çakur B, Miloglu Ö, Yolcu Ü, Göregen M, Gürsan N. Keratocystic odontogenic tumor invading the right maxillary sinus: a case report. J Oral Scien. 2008;50:345-9.
1. Bauru Dentistry School, Universidade de São Paulo (FOB-USP), Bauru, SP, Brazil
2. Dentistry School, Universidade Federal do Ceará (UFC), Sobral, CE, Brazil
3. Dentistry School, Universidade de Fortaleza (UNIFOR), Fortaleza, CE, Brazil
4. Private Practice, Granja, CE, Brazil
Corresponding author.
M.B.S. Sampieri
E-mail: mar_sampieri@hotmail.com
Received 17 July 2012.
Accepted 15 December 2012.
All rights reserved - 1933 /
2026
© - Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico Facial