Year: 2014 Vol. 80 Ed. 2 - (12º)
Artigo Original
Pages: 152 to 155
Peripheral Th17/Treg cell-mediated immunity imbalance in allergic rhinitis patients*
Author(s): Xuekun Huang1; Yulian Chen1; Fucheng Zhang2; Qintai Yang1; Gehua Zhang1
DOI: 10.5935/1808-8694.20140031
Keywords: Rhinitis allergic, seasonal; Th17 cells; T-lymphocytes, regulatory
Abstract:
INTRODUCTION: Allergic rhinitis (AR) is an IgE-mediated non-infectious disease of the nasal mucosa following contact with allergens.
OBJECTIVE: To investigate the peripheral Th17 cells and CD4 + CD25 + Foxp3 + regulatory T (Treg) cells and the expression of cytokines in the serum of AR patients.
METHODS: The peripheral blood of 14 patients with AR (AR group) and six healthy subjects (control group) was collected from March to May of 2012. Flow cytometry was performed to detect the Th17 cells and Treg cells, and enzyme-linked immunosorbent assay (ELISA) to measure the serum levels of IL-17 and TGF-β1.
RESULTS: The proportion of Th17 cells in the AR group was markedly higher than that in the control group (p < 0.01). The proportion of Treg cells in the AR group was also dramatically reduced when compared with the control group (p < 0.01). In the AR group, serum IL-17 levels were markedly higher than those in the control group (p < 0.01). In the AR group, serum TGF-β1 levels were significantly lower than those in the control group (p < 0.01).
CONCLUSION: The imbalance of peripheral Th17/Treg cells plays an important role in the pathogenesis of AR.
![]()
INTRODUCTION
Allergic rhinitis (AR) is an IgE-mediated non-infectious disease of the nasal mucosa following contact with allergens.1 Previous studies have demonstrated that imbalance of Th1/Th2 cell-mediated immunity has an important role in the pathogenesis of AR, which is characterized by Th2 cell-mediated inflammation.2 In recent years, there is evidence showing that regulatory T (Treg) cells are another subset of T lymphocytes involved in allergic diseases and can regulate the pathological and physiological immune response, which may promote self-immune tolerance and maintenance of immune balance.3 CD4+CD25+ Treg cells are the major type of Treg cells; they can secret some cytokines, including TGF-β1 and IL-10. Forkhead box p3 (Foxp3) gene is a critical regulatory gene in the development and functional maintenance of CD4+CD25+ Treg cells.4
Th17 cells are a subset of T lymphocytes that play crucial roles in pro-inflammatory inflammation and autoimmune diseases. RORγt is a key nuclear transcription factor of Th17 cells, and IL-17 is an important effector cytokine secreted by these cells. IL-17 can exert a pro-inflammatory effect, promote the production of chemokines (such as IL-8 and monocyte chemoattractant protein-1, among others) in the local tissues, facilitate the proliferation of monocytes and neutrophils, and stimulate the generation of IL-6 and prostaglandin E2, resulting in local inflammation.5,6 Some researchers, using real-time polymerase chain reaction (RT-PCR) and enzyme-linked immunosorbent assay (ELISA) for the detection of associated transcription factors and cytokines of Th17 and Treg cells in the peripheral blood of AR patients, observed that the expression of RORγt and IL-17 increased and the expression of Foxp3 (transcription factor of Treg cells) and TGF-β1 (associated cytokine) decreased.7 In the present study, flow cytometry (FCM) and ELISA were employed to detect the Th17/Treg cells and serum levels of IL-17 and TGF-β1, respectively, aiming to explore the role of Th17/Treg cells in the pathogenesis of AR.
MATERIALS AND METHODS
Subjects
From March to May of 2012, a total 14 patients with AR were admitted into this department: five males and nine females, with a mean age of 29.76 years. The diagnosis of AR was made according to its diagnostic criteria.1 Skin- prick test results were positive for dust mite; the severity of AR was moderate or severe in all 14 patients. These patients had not been treated with glucocorticoids in the past month and had not received anti-histamine therapy and allergen-specific immunotherapy. Patients with sinusitis, asthma, and intolerance to acetylsalicylic acid were excluded. Additionally, six healthy volunteers without symptoms of AR were recruited as controls: two males and four females, with a mean age of 30.83 years. All subjects signed an informed consent prior to their enrollment in the study.
Main reagents and instrument
Flow cytometer (FACSCalibur; BD - USA) was used for detection and Cellquest software (BD - USA) was employed for the acquisition of data and subsequent analysis. Microplate reader (ELX-800; Bio-Tek - USA), PMA, ionomycin calcium, BFA (MultiSciences), Human Regulatory T Cell Staining Kit (eBioscience - USA), APC-conjugated human CD8 mAb (BD - USA), PerCP-Cy5.5 conjugated human CD3 mAb, PE-conjugated human IL-17 mAb and corresponding istype control (eBioscience - USA), fixation solution and membrane rupture solution (Invitrogen - USA), anti-human IL-17 ELISA kit (eBioscience - USA), and TGF-β1 ELISA kit (RayBio - USA) were used in the present study.
Sample collection
In the morning, venous blood samples (4 mL) were collected from the ulnar vein and anti-coagulated with heparin. Then, 2 mL of blood were subjected to centrifugation at 3,000 rpm for 15; the serum was collected and stored at -20ºC for the detection of IL-17 and TGF-β1. In addition, the remaining 2 mL of blood were used for flow cytometry for the detection of Th17 cells and Treg cells.
Detection of Th17 cells by FCM
In brief, 250 µL of peripheral blood were mixed with 50 µg/L PMA, 2.0 µmol/L monensin, and 750 µmoL/L ionomycin calcium, followed by incubation at 37ºC in an environment with 50 mL/L CO2 for 4 h. The cell suspension was transferred into a 1.5 ml-PE tube followed by centrifugation at 2,500 rpm for 6 min. The supernatant was removed, and the cells were washed with PBS twice for FCM. The cells were treated with 10 µL of PECy5-CD3Ab and 10 µL of FITC-CD8Ab at room temperature, in a dark environment, for 30 min. After washing in PBS twice, the cells were fixed in 300 µL of fixation solution in a dark environment at 4ºC for 15 min. After centrifugation, the supernatant was removed. Following the addition of membrane rupture solution, centrifugation was performed at 3,000 rpm and the supernatant was removed. After washing in PBS twice, cells were transferred into two tubes and treated with 20 µL of PE-IL-17Ab and 10 µL of isotype control PE-IgG1, respectively, in a dark environment at room temperature for 30 min. After washing in PBS twice, cells were re-suspended in 0.3 mL of PBS and subjected to FCM. CellQuest software was employed for data analysis.
Detection of Treg cells by FCM
Cells were transferred into sample tube and control tube. Cells in the sample tube were treated with CD4/CD25/Foxp3, and those in the control group were treated with Foxp3 isotype control (CD4/CD25/mouse IgG). Then, 100 µL of anti-coagulated blood was added followed by incubation in a dark environment at room temperature for 20 min. Following the addition of 1 mL of hemolytic agent, incubation was performed at room temperature in a dark environment for 10 min followed by centrifugation at 1,000 rpm for 5 min. The supernatant was removed and cells were re-suspended in 1 mL of PBS followed by centrifugation at 1,000 rpm for 5 min. The supernatant was then removed, and 0.5 mL of Foxp3 fixation solution were added, followed by incubation in a dark environment at room temperature for 20 min. Cells were re-suspended in 1 mL of PBS, and centrifuged at 1,000 rpm for 5 min. The supernatant was removed, and 0.5 mL of Foxp3 membrane rupture solution was added to each tube, followed by centrifugation at 1,000 rpm for 5 min. These cells were re-suspended in 0.5 mL of Foxp3 membrane rupture solution, followed by incubation in a dark environment at room temperature for 15 min. After centrifugation at 1,000 rpm for 5 min, the supernatant was removed. Then, 10 µL of PE Foxp3Ab were added to the sample tube and 10 µL of isotype control were added to the control tube, followed by incubation at room temperature in a dark environment for 30 min. Cells were re-suspended in 1 mL of PBS and centrifuged at 1,000 rpm for 5 min. The supernatant was removed and the cells were re-suspended in 0.4 mL of PBS. FCM was performed and CellQuest software was employed for data analysis.
Detection of serum IL-17 and TGF-β1 by ELISA
The detection of serum contents of IL-17 and TGF-β1 was performed according to the manufacturer's instructions. The lower limit of detection was 0.5 pg/mL for IL-17 and 9 pg/mL for TGF-β1.
Statistical analysis
Statistical analysis was performed with SPSS version 16.0. Data with normal distribution were expressed as mean ± standard deviation. Student's t-test for independent variables was performed for comparisons between two groups. A value of p < 0.05 was considered statistically significant.
RESULTS
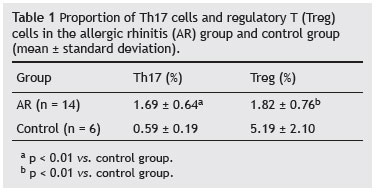
Proportion of Th17 cells in AR group and control group
FCM demonstrated that the proportion of Th17 cells in the AR group was markedly higher than that of the control group (p < 0.01; Table 1).
Proportion of Treg cells in AR group and control group
In the AR group, the proportion of Treg cells was markedly reduced when compared to the control group (p < 0.01; Table 1).
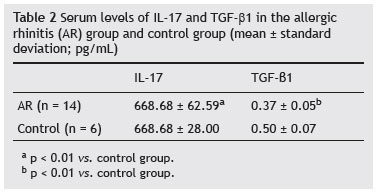
Serum contents of IL-17 and TGFβ1 in AR group and control group
ELISA was performed to detect the serum contents of IL-17 and TGF-β1 in the AR group and control group. Data are shown in Table 2. Results demonstrated that the IL-17 level in the AR group was markedly higher than that of the control group (p < 0.01). In the AR group, the TGF-β1 level was dramatically reduced when compared with the control group (p < 0.01).
DISCUSSION
Previous studies have demonstrated that the serum level of IL-17 in AR patients was significantly increased when compared with controls,8 and that the proportion of IL-17 positive cells in the nasal mucosa in AR patients was also markedly higher than that in healthy subjects.9 Ciprandi et al.10,11 observed that the serum IL-17 level was positively related to the severity of symptoms of AR and positively associated with the number of peripheral eosinophils. The peripheral monocytes from AR patients who were treated with pollen allergen and FCM showed the proportion of Th17 cells was markedly higher than that in the control group. In the present study, the results indicated that the proportion of peripheral Th17 cells in AR patients was significantly higher than that of the controls, accompanied by the increase in serum level of IL-17. These findings suggest that Th17 cells can secret a large amount of IL-17, which is involved in the pathogenesis of AR.
Additionally, the proportion of CD4 + CD25 + Treg cells in peripheral blood of AR patients was significantly lower than that of the controls, accompanied by the reduction of serum TGF-β1 level. This suggests that the reduction of peripheral Treg cell count leads to a compromised function of these cells. In healthy subjects, the proportion of CD4 + CD25 + Treg cells was approximately 5% to 10% in the peripheral blood. The CD4 + CD25 + Treg cells can exert inhibitory effect on the immune response via the intercellular interaction or secretion of inhibitory cytokines (such as IL-10 and TGF-β).4 The present results demonstrated that the proportion of peripheral CD4 + CD25 + Treg cells and the serum level of TGF-β1 were reduced. Xu et al.12 confirmed that the Foxp3 + positive lymphocytes and Foxp3 mRNA expression in the nasal mucosa and peripheral monocytes of AR patients were markedly reduced when compared with healthy controls, and that Foxp3 and CD4 + CD25 + Treg cells in allergy patients were markedly reduced.13 This suggests that the compromised inhibitory effect of Treg cells leads to the occurrence of allergic diseases.
Th17 cells and Treg cells are derived from naïve T cells. Th17 cells mediate the inflammatory reaction, whereas Treg cells mediate immune tolerance. There is antagonism in the function and differentiation of Th17 cells and Treg cells. Thus, the balance of Treg cells and Th17 cells is crucial for the maintenance of the immune status. In the present study, the results demonstrated that the proportion of Th17 cells in the peripheral blood of AR patients was markedly increased and that of Treg cells was dramatically reduced. This suggests that Th17/Treg imbalance plays an important role in the pathogenesis of AR. Further research in the Th17/Treg balance may provide a novel strategy for the treatment of AR.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
REFERENCES
1. Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, et al. Allergic rhinitis and its impact on asthma (ARIA) 2008 Update (in collaboration with the World Health Organization, GA2LEN and AllerGen). Allergy. 2008;63(Suppl 86):8-160.
2. Agrawal DK, Shao Z. Pathogenesis of allergic airway inflammation. Curr Allergy Asthma Rep. 2010;10:39-48.
3. Ozdemir C, Akdis M, Akdis CA. T regulatory cells and their counterparts-masters of immune regulation. Clin Exp Allergy. 2009;39:626-39.
4. Pai SY, Truitt ML, Ting CN, Leiden JM, Glimcher LH, Ho IC. Critical roles for transcription factorGATA-3 in thymocyte development. Immunity. 2003;19:863-75.
5. Harrington LE, Hatton RD, Mangan PR, Turner H, Murphy TL, Murphy KM, et al. Interleukin 17-producing CD4+ effector T cells develop via a lineage distinct from the T helper type 1 and 2 lineages. Nat Immunol. 2005;6:1123-32.
6. Ivanov II, McKenzie BS, Zhou L, Tadokoro CE, Lepelley A, Lafaille JJ, et al. The orphan nuclear receptor RORgammat directs the differentiation program of proinflammatory IL-17+ T helper cells. Cell. 2006;126:1121-33.
7. Zhang C, Hong S, Hu G. The expression of Treg/Th17 cells related transcription factors and cytokines in PBMCs and plasma in patients with allergic rhinitis. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2012;26:209-11.
8. Huang X, Yang Q, Chen Y, Zhang GH, Li Y. Expressions of IL-17, IL-21 and IL-23 in the serum of allergic rhinitis patients. J Med Biochem. 2011;30:323-7.
9. Ba L, Du J, Liu Y, Shang T, Yang F, Bian P. The expression and significance of interleukin-17 and the infiltrating eosinophils in nasal polyps. J Clin Otorhino Laryngol Head Neck Surg. 2010;24:53-6.
10. Ciprandi G, De Amici M, Murdaca G, Fenoglio D, Ricciardolo F, Marseglia G, et al. Serum interleukin-17 levels are related to clinical severity in allergic rhinitis. Allergy. 2009;64:1375-8.
11. Ciprandi G, Filaci G, Battaglia F, Fenoglio D. Peripheral Th- 17 cells in allergic rhinitis: New evidence. Int Immuno Pharmacol. 2010;10:226-9.
12. Xu G, Mou Z, Jiang H, Cheng L, Shi J, Xu R, et al. A possible role of CD4+CD25+ T cells as well as transcription factor Foxp3 in the dysregulation of allergic rhinitis. Laryngoscope. 2007;117:876-80.
13. Larché M. Regulatory T cells in allergy and asthma. Chest. 2007;132:1007-14.
1. Department of Otolaryngology, Third Hospital, Sun Yat-sen University, Guangdong, China
2. Central Laboratory, Third Hospital of Sun Yat-sen University, Guangdong, China
Corresponding author.
Q. Yang
E-mail: yang32432423@sohu.com
Received 8 July 2013.
Accepted 10 November 2013.
* Study conducted at Third Hospital, Sun Yat-sen University, Guangdong, China.