Year: 2014 Vol. 80 Ed. 2 - (8º)
Artigo Original
Pages: 126 to 130
Adherence of obstructive sleep apnea syndrome patients to continuous positive airway pressure in a public service*
Author(s): Danielle L.C. Queiroz; Mariane S. Yui; Andréa A. Braga; Mariana L. Coelho; Daniel S. Küpper; Heidi H. Sander; Leila A. Almeida; Regina M.F. Fernandes; Alan L. Eckeli; Fabiana Cardoso Pereira Valera
DOI: 10.5935/1808-8694.20140027
Keywords: Continuous positive airway pressure; Obstructive sleep apnea; Sleep medicine; Sleep disorders
Abstract:
INTRODUCTION: The standard therapy for obstructive sleep apnea syndrome (OSAS) is continuous positive airway pressure (CPAP), but its correct and frequent use is essential to control the disease.
PURPOSE: To analyze adherence to CPAP among patients with OSAS treated in a multidisciplinary outpatient clinic of a public tertiary hospital.
METHODS: This was a retrospective study evaluating 156 patients with OSAS who underwent polysomnography for CPAP titration from 2008 to 2011. The patients were divided into two groups, those with good adherence to CPAP (a mean use of four or more hours per night) and those with poor adherence. The groups were compared regarding the following data: gender, age, body mass index, associated diseases, AHI at diagnostic polysomnography, and pressure (cmH2O) suggested by titration polysomnography.
RESULTS: 125 patients were analyzed, and it was observed that 82 of the patients (65%) had good adherence, whereas 43 (35%) showed poor adherence. Comparison between groups revealed that patients with a higher apnea-hypopnea index (AHI) were those who better adhered to treatment with CPAP.
CONCLUSIONS: the rate of adherence to CPAP among OSAS patients undergoing clinical monitoring at a public service was 65%. Patients with a higher AHI were those who adhered better to treatment with CPAP.
![]()
INTRODUCTION
Obstructive sleep apnea syndrome (OSAS) is currently considered a public health problem, affecting up to 32.8% of the adult population in the city of São Paulo.1 It especially affects obese male patients older than 40 years; age and body mass index (BMI) are significant risk factors.2
If not appropriately diagnosed and treated, OSAS can lead to high morbidity, such as reduced cognitive function3 and increased risk of accidents, and it is associated with diseases such as systemic arterial hypertension,4 metabolic syndrome, acute myocardial infarction, and stroke.
Many factors are associated with the complex physiopathology of OSAS. Decreased airway volume, either due to craniofacial abnormalities or airway obstruction (adenotonsillar hypertrophy, fat deposition in the airways, etc.) has been reported, associated with neuromuscular alterations in this region.
The main complaint related to OSAS is excessive daytime sleepiness (EDS), followed by snoring, increased weight gain, and excessive nocturnal motor activity. The gold standard evaluation to confirm OSAS diagnosis is the polysomnography. Continuous positive airway pressure (CPAP) equipment is one of the most often employed treatments,5 since it is non-invasive, low-risk, relatively simple to use, and highly effective. Studies have demonstrated that, once the patient adheres to treatment, CPAP provides significant improvement in quality of life, reduces daytime sleepiness and other symptoms,6 and considerably decreases risk factors.4
Although extremely positive, the effects of CPAP become irrelevant when the patient does not adhere to its regular use. Poor adherence is a barrier to effective treatment of OSAS, as the regular use of CPAP requires a proactive patient attitude.6
Adherence to CPAP is determined by characteristics of the disease and the patient, previous titration with the equipment, device characteristics and technology, and psychosocial and economic factors.7 Since the nasal interface is preferred, nasal resistance and the use of humidifiers are also important factors for good treatment adherence.8 Moreover, CPAP treatment should ideally involve a multidisciplinary team with physicians, nurses, and physical therapists, among others.9
Lack of adherence to the main treatment of OSAS is an important problem. This study aimed to evaluate CPAP by patients followed in the outpatient clinic of sleep respiratory disorders in a public service, and to evaluate study variables that might be correlated with poor adherence.
METHODS
According to the protocol of the Outpatient Clinic of Sleep Respiratory Disorders of Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, patients that receive a diagnosis of OSAS are referred to CPAP therapy after undergoing nocturnal polysomnography at the Sleep Laboratory, and multidisciplinary clinical assessment by an otolaryngologist, a neurologist, and a pulmonologist. At this time, OSAS is explained to the patient, as well as its causes and its consequences if left untreated. Possible and viable therapeutic modalities are defined and, if indicated, CPAP is introduced to the patient. The goals of treatment are geared towards improving quality of life and reducing associated risks. The patient is then referred for titration polysomnography and instructed to return to the outpatient clinic as soon as the device is available.
Upon return, the device and the mask are verified and adjusted to the patient. The patient is instructed regarding its use, maintenance, and cleaning, as well as possible adverse effects. Periodic visits are scheduled and the patient is instructed to bring the CPAP device for verification of maintenance and time of usage, in order to assess adherence. Practical periodic training is offered to patients who have complaints when attempting to optimize device use. Patients were considered adherent when they used the device for a mean period > four hours a night.
This study assessed 156 medical records of patients with OSAS, who had undergone titration polysomnography between 2008 and 2011. Adherence (number of hours of use/day), anthropometric, and pretreatment polysomnographic data, as well as data on the occurrence of associated diseases (especially cardiovascular, pulmonary, and endocrine diseases) were retrieved from medical records.
Only records with complete data were considered for analysis. Patients with good adherence (group 1 - mean use of four or more hours/night) were compared to patients with poor adherence (group 2 - mean use of less than four hours) regarding gender, age, obesity (clinically assessed based on BMI calculated at the first consultation), and presence of comorbidities reported by the patient (diabetes, hypertension, and dyslipidemia) by Fisher's exact contingency test. Age, diagnostic apnea-hypopnea index (AHI), and CPAP pressure considered to be ideal on the day of titration polysomnography were compared using Student's t-test. The level of significance was set at p < 0.05 for all analyses.
This study was approved by the research ethics committee of the institution, under CAAE number 06340012.0.0000.5440.
RESULTS
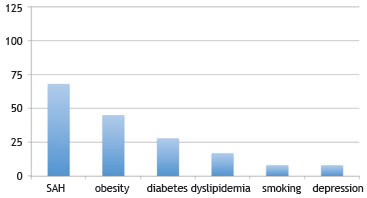
Of the 156 medical records of patients submitted to titration polysomnography, 31 were excluded due to incomplete data. Of the 125 evaluated patients, 68 reported systemic arterial hypertension. Obesity was present in 45 patients, 28 had diabetes, 17 had dyslipidemia, eight were smokers, and eight underwent depression treatment (Fig. 1). Of the analyzed patients, 74 had CPAP indicated for severe OSAS, 37 for moderate OSAS, 13 for mild OSAS (by patient choice or by not being tolerant to any other), and one for pulmonary hypoventilation secondary to neuromuscular disease. The mean age was 56.89 ± 16.01 years; 57 patients were males and 68 were females.
Figure 1 Prevalence of associated diseases in patients with obstructive sleep apnea syndrome (OSAS) using continuous positive airway pressure (CPAP).
All patients were, at the time of initial evaluation, assessed for nasal function, and treated when necessary, either clinically (use of topical corticosteroids and saline solution) or surgically (septoplasty, with or without turbinectomy). None were using a humidifier.
Of the 125 patients, 82 showed good adherence to CPAP and 43 had poor adherence. The reported causes of poor adherence were leakage (n = 7), problems with the mask (n = 7), symptom improvement without CPAP use (n = 4), feeling of suffocation (n = 3), dry mouth (n = 2), insomnia (n = 2), problems with the device (n = 1), and disturbing the partner (n = 1). Fifteen patients gave no justification for not making regular use of CPAP.
Group 1 comprised 82 patients (65%) with a mean age of 56.2 ± 15.8 years, while group 2 comprised 43 patients (35%) with a mean mean age of 57.9 ± 16.4 years. There was no significant difference between the groups (p = 0.57).
The contingency analysis showed no association between adherence to CPAP and gender (p > 0.05). There were 41 males and 41 females in the group of adherent patients. Group 2 consisted of 17 men and 27 women.
The presence of systemic arterial hypertension (45 in group 1 vs. 23 in group 2, p > 0.05), diabetes (16 in group 1 vs. 12 in group 2, p > 0.05), dyslipidemia (13 in group 1 vs. four in group 2, p > 0.05), and obesity (31 in group 1 vs. 14 in group 2, p > 0.05) trended higher in the adherent group, with no statistical difference between the groups.
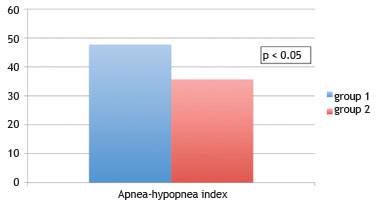
The mean AHI at diagnosis was 47.7 ± 40.7 for group 1, significantly higher (p = 0.04) than that obtained for group 2 (35.7 ± 25.4), with a mean difference of 12.0 (95% CI: 23.81; 0.29) (Fig. 2).
Figure 2 Comparison of apnea-hypopnea index (AHI) between patients with and without good adherence to continuous positive airway pressure. Analyzed by Student's t-test, considered statistically significant when p < 0.05.
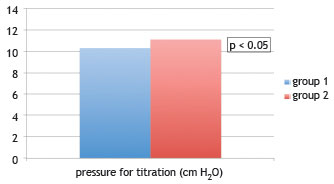
The mean CPAP pressure prescribed by titration was 10.3 ± 3.04 cm of water for group 1 and 11.1 ± 7.11 cm of water for group 2, with no statistically significant difference between the groups (p = 0.56) (Fig. 3).
Figure 3 Comparison of pressure considered ideal for titration (in cm H2O) between patients with and without good adherence to continuous positive airway pressure (CPAP). Analyzed by Student's t-test, considered statistically significant when p < 0.05.
DISCUSSION
OSAS is a highly prevalent and severe disease.1-4 Apnea and hypopnea events can cause hypoxemia, nocturnal awakening, and activation of the sympathetic nervous system, events associated with cognitive complaints, hypertension, type 2 diabetes mellitus, acute myocardial infarction, and metabolic syndrome.8
Many studies have confirmed that the use of CPAP objectively improves AHI and sleepiness symptoms.10-12 However, despite the proven benefits of its use, adherence rates are problematic. Matthews et al.10 reported that 15% to 30% of patients reject CPAP at the start of treatment, and that the rate of long-term adherence is, on average, 50%. Other authors13-18 have reported that adherence to CPAP ranges from 28% to 83%, and that adherence tends to decrease with time, especially in cases where the patient is not followed-up regularly. According to them, one of the main factors that influence adherence is patient instruction on the correct use of the device when the patient first acquires it and periodic follow-up to confirm that the patient is using it, as well as to correct any errors or answer any questions that might arise in that period.
In the present study, the rate of adherence was 65%, after a minimum of one year of use. This relatively good result was probably because patients were trained and instructed on the importance of using the equipment to improve quality of life and to reduce risk factors, in addition to periodic returns for device maintenance and verification of the hour meter, even when the patient has been adherent to the device for a long period of time.
There is no consensus on the influence of demographic data on adherence to CPAP. In the present study, no influence of gender was observed on CPAP adherence, which is in agreement with the results reported by Budhiraja et al.19 However, there was a predominance of women among patients who brought the CPAP to the clinic, despite the clear predominance of OSAS in men. Villar et al.20 reported better adherence to CPAP among women.
Moreover, no influence of age was observed on adherence to CPAP, while Villar et al.20 reported that younger patients of lower socioeconomic level had poorer adherence to the device. This discrepancy between the results can be explained by the fact that the population of the present study did not include very young patients, who probably have the poorest adherence. The influence of socioeconomic factors on the purchase of the device was minimized in the present study due to an agreement between the Hospital, the Regional Department of Health, and the Municipal Governments of DRSXIII - São Paulo, Brazil, in which the latter rent the equipment for the patients and pay for the treatment, when it is indicated.
It is reasonable to assume that the more symptomatic patients are those who show better adherence to treatment. Studies on adherence to CPAP have suggested that patients with worse AHI would show better adherence to treatment.8,21 The present study, as well as the study by Wild et al.,22 confirmed this suspicion. It could be speculated that patients with worse AHI are more adherent because they are more symptomatic and are especially concerned with developing associated diseases.
Shapiro et al.13 reported that BMI and AHI are predictive of better adherence to CPAP. However, no association between treatment adherence and obesity was observed in the present study.
CPAP treatment is important in reducing the risk of possible diseases associated with OSAS. However, adherence to the equipment remains a therapeutic challenge. In this sense, continued patient education and follow-up by a multidisciplinary team should be encouraged in specialized centers for the treatment of patients with OSAS.
CONCLUSION
Approximately two-thirds of the studied patients adequately adhered to CPAP therapy in a center where a multidisciplinary team provides continuous and long-term monitoring to patients. An association was observed between adherence to CPAP and intensity of AHI, and patients with more severe apnea showed better adherence.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
REFERENCES
1. Tufik S, Santos-Silva R, Taddei JA, Bittencourt LR. Obstrucitve sleep apnea syndrome in the São Paulo Epidemiologic Sleep Study. Sleep Med. 2010;11:441-6.
2. Silva GA, Giacon LAT. Síndrome das apneias/hiponeias obstrutivas do sono (SAHOS). Medicina (Ribeirão Preto). 2006;39:185-94.
3. McDaid C, Durée KH, Griffin SC, Weatherly HL, Stradling JR, Davies RJ, et al. systematic review of continuous positive airway pressure for obstructive sleep apnoea-hypopnoea syndrome. Sleep Med Rev. 2009;13:427-36.
4. Marin JM, Agusti A, Villar I, Forner M, Nieto D, Carrizo SJ, et al. Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA. 2012;307:2169-76.
5. Durán-Cantolla J, Aizpurv F, Martínez-Null C, Barbé-Illa F. Obstructive sleep apnea/hypopnoea a systemic hypertension. Sleep Med Rev. 2009;13:323-31.
6. Sullivan CE, Issa FG, Berthon-Jones M, Eves L. Reversal of obstructive sleep apnea by continuous positive airway pressure applied trough the nares. Lancet. 1981;1:862-5.
7. Avlonitov E, Kapsimalis F, Varouchakis G, Vardavas CI, Behrakis P. Adherence to CPAP therapy improves quality of life and reduces symptoms among obstructive sleep apnea syndrome patients. Sleep Breath. 2012;16:563-9.
8. Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence intervention. Sleep Med Rev. 2011;15:343-56.
9. Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, et al. Clinical guideline for evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;15:263-76.
10. Matthews EE, Aloia MS. Continuous positive airway pressure treatment and adherence in obstructive sleep apnea. Sleep Med Clin. 2009;4:473-85.
11. George CF, Boudreau AC, Smiley A. Effects of nasal CPAP on simulated driving performance in patients with obstructive sleep apnoea. Thorax. 1997;52:648-53.
12. Kiely JL, Murphy M, McNicholas WT. Subjective efficacy of nasal CPAP therapy in obstructive sleep apnoea syndrome: a prospective controlled study. Eur Respir J. 1999;13:1086-90.
13. Meurice JC, Paquereau J, Neau JP, Caron F, Dore P, Ingrand P, et al. Long-term evolution of daytime somnolence in patients with sleep apnea/hypopnea syndrome treated by continuous positive airway pressure. Sleep. 1997;20:1162-6.
14. Shapiro GK, Shapiro CM. Factors that influence CPAP adherence: an overview. Sleep Breath. 2010;14:323-35.
15. La Piana GE, Scartabellati A, Chiesa L, Ronchi L, Raimondi P, Carro MA, et al. Long-term adherence to CPAP treatment in patients with obstructive sleep apnea: importance of educational program. Patient Prefer Adherence. 2011;5:555-62.
16. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5:173-8.
17. Sin DD, Mayers I, Man GC, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121:430-5.
18. Nowak C, Bourgin P, Portier F, Genty E, Escourrou P, Bobin S. Nasal obstruction and compliance to nasal positive airway pressure. Ann Otolaryngol Chir Cervicofac. 2003;120:161-6.
19. Brin YS, Reuveni H, Greenberg S, Tal A, Tarasiuk A. Determinants affecting initiation of continuous positive airway pressure treatment. Isr Med Assoc J. 2005;7:13-8.
20. Budhiraja R, Parthasarathy S, Drake CL, Roth T, Sharief I, Budhiraja P, et al. Early CPAP use identifies subsequent adherence to CPAP therapy. Sleep. 2007;30:320-4.
21. Villar I, Izuel M, Carrizo S, Vicente E, Marin JM. Medication adherence and persistence in severe obstructive sleep apnea. Sleep. 2009;32:623-8.
22. Wild MR, Engleman HM, Douglas NJ, Espie CA. Can psychological factors help us to determine adherence to CPAP? A prospective study. Eur Respir J. 2004;24:461-5.
Hospital das Clínicas, Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil
Corresponding author.
F.C.P. Valera
E-mail: facpvalera@fmrp.usp.br
Received 21 April 2013.
Accepted 10 November 2013.
* Institution: Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo.