Year: 2014 Vol. 80 Ed. 2 - (7º)
Artigo Original
Pages: 120 to 125
Complications in the endoscopic and endoscopic-assisted treatment of juvenile nasopharyngeal angiofibroma with intracranial extension*
Author(s): Maria Dantas Costa Lima Godoy1,2; Thiago Freire Pinto Bezerra3; Fabio de Rezende Pinna3; Richard Louis Voegels3
DOI: 10.5935/1808-8694.20140026
Keywords: Angiofibroma; Endoscopy; Video-assisted surgery; Recurrence; Intraoperative complications; Postoperative complications
Abstract:
INTRODUCTION: Although it is a rare neoplasm, juvenile nasopharyngeal angiofibroma (JNA) is associated with high rates of morbidity and mortality, with the potential for intracranial extension. Surgical excision is the main treatment. The external approach has largely been replaced by the endoscopic approach in small lesions, and it can be used as a complement in more advanced cases. However, there is no consensus in the literature regarding the complications of surgical treatment of JNAs with intracranial extension.
AIM: To assess the prevalence of complications in endoscopic or endoscopic-assisted surgical treatment of JNA with minimal intracranial invasion.
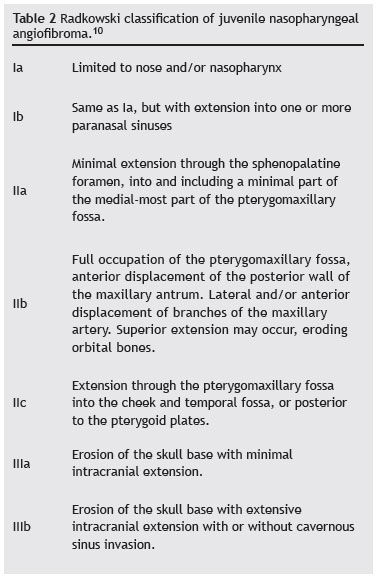
METHODS: This was a retrospective cohort study of all patients with JNA with intracranial extension (Radkowski grade IIIa) treated with endoscopic, endoscopic-assisted, and external surgery from January of 1996 to May of 2010.
RESULTS: Thirteen patients underwent surgery. Endoscopic surgery was performed in three patients, without postoperative complications; endoscopic-assisted surgery in three others, with two instances of complications, and external surgery in seven.
CONCLUSIONS: Operative treatment of nasopharyngeal angiofibroma with intracranial extension is one of the major challenges of ENT and neurosurgical practice. The success rates and low intra- and postoperative complication rates of endoscopic surgery suggest that this route has been gaining ground in the management of Radkowski grade IIIa JNAs.
![]()
INTRODUCTION
Although it is a rare neoplasm, accounting for less than 0.5% of all head and neck tumors,1,2 juvenile nasopharyngeal angiofibroma (JNA) is associated with high rates of morbidity and mortality, with the potential for intracranial extension, which occurs in 10% to 20% of cases.3
Surgical excision is considered the treatment of choice for JNA, regardless of the presence of intracranial invasion.4 A variety of external surgical approaches have been described, such as midfacial degloving, transpalatal approach, lateral rhinotomy, and several craniofacial routes.5 All of these approaches are associated with increased morbidity, due to the need for oral or facial incisions and for removal of bone to gain access to the target lesion.1
For treatment of small lesions, external surgical approaches are gradually being replaced by endoscopic surgery, which can also be combined with conventional approaches in cases of more advanced disease.6 However, there is no consensus in the literature regarding to the complications of surgical treatment, whether endoscopic or open, of JNAs with intracranial extension.1,4,7-9 The objective of this study was to assess the prevalence of complications of endoscopic or endoscopic-assisted surgical treatment of JNAs with minimal intracranial invasion.
MATERIALS AND METHODS
This was a retrospective cohort study. The sample comprised patients with a clinical and radiographic diagnosis of JNA with erosion of the skull base and minimal intracranial extension, meeting criteria for grade IIIa of the Radkowski classification.6,10 Patients were treated between January of 1996 and May of 2010.
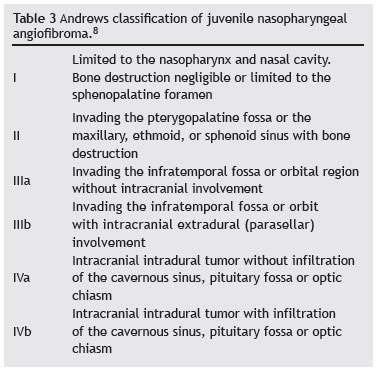
According to the adopted categorization scheme, these patients would correspond to grade IIIb of the Andrews classification.8
All patients underwent preoperative embolization at a single interventional radiology service. For the purposes of this study, the presence of intraoperative or postoperative complications were evaluated and the rates of recurrence and reoperation were measured. Patients requiring craniotomy for neurosurgical access were excluded from the sample, since the findings associated with this route fell outside the scope of the present study.
This study was approved by the local research ethics committee under protocol No. 0459/10.
RESULTS
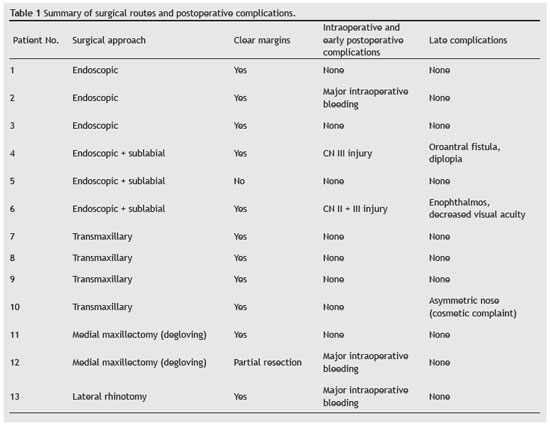
Thirteen patients met the criteria for inclusion and underwent surgical treatment. The demographic profile, surgical techniques used, immediate and delayed complications, and recurrence rate of the sample are listed in Table 1.
The chosen approach was fully endoscopic in three patients, fully external in seven, and combined (endoscopic-assisted) in three. Craniotomy was not performed in any of the patients. Mean patient age was 15.8 ± 2.5 years (range: 11-19 years). Endoscopic-assisted surgical approaches were used in 23% of patients (3/13), and reoperation was indicated in one case.
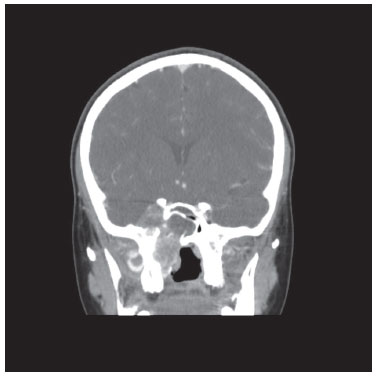
All patients in the sample had Radkowski grade IIIa10 or Andrews grade IIIb8 disease (Figs. 1-4). The Radkowski and Andrews classifications are summarized in Tables 2 and 3 respectively.
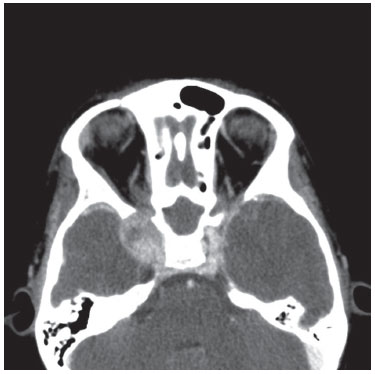
Figure 1 Computed tomography scan (axial view) of a juvenile angiofibroma extending into the right cavernous sinus.
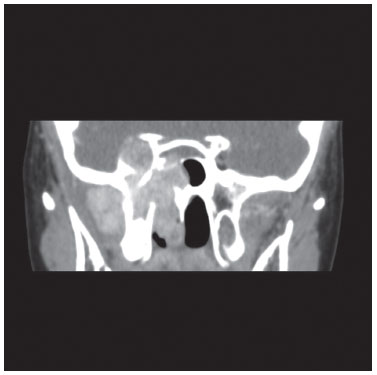
Figure 2 Computed tomography scan (coronal view) of an extensive juvenile angiofibroma. The patient underwent endoscopic-assisted surgery.
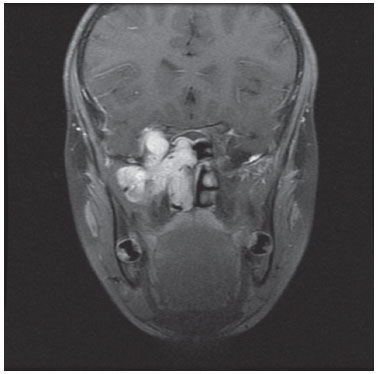
Figure 3 Magnetic resonance imaging (coronal view) of the same patient as Figures 1 and 2.
Figure 4 Postoperative computed tomography scan showing the extent of resection and a tumor recurrence.
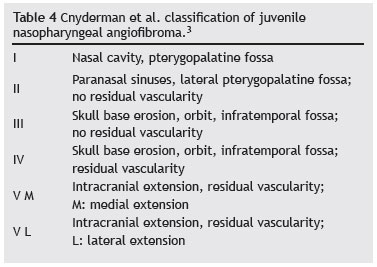
Based on the Snyderman classification,3 residual vascularity following preoperative embolization was present in all cases included the sample. Therefore, all cases corresponded to Snyderman grade IV (Table 4).
Massive intraoperative bleeding was the most common intraoperative complication, occurring in 23% of cases (3/13). Massive bleeding was defined as that leading to hemodynamic instability and requiring packed red blood cell transfusion. In one patient, the procedure had to be halted due to persistent hypovolemic shock despite transfusion, and only partial resection of the tumor was achieved.
Immediate complications of surgery occurred in two patients. One developed oculomotor nerve palsy with CT findings indicative of cavernous sinus thrombosis, and the other sustained optic and oculomotor nerve injury manifesting as decreased visual activity and ptosis. In both cases, a combined surgical approach had been employed. The patient with oculomotor nerve palsy had no improvement at the 12-month follow-up. The condition of the second patient was also unchanged, with persistent palsy, at the 22-month follow-up.
None of the patients who underwent fully endoscopic surgery developed any immediate or delayed complications.
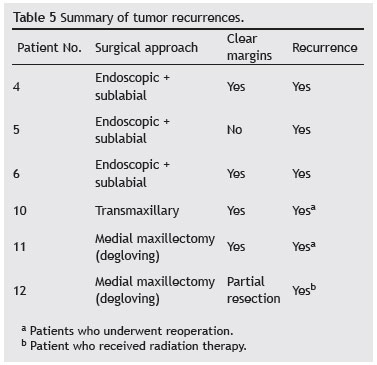
Tumor recurrence occurred in 46% of patients (Table 5). The disease-free period ranged from 10 to 36 months postoperatively. Of these six patients, three (3/13) underwent a second surgical procedure, one (1/13) received radiation therapy, and one (1/13) was simply submitted to further observation. Detection of residual tumor on postoperative follow-up was the criterion for reoperation. The patient who received radiation therapy had an extensive residual lesion that was not amenable to surgical removal by any route. Finally, watchful waiting was chosen as the most appropriate course of action for the remaining patient, due to an absence of symptoms or tumor growth during follow-up, which was probably due to the absence of residual vascularity.
DISCUSSION
Analysis of these 13 patients suggests that fully endoscopic surgery is viable even in advanced cases of JNA.6 Endoscopic approaches may thus be considered one of the most significant advances in treatment of this neoplasm1 and a veritable paradigm shift in its management.11 With progress in the learning curve of the endoscopic route and improvements in the understanding of the complex anatomy of the paranasal sinuses and neurovascular structures of the anterior skull base,11 extended access to the skull base is becoming increasingly popular, broadening the surgeon's armamentarium for JNA management with intracranial invasion.
The endoscope has proved itself to be an important tool for visualizing the entire extent of these tumors, particularly in the region of the superior orbital fissure, cavernous sinus, and even in the pterygopalatine fossa, where the presence of residual lesions is not unusual after resection of tumors as extensive as those described in the present study.1,11
Intraoperative endoscopy may thus render many osteotomies and bone resections unnecessary, which can decrease the risk of changes in facial growth.2 Nevertheless, removal of the lateral nasal wall and posterior portion of the maxilla is required in some cases; the effect of this intervention on facial growth is unknown.1
According to Onerci et al., lesions extending significantly posterior to the pterygoid plates are poor candidates for endoscopic resection. Other essential requirements for the endoscopic approach include adequate surgeon experience, availability of proper instruments, performance of preoperative embolization, and the possibility of adding an open route if necessary.6
In the present study, three patients underwent fully endoscopic resection and three underwent combined (open + endoscopic) procedures for resection of Radkowski grade IIIa JNAs.10 The remaining procedures were performed through conventional external routes. This approach is consistent with the current literature, which recommends that a complete resection through the route associated with the least morbidity should be attempted whenever possible.4,6
Pryor et al.11 found a greater frequency of complications among patients who underwent open procedures as compared with endoscopic surgery. In this study, immediate complications occurred in two patients who underwent surgery via endoscopic-guided external access. None of the three patients who underwent fully endoscopic surgery developed immediate or delayed complications.
Surgical treatment of JNA is fraught with technical challenges, including the risk of intraoperative bleeding, difficulties in tumor dissection, and morbidity associated with the involvement of certain anatomic sites, as well as the risk of recurrence.2 In the present study, only two patients, both in the endoscopic-guided group, developed persistent postoperative complications: one had diplopia and an oroantral fistula, and one had ptosis and decreased visual acuity. The occurrence of irreversible complications in the combined access group may be attributable to the greater surgical difficulty of the affected cases, prompting the decision to use the endoscopic-guided access in the first place. Therefore, the irreversible lesions found in this group may have been the result of the technical challenges encountered during surgery.
In this series, the recurrence rate was 46% (6/13), over a maximum 36-month follow-up. These findings are consistent with those reported in the literature (an overall recurrence rate of 30% to 50%).1 It is noteworthy that the sample consisted of patients with extensive, intracranially invasive tumors, which could have led to a higher recurrence rate.
Due to the benign nature of JNAs, the vast majority of these tumors remain extradural even when there is intracranial extension,9 and the surgical plane is situated between important structures such as the internal carotid artery and cavernous sinus.4 However, lateral extension of the tumor into the infratemporal fossa, the parasellar region, or the vicinity of the optic nerve can pose challenges to endoscopic resection.9
Even though JNAs are covered by nasopharyngeal mucosa, in the authors' experience identification of the plane of dissection can be somewhat challenging, particularly when close to the cavernous sinus. In this study, one patient developed a postoperative decline in visual acuity which remained at the 22-month follow-up, most likely due to inadvertent optic nerve injury during the procedure. The authors believe that this injury may have been secondary to the heat of electrocoagulation.
Some authors maintain that endoscopic approaches should only be used when the tumor is confined to the nasal cavity, paranasal sinuses, pterygopalatine fossa, or infratemporal fossa. When a conventional approach is required for resection of lesions that extend beyond the boundaries of endoscopic visualization, endoscopy should still be used as an adjunct to the external route.12,13 However, the present authors agree with Andrade et al. that a reassessment of the limits of endoscopic resection of JNA, to include larger tumors and cases with some intracranial invasion, is required.2 To the best of the authors' knowledge, this was one of the largest series restricted to patients with JNAs with intracranial extension treated exclusively via non-neurosurgical routes.
The limitations of the present study should also be considered. As previously noted, this case series was restricted to non-neurosurgical routes; patients who required craniotomy due to tumor extension (Radkowski grade IIIb) were excluded.10 A comparison of these different approaches would be an interesting subject for future research. However, in view of the findings of this study, fully endoscopic or endoscopic-guided access should be considered even for advanced-stage tumors with major intracranial extension.
Endoscopic treatment of lesions of the skull base is a branch of surgery that is currently undergoing rapid progress. Use of neuronavigation techniques, intraoperative MRI, customized instruments, and ever-increasing surgical experience are all factors contributing to further advancements in this field, toward safer and more effective endoscopic approaches.13
CONCLUSION
Operative treatment of nasopharyngeal angiofibroma with intracranial extension is one of the major challenges of ENT and neurosurgical practice. The success rates and low intra- and postoperative complication rates of endoscopic surgery suggest that this route has been gaining ground in the management of Radkowski IIIa class JNAs.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
REFERENCES
1. Enepekides DJ. Recent advances in the treatment of juvenile angiofibroma. Curr Opin Otolaryngol Head Neck Surg. 2004;12:495-9.
2. Andrade NA, Pinto JA, Nóbrega MO, Aguiar JE, Aguiar TF, Vinhaes ES. Exclusively endoscopic surgery for juvenile nasopharyngeal angiofibroma. Otolaryngol Head Neck Surg. 2007;137:492-6.
3. Snyderman CH, Pant H, Carrau RL, Gardner P. A new endoscopic staging system for angiofibromas. Arch Otolaryngol Head Neck Surg. 2010;136:588-94.
4. Danesi G, Panciera DT, Harvey RJ, Agostinis C. Juvenile nasopharyngeal angiofibroma: evaluation and surgical management of advanced disease. Otolaryngol Head Neck Surg. 2008;138:581-6.
5. Ardehali MM, Samimi Ardestani SH, Yazdani N, Goodarzi H, Bastaninejad S. Endoscopic approach for excision of juvenile nasopharyngeal angiofibroma: complications and outcomes. Am J Otolaryngol. 2010;31:343-9.
6. Onerci TM, Yücel OT, Oğretmenoğlu O. Endoscopic surgery in treatment of juvenile nasopharyngeal angiofibroma. Int J Pediatr Otorhinolaryngol. 2003;67:1219-25.
7. Pryor SG, Moore EJ, Kasperbauer JL. Endoscopic versus traditional approaches for excision of juvenile nasopharyngeal angiofibroma. Laryngoscope. 2005;115:1201-7.
8. Andrews JC, Fisch U, Valavanis A, Aeppli U, Makek MS. The surgical management of extensive nasopharyngeal angiofibromas with the infratemporal fossa approach. Laryngoscope. 1989;99:429-37.
9. Douglas R, Wormald PJ. Endoscopic surgery for juvenile nasopharyngeal angiofibroma: where are the limits? Curr Opin Otolaryngol Head Neck Surg. 2006;14:1-5.
10. Radkowski D, McGill T, Healy GB, Ohlms L, Jones DT. Angiofibroma. Changes in staging and treatment. Arch Otolaryngol Head Neck Surg. 1996;122:122-9.
11. Lund VJ, Stammberger H, Nicolai P, Castelnuovo P, Beal T, Beham A, et al. European position paper on endoscopic management of tumours of the nose, paranasal sinuses and skull base. Rhinol Suppl. 2010;22:1-143.
12. Ogawa AI, Fornazieri MA, da Silva LV, Pinna FR, Voegels RL, Sennes LU, et al. Juvenile angiofibroma: major and minor complications of preoperative embolization. Rhinology. 2012;50:199-202.
13. Carrau RL, Snyderman CH, Kassam AB, Jungreis CA. Endoscopic and endoscopic-assisted surgery for juvenile angiofibroma. Laryngoscope. 2001;111:483-7.
1. Universidade de São Paulo (USP), São Paulo, SP, Brazil
2. Hospital do Servidor Público Estadual de São Paulo, São Paulo, SP, Brazil
3. Hospital das Clínicas da Faculdade de Medicina, Universidade de São Paulo (USP), São Paulo, SP, Brazil
Corresponding author.
M.D.C.L. Godoy
E-mail: mariadcostalima@hotmail.com
Received 8 April 2013.
Accepted 12 October 2013.
* Study conducted at Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, São Paulo, SP, Brazil.