Year: 2014 Vol. 80 Ed. 1 - (8º)
Artigo Original
Pages: 29 to 34
Localization of ectopic and supernumerary parathyroid glands in patients with secondary and tertiary hyperparathyroidism: surgical description and correlation with preoperative ultrasonography and Tc99m-Sestamibi scintigraphy
Author(s): José Santos Cruz de Andrade1; João Paulo Mangussi-Gomes1; Lillian Andrade da Rocha2; Monique Nakayama Ohe3; Marcello Rosano1; Murilo Catafesta das Neves2; Rodrigo de Oliveira Santos1,2
DOI: 10.5935/1808-8694.20140008
Keywords: Hyperparathyroidism; Parathyroid glands; Parathyroidectomy; Chronic renal insufficiency; Ultrasonography; Scintigraphy
Abstract:
INTRODUCTION: Hyperparathyroidism is an expected metabolic consequence of chronic kidney disease (CKD). Ectopic and/or supernumerary parathyroid glands (PT) may be the cause of surgical failure in patients undergoing total parathyroidectomy (PTX).
AIM: To define the locations of ectopic and supernumerary PT in patients with renal hyperparathyroidism and to correlate intraoperative findings with preoperative tests.
MATERIALS AND METHODS: A retrospective study was conducted with 166 patients submitted to PTX. The location of PT during surgery was recorded and classified as eutopic or ectopic. The preoperative localizations of PT found by ultrasonography (USG) and Tc99m-Sestamibi scintigraphy (MIBI) were subsequently compared with intraoperative findings.
RESULTS: In the 166 patients studied, 664 PT were found. Five-hundred-seventy-seven (86.4%) glands were classified as eutopic and 91(13.6%) as ectopic. Eight supernumerary PT were found. The most common sites of ectopic PT were in the retroesophageal and thymic regions. Taken together, USG and MIBI did not identify 56 (61.5%) ectopic glands. MIBI was positive for 69,7% of all ectopic glands located in the mediastinal and thymic regions.
CONCLUSION: The presence of ectopic and supernumerary PT in patients with renal hyperparathyroidism is significant. Although preoperative imaging tests did not locate most of ectopic glands, MIBI may be important for identifying ectopic PT in the mediastinal and thymic regions.
![]()
INTRODUCTION
Hyperparathyroidism is a physiological response to metabolic changes that occurs in patients with chronic kidney disease (CKD). In spite of advances in the clinical treatment of these patients, a significant number develops parathyroid (PT) hyperfunction and autonomy, with consequent elevation of parathyroid hormone (PTH). When the harmful effects of hyperparathyroidism are identified, such as severe bone disease, surgical treatment becomes necessary.1
Thus, total parathyroidectomy (PTx) in CKD has been indicated in symptomatic patients with marked and non-suppressible elevations of PTH.1 The goal of surgery is to correctly identify and resect all PTs. Although the hyperplastic glands are much larger than normal due to kidney disease, their identification is not always simple.2,3 Moreover, although the finding of four glands is expected in most patients, there is significant variability in the number of PTs. Supernumerary glands are present in 2.5% to 30% of patients,4,5 and may be the reason for surgical treatment failure, if not properly identified.2,6
There is also considerable variation regarding the location of the PTs, which are often not found in their usual location. The identification of all glands may require a thorough exploration of the superior mediastinum regions, thyroid gland, carotid sheath, and retroesophageal area.5,7
As a result, imaging studies have been performed to quantify and locate the PTs before surgery. However, although widely used in patients with CKD-associated hyperparathyroidism, it is not yet known whether ultrasonography (USG) and 99mTc-sestamibi (MIBI) scintigraphy can affect surgical outcomes, complication rates, and long-term therapeutic success.8-10
This study aimed to evaluate the main locations of the PTs in patients with secondary (SHPT) and tertiary (THPT) hyperparathyroidism, based on intraoperative findings, and to correlate these findings with the preoperative examinations.
MATERIALS AND METHODS
A cross-sectional study including patients with CKD treated at a tertiary referral hospital was performed. Between February of 2011 and October of 2012, 166 patients (44 diagnosed with SHPT and 122 diagnosed with THPT) underwent PTx with presternal parathyroid autotransplantation. All patients were examined by a nephrologist specialized in renal osteodystrophy; surgical indication followed the criteria of clinical treatment failure: hypercalcemia and/or persistent hyperphosphatemia; pruritus; bone pain; fractures or high risk of fractures; skeletal deformities and/or calcifications; calciphylaxis; and radiographic evidence of renal osteodystrophy. Patients who had previously undergone PT surgery were excluded from the analysis.
Patients were referred for surgical evaluation after preoperative imaging examinations had been performed at the service of origin or at the hospital in which the surgery was performed. USG and MIBI images reports from each patient were analyzed, the number of PTs observed, and their locations were quantified for each test. In cases where the MIBI image was not available for analysis by the surgeon, the examination report was considered. Preoperative imaging assessments were not performed by the same radiologist, nor in the same radiology department.
All patients were submitted to surgery by the same surgical team. The surgical technique consisted of conventional parathyroidectomy with bilateral neck exploration and heterotopic presternal intramuscular autotransplantation, as previously described.11
During the procedure, the location of the PT was recorded; it was considered normal when the lower glands were related to the lower pole of the thyroid gland, and when the upper glands were found near the upper pole of the thyroid, by the entry point of the inferior laryngeal nerve in the cricothyroid muscle.
When the PT was not identified in its usual position, a systematic exploration of the following areas was performed: retroesophageal, carotid sheath, thymic tongue, and upper mediastinum. If even then the PT was not identified, an ipsilateral total lobectomy of the thyroid gland was performed.
For those patients in whom the PT was not identified intraoperatively, but with persistence or recurrence of disease in the postoperative follow-up, the gland was classified as ectopic and the case was considered a "surgical failure".
PT fragments were sent for cryopreservation in most patients. Intraoperative frozen pathology was not performed in any case. Although the collection of intraoperative PTH (IOPTH) was performed in all cases (two blood samples, one at anesthetic induction, and another 20 minutes after removal of all glands), the result did not affect the surgical decision in any situation, due to the delay in obtaining these results.11
Only patients with a minimum postoperative follow-up period of 6 months were included in the study.
Finally, the data provided by radiological preoperative imaging were compared with the intraoperative findings for each patient. The present study was approved by the research ethics committee of the institution under protocol No. 886/00.
RESULTS
Of the 166 patients studied, 44 had a diagnosis of SHPT and 122 of THPT. Regarding gender, 82 were males and 84 were females. The mean age among patients with SHPT and THPT was 46.3 years (range: 23-67 years) and 48.1 years (range: 21-72 years), respectively. The mean duration of dialysis in patients with SHPT was 10.2 years (range: 2-25 years) and in patients with THPT, 6.1 years (range: 0.5 to 17 years).
A total of 664 PTs were found in 166 patients undergoing surgery. Four PTs were identified in 150 patients; five PTs were identified in eight patients (4.8%), and only three PTs in eight other patients (4.8%).
Of the eight patients with only three glands identified intraoperatively, four (2.4%) did not present clinical and laboratory evidence of disease recurrence. The other four patients (2.4%) had evidence of persistent or recurrent hyperparathyroidism in the postoperative follow-up, and their missing glands were considered ectopic. Surgical failure was, therefore, 2.4%.
Regarding the location of PTs, 577 (86.4%) glands were classified as eutopic, and 91 (13.6%) as ectopic (87 located in non-usual position, and four that were not found intra-operatively).
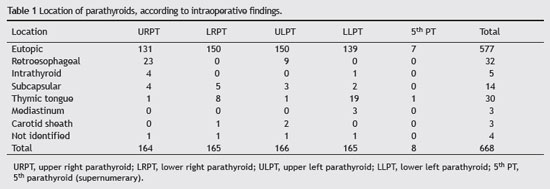
Considering a total number of 668 PTs (ectopic and eutopic), 664 glands (99.4%) were located. The surgical location of PTs is shown in Table 1.
Regarding the 87 ectopic glands, the upper-right PT (URPT) and lower-left PT (LLPT) were the most commonly found in non-usual positions, representing, 36.3% and 28.6% of total ectopic findings, respectively.
Regarding the URPT, it was considered ectopic in 24.6% of cases, and the retroesophageal position was the most frequent (71.8%). The LLPT, in turn, was classified as ectopic in 17% of cases, and the thymic region was the most common location (76%).
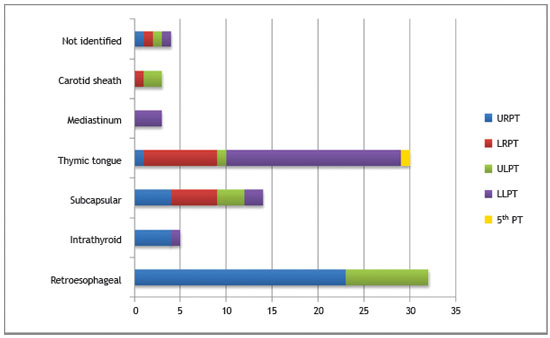
Of the eight supernumerary PTs that were identified, seven were located in eutopic positions. Only one was ectopic. Fig. 1 shows the location of ectopic PTs.
Figure 1 Intraoperative identification of ectopic parathyroids. The parathyroid glands that were not identified intraoperatively were also included. URPT, upper right parathyroid; LRPT, lower right parathyroid; ULPT, upper left parathyroid; LLPT, lower left parathyroid; 5th PT, 5th parathyroid (supernumerary).
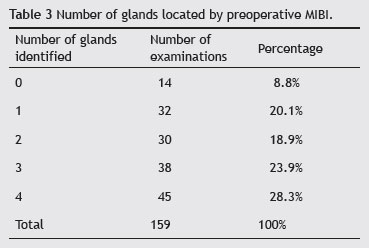
During the preoperative assessment, 153 patients (92.1%) underwent USG. The number of glands located is shown in Table 2. As for MIBI, 159 patients (95.7%) underwent the examination. The number of glands located is shown in Table 3. The mean number of glands identified by USG was 1.58 glands/exam. MIBI identified a mean of 2.41 glands/exam.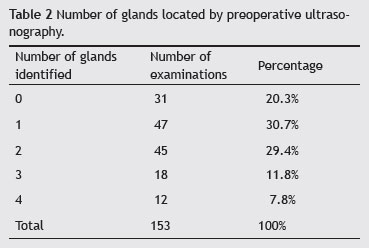
The association between ectopic PTs and imaging tests was as follows:Of the three PTs found in the carotid sheath, only one was located by the USG and MIBI. In the other two cases, both the USG and the MIBI were negative. Of the five intrathyroid PTs, only two were suggested by USG, and three were not identified either by USG or by MIBI. Of the three mediastinal PTs, all were visualized by MIBI.
Regarding the 30 ectopic PTs located in the thymic tongue, five were not identified in any of the examinations, ten were identified only by MIBI, five were identified only by USG, and ten were identified by USG and MIBI.
No ectopic PT located in the subcapsular or retroesophageal region was identified by USG or MIBI before surgery. When considering only the regions of the upper mediastinum and thymus, the USG was able to identify 45.5% of ectopic PTs, all located in the thymic tongue. MIBI identified 69.7% of the glands in these regions.
Preoperatively, the USG and MIBI correctly identified 18 (19.8%) and 24 (26.4%) of ectopic PTs, respectively. Regarding ectopic PTs, 31 (34.1%) were identified by USG and/or MIBI; 60 ectopic glands (65.9%) were not identified by any of the preoperative examinations used in this study.
DISCUSSION
Although IOPTH and frozen pathology were not used to confirm the removal of all glands intraoperatively, 99.4% of PTs were correctly located in the sample presented. Furthermore, only 2.4% of patients had surgical failure in the postoperative follow-up.
The main causes of failure in the surgical treatment of patients with hyperparathyroidism associated with CKD are failure to identify the PTs or presence of supernumerary glands. Both situations can be related to the existence of ectopic PTs.5
The frequency of ectopic PTs in the present study was 13.6%, similar to that found by other authors. Gomes et al.3 reported 18.9% ectopic glands, while the rate observed by Vulpio et al. was 12%.8
The main difference compared to the literature, however, is the location of the ectopic glands. While in the present study the regions where ectopic PTs were most commonly found were, in descending order, retroesophageal areas (35.2% of all ectopic PTs, with upper PTs in 100% of cases) and thymus (32.9% of ectopic PTs, with lower PTs in 90% of cases), the literature describes only the thymus region as the most common for the finding of ectopic PTs (lower, in most cases).3,12-14
All authors agree that the position of the gland is related to embryological development. The lower PTs originate from the third branchial arch together with the thymus, while the upper PTs originate from the fourth branchial arch. The migration of lower PTs, longer and closer to the thymic tissue, would determine the greater variability in their final position.12-14
Another major cause of failure at the initial surgery is the presence of supernumerary PTs, identified in 4.8% of patients in the present series. In the literature, the presence of supernumerary glands is quite variable, ranging from 2.5% to 30%.4,5,14 The explanation for such a significant variation may be related to differences in the surgical techniques used in each study.
Therefore, some authors recommend a routine cervical thymectomy during the surgical treatment of patients with hyperparathyroidism associated with CKD.3,5,13,14 Pattou et al., for instance, in a study of 290 patients submitted to PTx and routine cervical thymectomy due to hyperparathyroidism associated with CKD, found supernumerary PTs located in the thymic region in 70 individuals (24.1% of total number of patients).5
The fact that routine cervical thymectomy was not performed in this study may explain the small number of supernumerary PTs found mainly in the thymus and/or upper mediastinum regions. Nevertheless, the surgical failure rate was only 2.4%, similar to that demonstrated by other authors. Tominaga et al., for instance, reported a 4.2% failure rate in 1,156 patients who underwent surgery.6
This apparent nonsensical finding is explained, as most supernumerary PTs found in the thymus actually represent small grafts of microscopic embryonic remnants. These grafts were unlikely to have the capacity to promote disease recurrence and/or persistence.
The capacity of imaging studies to locate the PTs preoperatively, especially ectopic glands, can greatly influence the surgical outcome.9,15
In this series of patients, the USG located 1.58 PTs/exam and MIBI located 2.41 PTs/exam. Many studies have shown conflicting data on the sensitivity and specificity of imaging studies in this group of patients.8,9,12,16 However, few have correlated the imaging findings with the intraoperative identification of ectopic glands.
Thus, considering only the ectopic PTs, the combination of USG and MIBI was able to identify only 34.1% of the glands. Separately, the USG located only 19.8% of ectopic PTs, and MIBI, 26.4%. As shown, it is already clear in the literature that the combination of imaging methods is superior to their isolated use.8,9,17
The low accuracy of USG and MIBI in identifying ectopic glands is explained by the limitations inherent to the methods. In the case of retroesophageal PTs, for instance, USG suffers interference from the trachea, and MIBI, from the thyroid.8,9,18 In this series, no retroesophageal gland was suggested by imaging studies.
Fortunately, the capacity of these tests to locate PTs in the upper mediastinum and thymic regions is higher.8,16 During the intraoperative period, the dissection of the retroesophageal area is much simpler to perform, when compared to the upper mediastinum approach. Mediastinal dissections can hardly be performed without any suggestion of the presence of a gland in this region, due to the higher morbidity of this surgical approach.
MIBI was able to identify 69.7% of PTs in the upper mediastinum and thymic tongue, versus only 45.5% identified by the USG. All three cases of mediastinal PTs were shown by MIBI.
The superiority of MIBI when compared to USG to identify PTs in the upper mediastinum and thymic regions has been described in the literature. In the study by Vulpio et al., USG did not identify any ectopic PT in the upper mediastinal or thymic regions versus 78% by MIBI.8 Similarly, Gasparri et al. demonstrated that preoperative MIBI was able to correctly identify 73.7% of ectopic glands in these regions.18
The real value of preoperative examinations in the context of hyperparathyroidism associated with CKD is yet to be determined. Some authors state that they do not change the primary surgery outcomes, as long as it is performed by an experienced surgeon.17,18 However, other authors have obtained good results with preoperative imaging analysis, and recommend the combined use of MIBI and USG in the preoperative evaluation of patients with hyperparathyroidism associated with CKD.9
This study was conducted in a public hospital with limited resources. Any technology that helps in the treatment of these patients is always well accepted. However, their unavailability should not prevent or contraindicate the surgery. In this study, IOPTH and pathological anatomy were not considered in the intraoperative decisions, which also did not compromise the surgical outcome.
The USG assessment is recommended as the most important preoperative examination, as it is more accessible and provides information regarding PTs and possible thyroid diseases, which are very prevalent in our country.Whenever possible, the additional utilization of MIBI to identify possible ectopic glands in the thymic and mediastinal regions is recommended, although this situation represents a minority of patients.
CONCLUSION
The presence of supernumerary and ectopic parathyroid glands in patients undergoing PTx for CKD-associated hyperparathyroidism is significant and justifies a careful intraoperative search. An exploration routine for the most common sites of ectopic gland location is necessary, which in this study were the retroesophageal and thymic regions for the upper and lower parathyroids, respectively. Although preoperative imaging exams did not identify the majority of ectopic glands, MIBI may have an important role as a surgical planning method, in the identification of ectopic PT located in the upper mediastinal and thymic regions.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
REFERENCES
1. The National Kidney Foundation Kidney Disease Outcomes Quality Initiative (NKF KDOQI). Clinical Practice Guidelines and Clinical Practice Recommendations for Diabetes and Chronic Kidney Disease. Am J Kidney Dis. 2007;49:S12-154.
2. Gough I. Reoperative parathyroid surgery: the importance of ectopic location and multigland disease. ANZ J Surg. 2006;76:1048-50.
3. Gomes EMS, Nunes RC, Lacativa PGS, Almeida MH de, Franco FM, Leal CTS, et al. Ectopic and extranumerary parathyroid glands location in patients with hyperparathyroidism secondary to end stage renal disease. Acta Cir Bras. 2007;22:105-9.
4. Wang C. The anatomic basis of parathyroid surgery. Ann Surg. 1976;183:271-5.
5. Pattou FN, Pellissier LC, Noël C, Wambergue F, Huglo DG, Proye CA. Supernumerary parathyroid glands: frequency and surgical significance in treatment of renal hyperparathyroidism. World J Surg. 2000;24:1330-4.
6. Tominaga Y, Katayama A, Sato T, Matsuoka S, Goto N, Haba T, et al. Re-operation is frequently required when parathyroid glands remain after initial parathyroidectomy for advanced secondary hyperparathyroidism in uraemic patients. Nephrol Dial Transplant. 2003;18:iii65-70.
7. Numano M, Tominaga Y, Uchida K, Orihara A, Tanaka Y, Takagi H. Surgical significance of supernumerary parathyroid glands in renal hyperparathyroidism. World J Surg. 1998;22:1098-102.
8. Vulpio C, Bossola M, De Gaetano A, Maresca G, Bruno I, Fadda G, et al. Usefulness of the combination of ultrasonography and 99mTc-sestamibi scintigraphy in the preoperative evaluation of uremic secondary hyperparathyroidism. Head Neck. 2010;32:1226-35.
9. Périé S, Fessi H, Tassart M, Younsi N, Poli I, St Guily JL, et al. Usefulness of combination of high-resolution ultrasonography and dual-phase dual-isotope iodine 123/technetium Tc 99m sestamibi scintigraphy for the preoperative localization of hyperplastic parathyroid glands in renal hyperparathyroidism. Am J Kidney Dis. 2005;45:344-52.
10. Chiu B, Sturgeon C, Angelos P. What is the link between nonlocalizing sestamibi scans, multigland disease, and persistent hypercalcemia? A study of 401 consecutive patients undergoing parathyroidectomy. Surgery. 2006;140:418-22.
11. Santos RO, Ohe MN, Carvalho AB, Neves MC, Kunii I, Lazaretti-Castro M, et al. Total parathyroidectomy with presternal intramuscular autotransplantation in renal patients: a prospective study of 66 patients. J Osteoporos. 2012;2012:631243.
12. Mariani G, Gulec SA, Rubello D, Boni G, Puccini M, Pelizzo MR, et al. Preoperative localization and radioguided parathyroid surgery. J Nucl Med. 2003;44:1443-58.
13. Noussios G, Anagnostis P, Natsis K. Ectopic parathyroid glands and their anatomical, clinical and surgical implications. Exp Clin Endocrinol Diabetes. 2012;120:604-10.
14. Schneider R, Waldmann J, Ramaswamy A, Fernández ED, Bartsch DK, Schlosser K. Frequency of ectopic and supernumerary intrathymic parathyroid glands in patients with renal hyperparathyroidism: analysis of 461 patients undergoing initial parathyroidectomy with bilateral cervical thymectomy. World J Surg. 2011;35:1260-5.
15. Madorin C, Owen RP, Fraser WD, Pellitteri PK, Radbill B, Rinaldo A, et al. The surgical management of renal hyperparathyroidism. Eur Arch Otorhinolaryngol. 2012;269:1565-76.
16. Sukan A, Reyhan M, Aydin M, Yapar AF, Sert Y, Canpolat T, et al. Preoperative evaluation of hyperparathyroidism: the role of dual-phase parathyroid scintigraphy and ultrasound imaging. Ann Nucl Med. 2008;22:123-31.
17. Lai ECH, Ching ASC, Leong HT. Secondary and tertiary hyperparathyroidism: role of preoperative localization. ANZ J Surg. 2007;77:880-2.
18. Gasparri G, Camandona M, Bertoldo U, Sargiotto A, Papotti M, Raggio E, et al. The usefulness of preoperative dual-phase 99mTc MIBI-scintigraphy and IO-PTH assay in the treatment of secondary and tertiary hyperparathyroidism. Ann Surg. 2009;250:868-71.
1. Department of Otolaryngology, Head and Neck Surgery, Universidade Federal de São Paulo/Escola Paulista de Medicina (UNIFESP/EPM), São Paulo, SP, Brazil
2. Department of Nephrology, Universidade Federal de São Paulo/Escola Paulista de Medicina (UNIFESP/EPM), São Paulo, SP, Brazil
3. Department of Clinical Endocrinology, Universidade Federal de São Paulo/Escola Paulista de Medicina (UNIFESP/EPM), São Paulo, SP, Brazil
Corresponding author.
J. Mangussi-Gomes
E-mail: joaopauloemt@gmail.com
Received 22 June, 2013.
Accepted 12 October, 2013.