Year: 2013 Vol. 79 Ed. 6 - (21º)
Relato de Caso
Pages: 790 to 790
Paracoccidioidomycosis of the larynx: Cases Report
Author(s): Claudiney Candido Costa1; Valeriana de Castro Guimarães2; Marina Neves Rebouças3; Edson Junior de Melo Fernandes4
DOI: 10.5935/1808-8694.20130141
Keywords: larynx; paracoccidioidomycosis; sulfamethoxazole; trimethoprim-sulfamethoxazole combination.
![]()
INTRODUCTION
Paracoccidioidomycosis is a severe systemic disease caused by Paracoccidioides brasiliensis (P. brasiliensis). It is a thermal dimorphic fungus, usually acquired through the respiratory tract by inhalation of spores in the air. The infection is insidious and chronic, characterized by the appearance of lesions in the oral and nasal cavities, pharynx, larynx, gums, tongue, soft palate, adrenal glands, liver, bones, gastrointestinal tract, lungs, skin, lymph nodes and nervous system. Dysphonia, dyspnoea, sore throat, dysphagia, weight loss, fever and cough may present as the initial symptoms of the disease. Men over 40, smokers and/or alcohol drinkers are more affected1-3.
In this report, the authors describe three patients with laryngeal paracoccidioidomycosis treated at a public hospital in the Midwest of Brazil.
CASE REPORT
Case 1
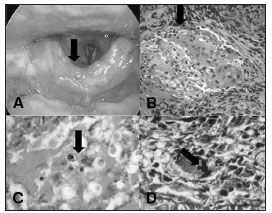
Male, 56 years old, smoker for 40 years and ex-alcoholic, coming from Aragarças, TO, with an epiglottis lesion. Upon laryngoscopy there was an ulcerative-infiltrative-vegetative lesion in the anterior face of the epiglottis, with cartilage fixation (Figure 1A). The CT scan showed nodules with cavitations in the pulmonary apex compatible with a chronic granulomatous process. The biopsy was performed in an outpatient basis.
Case 2
Male, 60 years old, smoker, born and living in Santa Rita do Araguaia, GO, complaining of dysphonia, severe dyspnea and weight loss for 3 months. The Videolaryngoscopy revealed an ulcerative-vegetative-infiltrating lesion on the right vocal fold and right-side ventricular band, extending to the entire posterior commissure, fixating the vocal folds. This patient was submitted to an emergency tracheotomy. A larynx biopsy was carried out under general anesthesia.
Case 3
Male, 60 years, smoker, coming from Goiânia, GO, complaining of dysphonia for six months worsened in recent months. Upon videolaryngoscopy, there was an ulcerative-infiltrative-vegetative lesion on the vocal folds, partially fixating them. Biopsy was performed under general anesthesia. With no clinical improvement, we investigated tracheal stenosis, which was confirmed by bronchoscopy.
Figure 1. Laryngoscopy: Ulcerative-infiltrative-vegetative lesion on
the anterior surface of the epiglottis (a); Histopathology: HE 200x granuloma (b); fungus Paracoccidioides PAS 100x (c); Grocott 400x Mickey-Mouse-type budding (d).
In all three cases, histopathological examination identified granulomatous process with fungi, suggestive of P. brasiliensis (Figures 1B-1D), being treated with trimethoprim-sulfamethoxazole.w
DISCUSSION
Diagnosis is based on clinical findings and the identification of P. brasiliensis, present in the pathological exam of the lesions1,2,4. In the cases described, the patients had lesions in the larynx, and were submitted to core biopsy, with a histopathology result suggestive of infection by P. brasiliensis1,3,5. Lesions found in cases of paracoccidioidomycosis are similar to laryngeal neoplasia, requiring differential diagnosis, and thus the established approach is the histopathological exam4.
Rural workers are at a higher risk because the disease affects mostly individuals whom, by their occupations, are in constant contact with vegetables and earth2,3. Corroborating with the literature, in the reported cases the patients are coming from endemic regions for P. brasiliensis, they are males, smokers and ex-alcoholic and two worked with farming.
Machado Filho et al.3, evaluated 104 individuals diagnosed with the disease. Of these, approximately 40 % had laryngeal lesions, and the vocal cords and epiglottis were the most affected structures.
The literature describes lung nodules as the most common radiological findings2,6. In one of the cases presented, the CT scan showed areas of cavitations with nodules in the lung apex.
In all three cases, the treatment was performed in outpatient clinics with sulfamethoxazole and trimethoprim, due to ease of administration (per os), better compliance and tolerability6. Drug maintenance and regular outpatient follow up were followed as suggested by some authors6.
FINAL REMARKS
Paracoccidioidomycosis should be considered in the differential diagnosis of patients with laryngeal lesions, especially those who reside or resided in endemic areas of P. brasiliensis.
REFERENCES
1. Lopes Neto JM, Severo LM, Mendes RP, Weber SAT. Sequelae lesions in the larynxes of patients with paracoccidioidomycosis. Braz J Otorhinolaryngol. 2011;77(1):39-43.
2. Freitas RM, Prado R, Prado FL, Paula IB, Figueiredo MT, Ferreira CS, et al. Pulmonary paracoccidioidomycosis: radiology and clinical-epidemiological evaluation. Rev Soc Bras Med Trop. 2010;43(6):651-6. PMID: 21181017 DOI: http://dx.doi.org/10.1590/S0037-86822010000600010
3. Machado Filho J, Rego AP, Chaves ALF, Miranda JL, Silva CC. Considerações relativas à Blastomicose Sul-americana. Da participação laríngea e brônquica em 104 casos: resultados endoscópicos. Hospital (RJ). 1960;(58):645-58.
4. Sant'Anna GD, Mauri M, Arrarte JL, Camargo H Jr. Laryngeal manifestations of paracoccidioidomycosis (South American blastomycosis). Arch Otolaryngol Head Neck Surg. 1999;125(12):1375-8. PMID: 10604418 DOI: http://dx.doi.org/10.1001/archotol.125.12.1375
5. Benard G, Campos AF, Netto LC, Gonçalves LG, Machado LR, Mimicos EV, et al. Treatment of severe forms of paracoccidioidomycosis: is there a role for corticosteroids? Med Mycol. 2012;50(6):641-8. DOI: http://dx.doi.org/10.3109/13693786.2011.654135
6. Wanke B, Aidê MA. Chapter 6-paracoccidioidomycosis. J Bras Pneumol. 2009;35(12):1245-9. DOI: http://dx.doi.org/10.1590/S1806-37132009001200013
1. PhD in Medicine - Otolaryngology; Adjunct Professor and Head - Department of Otorhinolaryngology, Medical School, Federal University of Goiás
2. PhD in Health Sciences; Speech Epidemiologist. Department of Otorhinolaryngology, Medical School, Federal University of Goiás, Goiânia, GO
3. ENT. Otolaryngologist. Medical School, Federal University of Goiás, Goiânia, GO
4. MD. Resident Physician, Department of Otorhinolaryngology, Medical School, Federal University of Goiás, Goiânia, GO
Medical School, Federal University of Goiás.
Send correspondence to:
Claudiney Candido Costa
Primeira Avenida, s/nº. Setor Leste Universitário
Goiânia - GO. Brasil. CEP: 74.605-020
E-mail: orlccp@uol.com.br
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on June 11, 2012; and accepted on July 28, 2012. cod. 9260.
All rights reserved - 1933 /
2025
© - Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico Facial