Year: 2013 Vol. 79 Ed. 6 - (19º)
Artigo de Revisão
Pages: 780 to 788
Comprehensive review of surgeries for obstructive sleep apnea syndrome
Author(s): Macario Camacho1; Victor Certal2; Robson Capasso3
DOI: 10.5935/1808-8694.20130139
Keywords: sleep apnea, obstructive; sleep apnea, obstructive/surgery; snoring; therapeutics.
Abstract:
There are several surgical treatment modalities utilized for obstructive sleep apnea syndrome (OSAS). OSAS can cause excessive daytime sleepiness as well as cardiovascular morbidity and mortality. Patients who fail medical management often seek surgical treatment.
OBJECTIVE: This paper reviews surgical treatment options for obstructive sleep apnea syndrome to include original descriptions as well as outcomes for snoring, apnea-hypopnea indices, and mortality benefits.
METHOD: A literature review was performed for OSAS surgical treatment options for soft tissue and skeletal surgeries. Articles with the original descriptions and surgical reviews are included for each procedure.
RESULTS: A total of twenty-eight surgical treatment modalities for OSAS were identified. Original article authors and year of description were obtained and presented. Polysomnographic data for apnea indices, apnea-hypopnea indices and mortality are presented.
CONCLUSION: There is a large amount of variability in outcomes for sleep surgeries, however, in order to maximize success and cure rates, multiple procedures are most often necessary. Sleep surgeons must get familiar with modern surgical concepts and techniques, and participate in multi-disciplinary care in order to maximize treatment outcomes.
![]()
INTRODUCTION
Obstructive sleep apnea syndrome (OSAS) manifests with excessive daytime sleepiness and affected patients can be treated either medically or surgically1. Continuous positive airway pressure (CPAP) was first described by Sullivan et al. in 1981 as highly efficacious treatment for OSAS2. Although CPAP has high efficacy, the effectiveness of the therapy is limited, as demonstrated by 46%-83% of patients being non-adherent to therapy (defined as > 4 hours of use per night)3. Patients who fail medical management often seek surgical treatment options. There is debate as to the effectiveness of surgical treatment for OSAS. Surgical treatment, guided by proper patient selection, counseling and realistic expectations increases the likelihood of success and patient satisfaction, respectively. The goal of this paper is to review surgical approaches for OSAS treatment.
METHOD
A literature review was performed for adult obstructive sleep apnea syndrome surgical treatment. Titles and abstracts were reviewed to identify surgical treatment modalities. The original study describing each procedure, the studies that contributed significantly and systematic reviews are included in this article. Surgical techniques are described based on sub-site and in the order that they first were described in the literature as treatment for obstructive sleep apnea. The search was performed on MedLine from inception to June 2013. The original articles providing the description of each procedure are presented from the earliest being uvulopalatopharyngoplasty (UPPP) in 1964, to the most recent, which is transoral robotic surgery (TORS) for tongue base reduction in 2010.
Subsequently, the articles describing outcomes for each of the procedures were also reviewed. Articles that contributed substantially were reviewed and were included. As a literature review, this study is exempt from the Stanford IRB protocol review.
RESULTS
The results of the MedLine search yielded the following surgical modalities: uvulopalatopharyngoplasty, tracheostomy, tonsillectomy, mandibular advancement, genioglossus advancement, hyoid suspension, cautery assisted uvuloplasty, maxillomandibular advancement (MMA), laser assisted uvuloplasty (LAUP), midline glossectomy, arytenoid reduction, epiglottectomy, epiglottopexy, epiglottoplasty, transpalatal advancement pharyngoplasty (TAP), cautery-assisted uvulopalatoplasty, cautery-assisted palatal stiffening operation (CAPSO), mandibular distraction, radiofrequency ablation of the soft palate, rapid maxillary expansion (RME)/surgically assisted rapid palatal expansion (SARPE), radiofrequency ablation of the tongue, tongue stabilization/tongue suspension, hypoglossal nerve stimulator/implant (HGNS), nasal surgery, lateral pharyngoplasty, palatal implants, Z-palatoplasty (ZPP), tongue base coblation, submucosal minimally invasive lingual excision (SMILE), expansion sphincter pharyngoplasty and transoral robotic surgery (TORS).
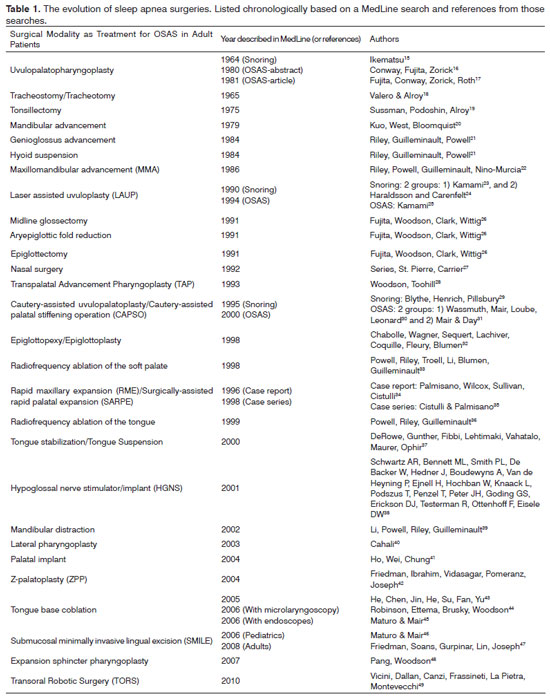
Table 1 chronologically presents surgeries as they appeared on MedLine or the searched articles' references for the original procedural description. In addition, a total of 11 other articles which are systematic reviews, meta-analyses or comprehensive overviews are also included in this review1,4-14.
Nasal surgeries
Series et al. 27 described 20 adults in 1992 who had undergone nasal surgeries, with significant improvement in nasal resistance, but minimal improvement in the respiratory disturbance index (RDI) from 39.8 ± 6.1/h to 36.8 ± 5.9/h. A recent meta-analysis by Li et al. 10, analyzing nine articles with pooled AHI results demonstrating a decrease from 35.2 ± 22.6/h to 33.5 ± 23.8/h, with a total success rate of 16.7%. Although nasal procedures do not have a statistically significant improvement in isolated treatment for OSAS, they do improve nasal breathing and can help improve CPAP compliance and reduce CPAP pressures from a mean of 11.9 down to 9.2 centimeters of water pressure50.
Palatal surgeries
Uvulopalatopharyngoplasty (UPPP)
Ikematsu et al. first began performing uvulopalatopharyngoplasties in 1952, and subsequently published his results of the procedure as treatment of snoring in 196415,51. Over the years, modifications have been described40,42,52. Initial techniques described removal of larger amounts of palatal tissue and subsequently had increased risks for foreign body sensation, dry throat, globus sensation, lower fundamental frequency of speech, problems with phlegm, velopharyngeal insufficiency and nasopharyngeal stenosis53-56. However, newer descriptions have been modified in a manner that re-organizes and preserves tissue52. Systematic reviews of UPPP surgeries have demonstrated wide variability among polysomnography results. Caples et al. 4 pooled data from 15 studies demonstrating a pre-operative AHI of 40.3/h, and post-operative AHI of 29.8/h for a 33% reduction. Elshaug et al. 6 pooled seven studies and demonstrated a 51.5% success rate in providing a 50% reduction in AHI and/or < 20/h6. Franklin et al. 7 assessed complications and found 30 deaths in six studies between 1989 and 2004.
Laser assisted uvuloplasty (LAUP)
Stiffening of the palate was initially described as treatment for snoring, and the procedure was subsequently applied as treatment for sleep apnea23,25. Kamami23, then Haraldsson & Carenfelt24 reported their initial experiences with LAUP in 1990 as a treatment modality that is more easily performed under local anesthetic. , Caples et al. 4 assessed two randomized controlled trials and six observational studies, with a pooled decrease of 32% in the AHI. Elshaug et al. 6 demonstrated a pooled success rate of 48.8% (confidence interval (CI) of 37.6-60). One issue with the LAUP is that patients often require several treatments, Kamami23,25 described that on average patients were treated with 4 individual sessions.
Transpalatal advancement pharyngoplasty (TAP)
Because the results of UPPP procedures were inconsistent, Woodson & Toohill28 developed the TAP as a way to advance the palate anteriorly more consistently. The technique involves a gothic arch incision from posterior to the alveolus with a continuation forward in the palatoglossal fold, the hamulus is exposed and fractured, the posterior hard palate is removed, redundant mucosa is excised and lateral flaps are advanced and sutured to the alveolar mucoperiosteum. The response from the initial study in 6 patients demonstrated a mean decrease from 69.3 ± 32.1/h to 26.6 ± 25.3/h28. Shine & Lewis53 described a modification of the TAP, which utilizes a "propeller incision" which has a lower incidence of oronasal fistula. Shine & Lewis54 compared patients who underwent the traditional gothic arch incision compared to the newer propeller incision and found that there was a 31% improvement in success rate with the propeller incision.
Cautery-assisted uvulopalatoplasty/Cauteryassisted palatal stiffening operation (CAPSO)
Initially described as a simple, inexpensive single stage clinic procedure for snoring, the procedure was subsequently described as treatment for OSAS29-31,55. When performed for snoring treatment, Blythe et al. 29 describe that 83% of spouses reported either resolution or significant improvement in the patients' snoring. Mair & Day31 reported treating 200 consecutive patients over an 18-month period with success rates of 92% initially, and a slight decrease in success down to 77% after 1 year. Wassmuth et al.30 demonstrated a decrease in AHI from 25 ± 12.9/h to 16.6 ± 15.0/h (p = 0.01). Pang and Terris'55 modification involves performing an uvulectomy, removing a horizontal strip of mucosa from the anterior aspect of the soft palate and the creation of vertical trenches in the soft palate bilaterally. The modified CAPSO reports an improvement in their patients' AHI from 12.3/h to 5.2/h (p < 0.05).
Radiofrequency ablation (RFA) of the soft palate
RFA of the soft palate was described by Powell et al. 33 in a group of 22 healthy men in 1998. This initial study demonstrated that the procedure was effective for the treatment of snoring (snoring scores decreased by 77%), an improvement in AHI and only mild patient discomfort. Caples et al. 4 reviewed seven observational studies and showed a mean change in AHI from 23.4/h to 14.2/h. Elshaug et al. 6 demonstrated a 60% success rate in the two studies evaluated (95% CI of 37.6-60).
Lateral pharyngoplasty
Cahali40 described treatment of OSAS by performing a bilateral tonsillectomy, with elevation of the superior pharyngeal constrictor muscle within the tonsillar fossa, superior traction is placed on the upper palatopharyngeus muscle, and a palatine flap is created laterally, a subtotal resection of the palatopharyngeus muscle is made and the flaps are closed in a z-plasty fashion. Results demonstrated an improvement in AHI from 41.2/h to 9.5/h (p = 0.009).
Palatal implants
There was one double-blinded, randomized, placebo-controlled trial which demonstrated a modest reduction in AHI, from 23.8/h to 15.9/h for the palatal implant arm vs. 20.1/h to 21.0/h for the placebo group, demonstrating a statistically significant difference in the two groups, p < 0.00156. Choi et al. 57 pooled data from seven studies and demonstrated a statistically significant reduction in AHI with and a standard mean difference of -0.378; 95% CI of 0.619 to -0.138, p = 0.02. The meta-analysis data also demonstrated a 9.3% extrusion rate.
Z-palatoplasty (ZPP)
The ZPP was described by Friedman et al. 42 for treatment of patients with OSAS who have previously undergone a tonsillectomy. In this technique, the mucosa over the anterior soft palate and uvula are removed, exposing the underlying muscle, followed by bisection of the uvula and inferior soft palate with a cold knife, the flaps are then rotated laterally over the soft palate and are sutured into position. This study demonstrated improved results compared to standard UPPP (25 patients in each arm), with ZPP decreasing AHI from 41.8 ± 26.4/h down to 20.9 ± 19.3/h.
Expansion sphincter pharyngoplasty
Pang & Woodson48 describe a technique in which a horizontal incision is made in the palatopharyngeus muscle (after tonsillectomy), superolateral incisions are made on the soft palate, in the inferior aspect of the palatopharyngeus muscle is then suspended superolaterally. The 45 patients had a BMI < 30 kg/m2, were Friedman stage 2 or 3, Type 1 Fujita and had lateral pharyngeal wall collapse, with an AHI improvement from 44.2 ± 10.2/h to 12.0 ± 6.6/h (p < 0.005).
Tonsillectomy
Whereas, in children there is a significant amount of data; in adults, tonsillectomy studies as treatment for OSAS is limited. Sussman et al. 19 described performing a tonsillectomy in two obese patients who also had significant tonsillar hypertrophy, and had resolution of their sleepiness after the tonsillectomy. One study by Stow et al. 58 of 13 patients who underwent tonsillectomy (11 with additional nasal surgeries) as treatment for OSAS and found a significant reduction in the AHI from 31.7/h to 5.5/h (p = 0.0002). The effectiveness of this procedure is dependent on several factors to include: the anatomy of the patients, the BMI, neck circumference, tongue size, and the anatomical location of the apneic obstruction during sleep.
Tongue
Radiofrequency ablation (RFA) of the tongue
After radiofrequency ablation of the palate had successful outcomes, Powell et al. 36 piloted a study on 18 patients with sleep disordered breathing to assess the effectiveness for the RFA to the tongue in 1999. This study found a mean reduction in AHI from 39.6/h to 17.8/h, with no change in speech or swallowing, and only one infection. Kezirian & Goldberg9 reviewed 11 studies on results of RFA of the tongue and demonstrated a wide range of AHI outcomes, ranging from 20% to 83% successful. Most studies demonstrate decreased daytime hypersomnolence, improved quality of life and improvement in the lowest oxygen saturation.
Tongue stabilization/Tongue suspension
DeRowe et al. 37 described the Repose system in 2000 as a new, minimally invasive procedure in which there is suspension of the base of tongue to reduce tongue-base collapse. This initial study on 16 patients demonstrated a mean RDI improvement from 35/h to 17/h (p = 0.001) and 14 out of 16 bed-partners reported improvement in snoring. Kezirian & Goldberg9 reviewed six studies and found 20% to 57% success rates.
Hypoglossal nerve stimulation
Investigations regarding the physiology of the genioglossus muscle and electrophysiological stimulation began with Guilleminault et al. 59 in 1978. Hypoglossal nerve stimulation studies were later continued by a few groups to include: 1) Fairbanks & Fairbanks60 in 1993, and 2) Eisele et al. 61 in 1997. , In 2001, Schwartz et al. 38 described the pilot study for placement of an implantable device which provides electrical stimulation of the hypoglossal nerve as treatment for OSAS. In this study, a total of eight patients with a mean AHI of 52 ± 20.4/h in NREM and 48.2 ± 0.5/h in REM, demonstrated a decrease down to 22.6 ± 12.1/h in NREM and 16.6 ± 17.1/h in REM (p < 0.001). 38 The current procedure involves placement of an implantable pulse generator, with a respiratory pressure sensor and a stimulation lead, which stimulates the hypoglossal nerve during sleep62.
Tongue base coblation
He et al. 43 studied UPPP with tongue base coblation in 112 patient with OSAS and at 12 months post-operatively and demonstrated 24 patients being cured (21.4%), 52 patients had notable improvement (46.4%), 16 had some improvement (14.2%), and 20 patients had no effect. Robinson et al. 44 described lingual tonsillectomies in 18 patients with massive (N = 10) and modest (N = 8) lingual tonsillar hypertrophy, with moderate pain (7-10 days), a mean of 20 mL of blood loss during the procedure and only two patients requiring revision. Robinson et al. 44 described using microlaryngoscopy with an operating microscope during the procedure, while Maturo & Mair45 in a letter to the editor described coblation lingual tonsillectomy utilizing a rubber bite block and a 70 degree sinus endoscope placed trans-orally, which is the current technique used in many institutions.
Submucosal minimally invasive lingual excision (SMILE)
Maturo & Mair46 described this technique for use in children with good results. The first article to evaluate the effectiveness in adults was Friedman et al. 47, in 2008, in which they demonstrated a 64.6% success rate (p = 0.024), however, there was a higher necessity for narcotic pain control (3.8 ± 3.8 days vs. 2.4 ± 3.5 days) and a longer time to return to a normal diet (4.9 ± 4.5 days vs. 2.9 ± 4.1 days) when compared to patients who underwent radiofrequency ablation of the tongue, respectively.
Transoral robotic surgery (TORS)
In 2010, Vicini et al. 48 described their outcomes utilizing TORS for OSAS. The study reported on 10 patients with a mean preoperative AHI of 38.3/h which decreased to 20.6/h with surgery of the tongue base and epiglottis using the transoral robotic surgery63. Additional studies have demonstrated the effectiveness of TORS for OSA, such as the Friedman et al. 64 2012 publication, which demonstrated a reduction in AHI from 54.6/h to 18.6/h (p < 0.001) and a success rate of 66.7% and cure rate of 18%.
Hyoid suspension
Resistance of airflow is directly proportional to the length of the airway, therefore, a decrease in airway length will provide a decrease in resistance. The decrease in airway length can be accomplished by performing a hyoid suspension, which was described in 1984 by Riley et al. 21. Kezirian & Goldberg9 evaluated 4 studies' data and found that when the hyoid suspension is performed at the same time as another surgery, then there are better outcomes with a 71% successful rate, however, when performed in isolation after previous unsuccessful surgery, then there is a 35% success rate.
Multiple procedures
Because obstructive apneic events during sleep occur in multiple locations in the airway, the treatment options are therefore more successful if those multiple areas of obstruction are addressed, rather than performing single site surgery. A common anatomical site of obstruction is the hypopharyngeal and supraglottic region, therefore, removal or reduction of tissue in this area can help reduce obstructive events. Fujita et al. described the midline glossectomy in 12 patients with simultaneously performed laser lingual tonsillectomy (N = 7), reduction in aryepiglottic folds (N = 10), partial epiglottectomy (N = 5) and all received a temporary tracheostomy. 26 Fujita et al. 26 results demonstrated an RDI decrease from 60.6/h to 14.5/h in responders (42%) and a decrease from 62.6/h to 48.4/h in non-responders (N = 7). As part of this comprehensive review, no studies were identified for isolated aryepiglottic fold reduction or isolated epiglottectomy as treatment for OSAS. Kezirian & Goldberg9 reviewed five studies in which multiple procedures were performed and demonstrated a range of success (25%-83%).
Lin et al. 11 pooled 58 studies in which multiple procedures were performed, with 1,978 patients, mean age of 46.2 years, with a pre-operative AHI of 48/h and found a 60.3% reduction in the AHI, which corresponds to a 66.4% success rate.
Skeletal surgeries
Mandibular advancement
Kuo et al. 20 first described the mandibular advancement surgery in 1979 as treatment for hypersomnia sleep apnea (HSA), which is now called obstructive sleep apnea syndrome (OSAS). They described three cases of traumatically induced mandibular retrognathism which caused sleep apnea with daytime hypersomnia, and each had resolution after the mandibular advancement65. It is the mandibular advancement procedure which was the groundwork for future advancement of the maxillomandibular complex in patients who did not have retrognathia, as treatment for OSAS.
Genioglossus Advancement/Genial Tubercle Advancement (GTA)
This procedure is often combined with other procedures such as a hyoid suspension, or uvulopalatopharyngoplasty. Initially described by Riley et al. 21, in combination with the hyoid suspension as a new treatment for OSAS in a 24 year old male with a BMI of 36.1 kg/m2who had failed previous tonsillectomy and septoplasty. Kezirian & Goldberg9 demonstrated a pooled GTA success rate of > 60%, with the AHI decreasing from 60/h to 29/h. Two key factors influencing the outcomes were preoperative BMI and AHI; demonstrating that those with a BMI < 30 kg/m2 having a 64% success rate compared with BMI > 30 kg/m2 having a 41% success rate. A preoperative AHI < 50/h was successful in 71% of patients, while those with an AHI > 50/h was successful in 32%9.
Maxillomandibular advancement (MMA)
MMA involves the creation of a LeForte 1 osteotomy to the maxilla and a bilateral split sagittal osteotomy to the mandible. This procedure was first described with simultaneously performed hyoid suspension as treatment for OSAS by Riley et al. 22 in 1986. Holty & Guilleminault8 performed a meta-analysis in 2012 demonstrating a mean AHI decrease from 63.9/h to 9.5/h, p < 0.001, with a surgical success rate of 86% and cure rate of 43.2%. It was noted that younger age (45 years), lower preoperative weight and AHI, an increase in posterior airway space > 11.6 mm, a maxillary advancement > 10 mm and a mandibular advancement more than 11.3 mm improved the likelihood of success. Pirklbauer et al. 12 systematic review and analysis of data recommends a grade of A to B with regard to levels of evidence based medicine.
Rapid maxillary expansion (RME)/Surgically-assisted rapid palatal expansion (SARPE)
An initial case report by Palmisano & Cistulli34, followed by a case series by Cistulli et al. 35, has been performed on adults, and demonstrated an improvement in AHI from 19 ± 4/h to 7 ± 4/h. In this study, the patients presented with transverse maxillary insufficiency and the success rate was 90% and the cure rate was 70%35.
Mandibular distraction osteogenesis
There is limited data on mandibular distraction osteogenesis as treatment for OSAS in adults. Li et al. 39 performed mandibular distractions on five healthy adults and after 12 months, found a mean improvement in AHI from 49/h to 7/h. In this study, the distraction osteogenesis advanced the mandibles between 5.5 mm to 12.5 mm, with a mean of 8.1 mm.
Tracheostomy
Valero & Alroy18 demonstrated the effectiveness of tracheostomy (tracheotomy) as treatment for obstructive sleep apnea in a patient with acquired micrognathia (1965). Holty & Guilleminault1 pooled nine studies and found that the apnea index decreased from 88.4/h to 0.5/h (p < 0.001), AHI during REM decreased from 63.8/h to 26.2/h (p < 0.001) and AHI during NREM decreased from 98.9/h to 21.6/h (p < 0.001). Despite the morbidity from the surgery, the patients who have had long term tracheostomies experienced a significant decrease in mortality66,67. Partinen et al. 66 evaluated 198 patients treated with either a tracheostomy (N = 71) or weight loss (N = 127), and had no deaths after five years in the tracheostomy group and 14 deaths in those in the weight loss group. He et al. 67 demonstrated that tracheostomy is equivalent to CPAP at 8 years, with no deaths in these groups during the study period.
DISCUSSION
Despite several different types of surgeries used on an annual basis to treat obstructive sleep apnea syndrome (~35,000/year), the surgeries most often performed in the United States are palatal surgeries, at an estimated 33,000/year68. Other procedures described herein are much less frequently performed, but include hypopharyngeal surgeries (~6500/year), genioglossus advancement (~5100/year), maxillomandibular advancement (~1400/year) and hyoid suspension (~675/year)68. The experience at Stanford has seen the development or application of several techniques for treatment of OSAS to include maxillomandibular advancement, genioglossus advancement, hyoid suspension and radiofrequency ablation, each of which have been modified or expanded by other colleagues around the country and around the world21,22,36. Innovation and technology are also providing improved outcomes as demonstrated by the application of radiofrequency, coblation and transoral robotic surgery33,36. In addition to the challenges of keeping up with the current evidence and technology, there will be patients who fail sleep surgery. In order to maximize success and cure rates, multiple procedures are often necessary. Some patients may fail soft tissue surgeries and may be candidates for either maxillomandibular advancements or tracheostomies1,8.
CONCLUSION
There is a large amount of variability in outcomes for sleep surgeries, however, in order to maximize success and cure rates, multiple procedures are most often necessary. Technology is advancing, and sleep surgeons must keep up with current literature and participate in multi-disciplinary care in order to maximize outcomes for our patients.
REFERENCES
1. Holty JE, Guilleminault C. Surgical options for the treatment of obstructive sleep apnea. Med Clin North Am. 2010;94(3):479-515. PMID: 20451028 DOI: http://dx.doi.org/10.1016/j.mcna.2010.02.001
2. Sullivan CE, Issa FG, Berthon-Jones M, Eves L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. 1981;1(8225):862-5. DOI: http://dx.doi.org/10.1016/S0140-6736(81)92140-1
3. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173-8. DOI: http://dx.doi.org/10.1513/pats.200708-119MG
4. Caples SM, Rowley JA, Prinsell JR, Pallanch JF, Elamin MB, Katz SG, et al. Surgical modifications of the upper airway for obstructive sleep apnea in adults: a systematic review and meta-analysis. Sleep. 2010;33(10):1396-407.
5. Choi JH, Kim SN, Cho JH. Efficacy of the Pillar implant in the treatment of snoring and mild-to-moderate obstructive sleep apnea: a meta-analysis. Laryngoscope. 2013;123(1):269-76. DOI: http://dx.doi. org/10.1002/lary.23470
6. Elshaug AG, Moss JR, Southcott AM, Hiller JE. Redefining success in airway surgery for obstructive sleep apnea: a meta analysis and synthesis of the evidence. Sleep. 2007;30(4):461-7.
7. Franklin KA, Anttila H, Axelsson S, Gislason T, Maasilta P, Myhre KI, et al. Effects and side-effects of surgery for snoring and obstructive sleep apnea--a systematic review. Sleep. 2009;32(1):27-36.
8. Holty JE, Guilleminault C. Maxillomandibular advancement for the treatment of obstructive sleep apnea: a systematic review and meta-analysis. Sleep Med Rev. 2010;14(5):287-97. DOI: http://dx.doi.org/10.1016/j.smrv.2009.11.003
9. Kezirian EJ, Goldberg AN. Hypopharyngeal surgery in obstructive sleep apnea: an evidence-based medicine review. Arch Otolaryngol Head Neck Surg. 2006;132(2):206-13. PMID: 16490881 DOI: http://dx.doi.org/10.1001/archotol.132.2.206
10. Li HY, Wang PC, Chen YP, Lee LA, Fang TJ, Lin HC. Critical appraisal and meta-analysis of nasal surgery for obstructive sleep apnea. Am J Rhinol Allergy. 2011;25(1):45-9. DOI: http://dx.doi.org/10.2500/ ajra.2011.25.3558
11. Lin HC, Friedman M, Chang HW, Gurpinar B. The efficacy of multilevel surgery of the upper airway in adults with obstructive sleep apnea/hypopnea syndrome. Laryngoscope. 2008;118(5):902-8. PMID: 18300704 DOI: http://dx.doi.org/10.1097/MLG.0b013e31816422ea
12. Pirklbauer K, Russmueller G, Stiebellehner L, Nell C, Sinko K, Millesi G, et al. Maxillomandibular advancement for treatment of obstructive sleep apnea syndrome: a systematic review. J Oral Maxillofac Surg. 2011;69(6):e165-76. PMID: 21605790
13. Sarkhosh K, Switzer NJ, El-Hadi M, Birch DW, Shi X, Karmali S. The impact of bariatric surgery on obstructive sleep apnea: a systematic review. Obes Surg. 2013;23(3):414-23. DOI: http://dx.doi.org/10.1007/ s11695-012-0862-2
14. Sher AE, Schechtman KB, Piccirillo JF. The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep. 1996;19(2):156-77.
15. Ikematsu T. Study of snoring, 4th report: therapy. J Jpn Otol Rhinol Laryngol. 1964;64:434-5.
16. Conway W, Fujita S, Zorick F, Roth. Uvulo-palato-pharyngoplasty in treatment of upper airway sleep apnea [ABSTRACT]. Am Rev Respir Dis 1980;121(Suppl):121.
17. Fujita S, Conway W, Zorick F, Roth T. Surgical correction of anatomic azbnormalities in obstructive sleep apnea syndrome: uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg. 1981;89(6):923-34.
18. Valero A, Alroy G. Hypoventilation in acquired micrognathia. Arch Intern Med. 1965;115:307-10. PMID: 14248361 DOI: http://dx.doi.org/10.1001/archinte.1965.03860150051009
19. Sussman D, Podoshin L, Alroy G. The Pickwickian syndrome with hypertrophy of tonsils: a re-appraisal. Laryngoscope. 1975;85(3):565-9. DOI: http://dx.doi.org/10.1288/00005537-197503000-00015
20. Kuo PC, West RA, Bloomquist DS, McNeil RW. The effect of mandibular osteotomy in three patients with hypersomnia sleep apnea. Oral Surg Oral Med Oral Pathol. 1979;48(5):385-92. PMID: 290935 DOI: http://dx.doi.org/10.1016/0030-4220(79)90063-X
21. Riley R, Guilleminault C, Powell N, Derman S. Mandibular osteotomy and hyoid bone advancement for obstructive sleep apnea: a case report. Sleep. 1984;7(1):79-82.
22. Riley RW, Powell NB, Guilleminault C, Nino-Murcia G. Maxillary, mandibular, and hyoid advancement: an alternative to tracheostomy in obstructive sleep apnea syndrome. Otolaryngol Head Neck Surg. 1986;94(5):584-8.
23. Kamami YV. Laser CO2 for snoring. Preliminary results. Acta Otorhinolaryngol Belg. 1990;44(4):451-6. PMID: 2128762
24. Haraldsson PO, Carenfelt C. Laser uvulopalatoplasty in local anaesthesia. A safe approach in the treatment of habitual snoring. Rhinology. 1990;28(1):65-6.
25. Kamami YV. Outpatient treatment of sleep apnea syndrome with CO 2 laser, LAUP: laser-assisted UPPP results on 46 patients. J Clin Laser Med Surg. 1994;12(4):215-9. PMID: 10172096
26. Fujita S, Woodson BT, Clark JL, Wittig R. Laser midline glossectomy as a treatment for obstructive sleep apnea. Laryngoscope. 1991;101(8):805-9. PMID: 1865726 DOI: http://dx.doi.org/10.1288/00005537-199108000-00001
27. Sériès F, St Pierre S, Carrier G. Effects of surgical correction of nasal obstruction in the treatment of obstructive sleep apnea. Am Rev Respir Dis. 1992;146(5 Pt 1):1261-5. PMID: 1443882
28. Woodson BT, Toohill RJ. Transpalatal advancement pharyngoplasty for obstructive sleep apnea. Laryngoscope. 1993;103(3):269-76. PMID: 8441314
29. Blythe WR, Henrich DE, Pillsbury HC. Outpatient uvuloplasty: an inexpensive, single-staged procedure for the relief of symptomatic snoring. Otolaryngol Head Neck Surg. 1995;113(1):1-4. PMID: 7603702 DOI: http://dx.doi.org/10.1016/S0194-5998(95)70137-0
30. Wassmuth Z, Mair E, Loube D, Leonard D. Cautery-assisted palatal stiffening operation for the treatment of obstructive sleep apnea syndrome. Otolaryngol Head Neck Surg. 2000;123(1 Pt 1):55-60. PMID: 10889482
31. Mair EA, Day RH. Cautery-assisted palatal stiffening operation. Otolaryngol Head Neck Surg. 2000;122(4):547-56. PMID: 10740176
32. Chabolle F, Wagner I, Séquert C, Lachiver X, Coquille F, Fleury B, et al. Tongue base reduction with hyoid-epiglottoplasty. A surgical alternative in severe sleep apnea syndromes. Ann Otolaryngol Chir Cervicofac. 1998;115(6):322-31. PMID: 9922828
33. Powell NB, Riley RW, Troell RJ, Li K, Blumen MB, Guilleminault C. Radiofrequency volumetric tissue reduction of the palate in subjects with sleep-disordered breathing. Chest. 1998;113(5):1163-74. PMID: 9596289 DOI: http://dx.doi.org/10.1378/chest.113.5.1163
34. Palmisano RG, Wilcox I, Sullivan CE, Cistulli PA. Treatment of snoring and obstructive sleep apnoea by rapid maxillary expansion. Aust N Z J Med. 1996;26(3):428-9. PMID: 8811226 DOI: http://dx.doi.org/10.1111/j.1445-5994.1996.tb01941.x
35. Cistulli PA, Palmisano RG, Poole MD. Treatment of obstructive sleep apnea syndrome by rapid maxillary expansion. Sleep. 1998;21(8):831-5.
36. Powell NB, Riley RW, Guilleminault C. Radiofrequency tongue base reduction in sleep-disordered breathing: A pilot study. Otolaryngol Head Neck Surg. 1999;120(5):656-64. PMID: 10229589 DOI: http://dx.doi.org/10.1053/hn.1999.v120.a96956
37. DeRowe A, Gunther E, Fibbi A, Lehtimaki K, Vahatalo K, Maurer J, et al. Tongue-base suspension with a soft tissue-to-bone anchor for obstructive sleep apnea: preliminary clinical results of a new minimally invasive technique. Otolaryngol Head Neck Surg. 2000;122(1):100-3. PMID: 10629491
38. Schwartz AR, Bennett ML, Smith PL, De Backer W, Hedner J, Boudewyns A, et al. Therapeutic electrical stimulation of the hypoglossal nerve in obstructive sleep apnea. Arch Otolaryngol Head Neck Surg. 2001;127(10):1216-23. PMID: 11587602 DOI: http://dx.doi.org/10.1001/archotol.127.10.1216
39. Li KK, Powell NB, Riley RW, Guilleminault C. Distraction osteogenesis in adult obstructive sleep apnea surgery: a preliminary report. J Oral Maxillofac Surg. 2002;60(1):6-10. PMID: 11756997 DOI: http://dx.doi.org/10.1053/joms.2002.29049
40. Cahali MB. Lateral pharyngoplasty: a new treatment for obstructive sleep apnea hypopnea syndrome. Laryngoscope. 2003;113(11):1961-8. PMID: 14603056 DOI: http://dx.doi.org/10.1097/00005537200311000-00020
41. Ho WK, Wei WI, Chung KF. Managing disturbing snoring with palatal implants: a pilot study. Arch Otolaryngol Head Neck Surg. 2004;130(6):753-8. DOI: http://dx.doi.org/10.1001/archotol.130.6.753
42. Friedman M, Ibrahim HZ, Vidyasagar R, Pomeranz J, Joseph NJ. Z-palatoplasty (ZPP): a technique for patients without tonsils. Otolaryngol Head Neck Surg. 2004;131(1):89-100. PMID: 15243563 DOI: http://dx.doi.org/10.1016/j.otohns.2004.02.051
43. He M, Chen H, Jin W, He Y, Su Z, Fan Y, et al. Uvulopalatopharyngoplasty and tongue base coblation treat the 112 cases of severe obstructive sleep apnea -hypopnea syndrome. Lin Chuang Er Bi Yan Hou Ke Za Zhi. 2005;19(23):1061-2.
44. Robinson S, Ettema SL, Brusky L, Woodson BT. Lingual tonsillectomy using bipolar radiofrequency plasma excision. Otolaryngol Head Neck Surg. 2006;134(2):328-30. PMID: 16455386 DOI: http://dx.doi.org/10.1016/j.otohns.2005.10.021
45. Maturo SC, Mair EA. Coblation lingual tonsillectomy. Otolaryngol Head Neck Surg. 2006;135(3):487-8. PMID: 16949992 DOI: http://dx.doi.org/10.1016/j.otohns.2006.04.015
46. Maturo SC, Mair EA. Submucosal minimally invasive lingual excision: an effective, novel surgery for pediatric tongue base reduction. Ann Otol Rhinol Laryngol. 2006;115(8):624-30. PMID: 16944662
47. Friedman M, Soans R, Gurpinar B, Lin HC, Joseph N. Evaluation of submucosal minimally invasive lingual excision technique for treatment of obstructive sleep apnea/hypopnea syndrome. Otolaryngol Head Neck Surg. 2008;139(3):378-84. DOI: http://dx.doi.org/10.1016/j.otohns.2008.06.011
48. Pang KP, Woodson BT. Expansion sphincter pharyngoplasty: a new technique for the treatment of obstructive sleep apnea. Otolaryngol Head Neck Surg. 2007;137(1):110-4. PMID: 17599576 DOI: http://dx.doi.org/10.1016/j.otohns.2007.03.014
49. Vicini C, Dallan I, Canzi P, Frassineti S, La Pietra MG, Montevecchi F. Transoral robotic tongue base resection in obstructive sleep apnoea-hypopnoea syndrome: a preliminary report. ORL J Otorhinolaryngol Relat Spec. 2010;72(1):22-7. DOI: http://dx.doi.org/10.1159/000284352
50. Poirier J, George C, Rotenberg B. The effect of nasal surgery on nasal continuous positive airway pressure compliance. Laryngoscope. 2013; April 10. [Epub ahead of print] DOI: http://dx.doi.org/10.1002/ lary.24131
51. Crestinu JM. Intrapalatine resection (IPR) in the treatment of sleep apnea and snoring. Plast Reconstr Surg. 1991;87(3):467-9. PMID: 1998017 DOI: http://dx.doi.org/10.1097/00006534-199103000-00011
52. Powell N, Riley R, Guilleminault C, Troell R. A reversible uvulopalatal flap for snoring and sleep apnea syndrome. Sleep. 1996;19(7):593-9.
53. Shine NP, Lewis RH. The "Propeller" incision for transpalatal advancement pharyngoplasty: a new approach to reduce post-operative oronasal fistulae. Auris Nasus Larynx. 2008;35(3):397-400. PMID: 18029127 DOI: http://dx.doi.org/10.1016/j.anl.2007.09.001
54. Shine NP, Lewis RH. Transpalatal advancement pharyngoplasty for obstructive sleep apnea syndrome: results and analysis of failures. Arch Otolaryngol Head Neck Surg. 2009;135(5):434-8. PMID: 19451461 DOI: http://dx.doi.org/10.1001/archoto.2009.45
55. Pang KP, Terris DJ. Modified cautery-assisted palatal stiffening operation: new method for treating snoring and mild obstructive sleep apnea. Otolaryngol Head Neck Surg. 2007;136(5):823-6. PMID: 17478223 DOI: http://dx.doi.org/10.1016/j.otohns.2006.11.014
56. Friedman M, Schalch P, Lin HC, Kakodkar KA, Joseph NJ, Mazloom N. Palatal implants for the treatment of snoring and obstructive sleep apnea/hypopnea syndrome. Otolaryngol Head Neck Surg. 2008;138(2):209-16. PMID: 18241718 DOI: http://dx.doi.org/10.1016/j.otohns.2007.10.026
57. Choi JH, Kim SN, Cho JH. Efficacy of the Pillar implant in the treatment of snoring and mild-to-moderate obstructive sleep apnea: a meta-analysis. Laryngoscope. 2013;123(1):269-76. DOI: http://dx.doi.org/10.1002/lary.23470
58. Stow NW, Sale PJ, Lee D, Joffe D, Gallagher RM. Simultaneous tonsillectomy and nasal surgery in adult obstructive sleep apnea: a pilot study. Otolaryngol Head Neck Surg. 2012;147(2):387-91. DOI: http://dx.doi.org/10.1177/0194599812444256
59. Guilleminault C, Hill MW, Simmons FB, Dement WC. Obstructive sleep apnea: electromyographic and fiberoptic studies. Exp Neurol. 1978;62(1):48-67. PMID: 729676 DOI: http://dx.doi.org/10.1016/00144886(78)90040-7
60. Eisele DW, Smith PL, Alam DS, Schwartz AR. Direct hypoglossal nerve stimulation in obstructive sleep apnea. Arch Otolaryngol Head Neck Surg. 1997;123(1):57-61. PMID: 9006504 DOI: http://dx.doi.org/10.1001/archotol.1997.01900010067009
61. Fairbanks DW, Fairbanks DN. Neurostimulation for obstructive sleep apnea: investigations. Ear Nose Throat J. 1993;72(1):52-4.
62. Kezirian EJ, Boudewyns A, Eisele DW, Schwartz AR, Smith PL, Van de Heyning PH, et al. Electrical stimulation of the hypoglossal nerve in the treatment of obstructive sleep apnea. Sleep Med Rev. 2010;14(5):299-305. DOI: http://dx.doi.org/10.1016/j.smrv.2009.10.009
63. Vicini C, Frassineti S, La Pietra MG, De Vito A, Dallan I, Canzi P. Tongue Base Reduction with Thyro-Hyoido-Pexy (TBRTHP) vs. Tongue Base Reduction with Hyo-Epiglottoplasty (TBRHE) in mild-severe OSAHS adult treatment. Preliminary findings from a prospective randomised trial. Acta Otorhinolaryngol Ital. 2010;30(3):144-8.
64. Friedman M, Hamilton C, Samuelson CG, Kelley K, Taylor D, Pearson-Chauhan K, et al. Transoral robotic glossectomy for the treatment of obstructive sleep apnea-hypopnea syndrome. Otolaryngol Head Neck Surg. 2012;146(5):854-62. DOI: http://dx.doi.org/10.1177/0194599811434262
65. Berger KI, Fagondes SC, Giugliani R, Hardy KA, Lee KS, McArdle C, et al. Respiratory and sleep disorders in mucopolysaccharidosis. J Inherit Metab Dis. 2013;36(2):201-10. DOI: http://dx.doi.org/10.1007/s10545-012-9555-1
66. Partinen M, Jamieson A, Guilleminault C. Long-term outcome for obstructive sleep apnea syndrome patients. Mortality. Chest. 1988;94(6):1200-4. DOI: http://dx.doi.org/10.1378/chest.94.6.1200
67. He J, Kryger MH, Zorick FJ, Conway W, Roth T. Mortality and apnea index in obstructive sleep apnea. Experience in 385 male patients. Chest. 1988;94(1):9-14. DOI: http://dx.doi.org/10.1378/chest.94.1.9
68. Kezirian EJ, Maselli J, Vittinghoff E, Goldberg AN, Auerbach AD. Obstructive sleep apnea surgery practice patterns in the United States: 2000 to 2006. Otolaryngol Head Neck Surg. 2010;143(3):441-7. PMID: 20723785 DOI: http://dx.doi.org/10.1016/j.otohns.2010.05.009
1. MD (Consulting Assistant Professor Department of Otolaryngology - Head and Neck Surgery Sleep Surgery)
2. MD (Department of Otorhinolaryngology, Hospital Sao Sebastiao, Sta Maria da Feira, Portugal CINTESIS - Center for Research in Health Technologies and Information Systems,
University of Porto, Portugal)
3. MD (Assistant Professor Department of Otolaryngology - Head and Neck Surgery Sleep Surgery Division Stanford Hospital and Clinics, Stanford, CA, USA)
Stanford Hospitals and Clinics, Stanford, CA.
Send correspondence to:
Macario Camacho
MD Consulting Assistant Professor Department of Otolaryngology - Head and Neck Surgery Sleep Surgery Division 2nd floor
Stanford Hospital and Clinics 450 Broadway
St. Redwood City, CA 94063
Ph: 650-723-6601, fax: 650-721-3448
E-mail: drcamachoent@yahoo.com
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on September 4, 2013;
and accepted on September 22, 2013. cod. 11101.