Year: 2002 Vol. 68 Ed. 4 - (16º)
Artigo Original
Pages: 552 to 556
The use of Picibanil (OK-432) for treatment of lymphangioma in the head and neck
Author(s):
Francisco V. Mello-Filho 1,
Luiz G. Tone 2,
Leonardo S. Kruschewsky 3
Keywords: Picibanil, lymphangioma, cystic higroma, cystic lymphangioma
Abstract:
Introduction and Aim: Head and Neck Lymphangiomas (HNL) are generally large in volume, surrounding important anatomical structures. As a current treatment, surgical removal is associated with special risk of aesthetic deformity and functional damage. This medical group studied the sclerosing effects of OK-432 therapy as an alternative treatment for HNL in children. Material and Method: Retrospective study of six children patients with diagnosis of HNL treated by picibanil injection at HC-FMRP-USP from 1997 to 2001. It was studied the following HNL characteristics: dimension, type of HNL and aspirated volume. We studied the time between and number of picibanil injections, the patient's evolution, complications and final results. Results: It was found diameter variation from 8 to 15 cm, with the macro cystic been the most frequent type of cystic higroma, the volume aspirated varied from 2 to 60 ml. The number of injections varied from one to five and the time interval between the injections from one month to one year. All patients experienced tumoral mass regression with total regression occurring in three patients. The only side effect registered was fever, mean of 38º Celsius degrees, happened in all patients. Conclusion: OK 432 is a safe drug and can be used as first treatment choice in HNL.
![]()
Introduction
Lymphangiomas are malformations of lymphatic tissue with widely variable distribution, size and characteristics, despite the fact that 75% of the lymphangiomas are head and neck lymphangiomas (HNL) normally of great proportions1. It is estimated that about 50 to 60% of the lymphangiomas are present at birth and approximately 80 to 90% manifest within the end of the second year of life2.
Even though HNL are congenital cystic benign lesions they may cause severe cosmetic deformities, as well as impairment of airways and digestive tract. The preferred treatment for HNL is surgical exeresis, which has the following disadvantages: technical difficulty to dissect the thin cystic walls, high rate of vascular-nervous lesions, high rate of recurrence and esthetical and functional deformities. These issues have encouraged the search for an alternative treatment to HNL.
Some authors demonstrated very promising results and series with the use of intratumor OK-432 in HNL 3-5. OK-432 (Picibanil, Chugai Pharmaceuticals Co, Tokyo, Japan) is a lyophilized mixture of group A Streptococcus pyogenes, type 3, human origin, treated with benzyl penicillin. The action mechanism of OK-432 has not been well defined as a sclerosing agent; it is known that anaphylotoxins and chemotactic factors cause an inflammation reaction, determining exchange of cell populations, activating natural killer cells, cytokines and production of interleukins that act on the endothelium causing involution of the lymphangioma 6.In order to avoid surgical treatment, which is potentially mutilating, we evaluated the efficiency of sclerosing OK-432 in the treatment of HNL.
Material and Method
We studied six cases retrospectively. There were six children with diagnosis of HNL who were treated in our institution with OK-432 between 1997 and 2001, the pioneers in Brazil. Patients in the study were identified numerically, including sex and age at the beginning of treatment. Diagnosis was based on clinical characteristics of patients and the following exams: ultrasound (US), computed tomography scan (CT), and/or magnetic resonance imaging (MRI). Therefore, we noticed and compared objectively the dimensions of the HNL during treatment with OK-432.
Thanks to imaging studies, HNL were classified concerning dimensions of the tumor, as well as dimensions of each cyst inside them. As to global dimension of tumors, we determined the larger diameter and the cyst dimensions, we classified the morphology as macrocystic, when there was predominance of cysts with diameter greater than 2 cm in the overall volume of the lesion, microcystic when there was predominance of cysts with diameter below 2cm in the overall volume of the lesion, and mixed, when it was impossible to determine the real predominance of the cyst sizes.
We quantified the aspirated volume of the HNL of each sclerosing sessions performed and the dates. We noticed the number of applications of OK-432 and the intervals of time, progression, events and final result.
For intratumor application of OK-432 we followed the method below: after careful assessment with US and/or MRI and/or CT, we identified the largest cyst of the HNL. While the child was awaken and immobilized, we introduced gauge 23 needle (coupled to a catheter, BD Asepto) into the cysts, aspirated into a 20ml syringe its content, which was measured and disposed. We then prepared a solution of 0.1mg of OK-432 diluted in sterile solution at 0.9% in the same volume of the aspirated content, provided that it did not exceed 20ml volume. Without removing the needle from inside the punched cyst, we started the infusion of OK-432 solution replacing the removed volume. When the aspirated volume of HNL was greater than 20ml, we injected only 20ml of OK-432 solution. At the end, the child was hospitalized to follow up occasional side effects.
Figure 1. Patient 3 with head and neck lymphangioma before treatment with OK-432 in frontal view.
Figure 2. Patient 3 with head and neck lymphangioma before treatment with OK-432 in lateral view.
Figure 3. Clinical aspect of patient 3 after one year of treatment with picibanil, frontal view.
Figure 4. Clinical aspect of patient 3 after one year of treatment with picibanil, lateral view.
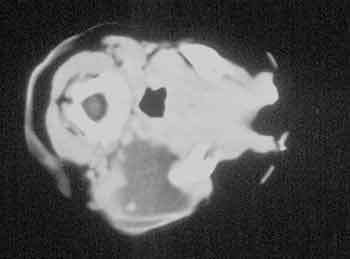
Figure 5. CT scan of patient 3 before treatment with 0K-432.
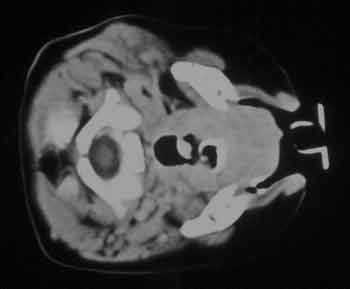
Figure 6. CT scan of patient 3 after treatment with 0K-432.
Results
We present the clinical aspect of patient 3 before treatment with OK-432. HNL occupied practically the whole cervical region on the right, reaching also part of the face, close to the mandible, producing deformities of the right labial commissure (Figure 1). In profile, it was possible to notice that HNL had reached the inferior portion of the parotid gland, elevating the earlobe (Figure 2). In Figures 3 and 4, we observed the clinical aspect, front and lateral position, respectively, of child 3 after two applications with OK-432. We can notice complete remission of the lesion without manifesting sequelae on the face or neck.
In Figure 5, we presented the aspect of the CT section before treatment with OK-432 in patient 3. We can observe in this Figure how precise the limits of HNL are, so it is possible to precisely determine diameters of the tumor and the size of the cysts inside it. In Figure 6, we observed in the same CT scan section the results obtained one year after the use of two applications of OK-432. The results of this study are summarized in Table 1.Table 1. Identification, classification, treatment, evolution and results obtained in six patients treated with OK-432.
Number, identification of patient; Sex, patients' sex; Age, age at beginning of treatment, being y (year) and m (months); Type, type of cyst classified as macro (macrocystic), micro (microcystic) or mixed; Number-Volume, number of applications and volume aspirated from HNL in each session; Date-Diameter, date of each application of OK-432 and larger diameter of HNL found in each session; Interval, interval between applications; Result the final result obtained, classified as total or partial remission.
Discussion
HNL is a not very common congenital lymphatic malformation that has great variety of shapes, sites and behaviors, leading to various names and attempts to classify it. The most common names are: lymphangioma, lymphangioma cyst, lymphatic malformation, hygroma, cystic hygroma and hygroma cyst. Among these names, we adopted the term head and neck lymphangioma, since we studied this type of affection located on the neck and head region. As to classification of HNL, Serres2 suggested to divide them topographically into supra-hyoid and infra-hyoid; other studies3-6 preferred to classify HNL according to size of lymphatic vessels in microcystic and macrocystic, when predominates the quantity of smaller and larger than 2cm lymphatic vessels, respectively, and mixed, when it is not possible to determine which type of cyst is predominant. As to size of lymphatic vessel, we prefer to adopt the nomenclature of macro/microcystic and mixed, because we consider it easier and more reliable. Some authors 3-5 mentioned that this classification could help in the prognosis of HNL, since the lesions classified as macrocystic are those that present the best results with the use of OK-432. In our reduced sample, this fact was confirmed in patients 1, 3 and 5, who presented total regression of HNL, however patients 2 and 4 also presented macrocystic type and experienced partial regression. This result, however, can change because patients 2 and 4 received only 3 and one applications, respectively, so it means they can receive other applications and experience complete local remission. Curiously, the only patient classified as mixed type, patient 6, received one application of OK-432 and presented total regression of the lesion.
Some studies2 refer that treatment of HNL is a challenge because of the potential of recurrent infection, upper airway impairment, swallowing difficulties and interference in normal speech development. The six children treated by us presented bulky tumors (Table 1) that caused major deformities, however in no cases did we notice impairment of airways or digestive tract. We were highly concerned about the risk of causing respiratory or digestive obstruction in these children because we knew that OK-432 produced an inflammatory process that led to increase in tumor volume, however, we could not predict how big they would be. Therefore, all children were hospitalized to be observed and to be submitted to tracheal intubation, tracheostomy or nasogastric tube placement, if necessary. To our surprise, no children needed any of these measures - there was always mild and progressive increase in tumor volume, during two or three days, followed by slight local hyperemia, and it was maintained for a variable period, ranging from 4 to 7 days, without causing any respiratory or swallowing disorders. After this period, there were no more phlogistic signs and the children were discharged. The only event observed in all children was fever at 38-39O C starting as of six hours after the application of OK-432 and it lasted from 2 to 4 days.
Spontaneous regression of HNL is rare, however it is possible to have an intermittent and quick increase of lesions caused by trauma and infection. The recovering endothelium of these lesions is vulnerable to infections and chemicals and the infection can result in spontaneous reduction of size of HNL, but it is a rare occurrence6. In our study, the age of children when they started treatment ranged from 45 days to 11 years and in 4 children they were about 2 years of age (Table 1) and there were no cases of spontaneous regression.
Response to treatment with OK-432 is an enigmatic issue. Some cases are apparently similar, but response to treatment can be very different. We assessed items such as size, volume of aspirated liquid and type of HNL, as well as number and interval between applications (Table 1) in search for prognostic factors. As to tumor size, all children presented bulky tumors but the response to treatment varied a lot from child to child and even in the same child. We had one patient that did not respond to the first application and later presented good response to the remaining applications, patients with progressive responses and patients with total regression after one single application. As to aspirated volume, we did not identify any relation with response to treatment. The interval between applications of OK-432 was another undefined issue; Ogita4 suggested in his study applications of OK-432 every 3 to 6 weeks up to total remission of HNL. It was also successfully tried to have a 14-day interval, when there was no inflammatory response after the injection5. In our study, owing to various factors, there was great variation of time intervals between applications (Table 1), but it was not possible to draw any conclusion.
Conclusion
Despite the small sample, we believe that it is important to show our preliminary results with the pioneer use of OK-432 in Brazil. We observed in all patients of the study a total or partial regression of the HNL, without complications. We concluded that OK-432 is a safe, effective drug that can be used as a first choice approach for the treatment of HNL.
Acknowledgment
To Professor Antonio Carlos dos Santos, Coordinator of the Division of Radiology, HC-FMRP-USP, for his valuable contribution.
References
1. Greinwald JH, Burke DK, Sato Y, Poust RI, Kimura K, Bauman NM, Smith JH. Treatment of lymphangiomas in Children: an update of picibanil (OK 432) sclerotherapy. Otolaryngology - Head and Neck Surgery 1999;121: 381-7.
2. Luzzatto C et al. Sclerosing treatment of lymphangiomas with OK-432. Arch Dis Child 2000; 82:316-8.
3. Mikhail M et al. Sclerosing of recurrent lymphangiomas using OK-432. J Pediatr Surg 1995;1159-60.
4. Ogita S, Tsuto T, Nakamura K, Deguchi E, Iwai N. Therapy in 64 patients with lymphangioma. J Pediatr Surg 1994;29:784-5.
5. Ogita S, Tsuto T, Nakamura K, Deguchi E, Tokiwa K, Iwai N. OK-432 Therapy for lymphangioma in children: why and how does it work? J Pediatr Surg 1996;31:477-80.
6. Serres LM, Sie KCY, Richardson MA. Lymphatic malformations of the head and neck. A proposal for staging. Arch Otolaryngol Head Neck Surg 1995;121:577-82.
[1] Ph.D., Professor of the Discipline of Head and Neck Surgery, Department of Ophthalmology, Otorhinolaryngology and Head and Neck Surgery, HC FMRP-USP.
[2] Ph.D., Professor of the Discipline of Pediatric Oncology, Department of Pediatrics, HC FMRP-USP.
[3] Assistant Physician, Discipline of Head and Neck, Department of Ophthalmology, Otorhinolaryngology and Head and Neck Surgery, HC FMRP-USP.
Affiliation: Hospital das Clinicas, Medical School of Ribeirão Preto-USP.
Address correspondence to: Francisco Veríssimo de Mello-Filho, Rua Salvador Delloiagono, 70
Tel. (55 11) 602.2801/2353 - Fax (55 11) 602 2860 - E-mail:fdmfilho@yahoo.com
Awarded as Best Free Communication, VIII Fórum de Pesquisa Básica e Clínica em Câncer de Cabeça e Pescoço, June 28, 2001.