Year: 2013 Vol. 79 Ed. 4 - (9º)
Artigo Original
Pages: 446 to 453
Mastoid surface area-to-volume ratios in adult brazilian individuals
Author(s): Marco Antônio Rios Lima1; Luciano Farage2; Maria Cristina Lancia Cury3; Fayez Bahmad Júnior4
DOI: 10.5935/1808-8694.20130080
Keywords: anatomy; mastoid; middle ear ventilation; tomography.
Abstract:
Computed tomography-based measurements of mastoid surface area and volume have not been described for adult Brazilian individuals. These measurements add to the understanding of middle ear physiology, related diseases, and their impact on mastoid pneumatization.
OBJECTIVE: To check the ratio between mastoid surface area and volume.
METHOD: This contemporary cross-sectional cohort study included 28 patients submitted to CT imaging of the mastoid. Measurements of surface area and volume were made based on serial CT scans and produced with the aid of software package Image Pro Plus.
RESULTS: Mastoid volumes ranged from 5.5 to 72.4 cm3. Surface areas ranged from 43.9 to 525.2 cm2. Surface areas varied linearly with volumes.
CONCLUSION: Mastoid surface areas and volumes of adult Brazilian subjects followed a linear correlation, as also described in studies carried out in other countries. Mean surface areas and volumes were higher than previously published, unlike surface area-to-volume ratios, which were lower. Further studies with larger populations will provide evidence as to whether Brazilian subjects have larger surface areas and volumes than other populations.
![]()
INTRODUCTION
The middle ear cleft is divided by the tympanic isthmus into anterior-inferior and posterior-superior compartments. The anterior-inferior compartment's main role is clearance, and it includes the protympanum, the mesotympanum, and the hypotympanum. The posterior-superior compartment comprehends the epitympanum and the retrotympanum, the aditus ad antrum and the antrum mastoideum, and the mastoid air cell system; it is primarily devoted to gas exchange. Both compartments are lined by the same respiratory mucosa. Gas exchanges are carried out through the air cell mucosa. Therefore, the total mucosal surface area has direct impact on gas exchange rates1.
The mastoid air cell system accounts for most of the volume of the middle ear cleft and, consequently, for most of the mucosa available for gas exchange2.
The role of the mastoid is yet to be clarified, despite the many theories on the matter. One of the main hypotheses states that the mastoid works as a gas reservoir used to compensate for pressure variations inside the middle ear together with the eustachian tube2-5. According to Magnuson, the mastoid air cell system works as a thermal insulant to protect the middle ear against temperature fluctuations5. Others have described the mastoid as a no longer useful vestige of mammal evolution6.
Computed tomography (CT) is the best method to assess mastoid pneumatization7,8. Various studies have looked into the volume of the adult mastoid, but few have considered the surface area of the mastoid. The latter is an important parameter in middle ear gas exchange through the mucosa9. The measurement of mastoid surface area and volume is relevant for the understanding of middle ear physiology and diseases, as it bears direct impact on mastoid pneumatization.
This study aimed to measure the surface area and volume of the mastoid using computed tomography scans of the temporal bones of adult Brazilians. Such measurements have not been described for Brazilian populations to date. Comparisons against data published in other countries are also included. Based on previous publications, the authors postulated that surface area and volume are linearly correlated8,10.
METHOD
This is a contemporary cross-sectional cohort study. Twenty-eight individuals without history of pediatric chronic otitis media or ear surgery were enrolled from a prospective study on the correlation between mastoid pneumatization and middle ear barotrauma in patients submitted to hyperbaric oxygen therapy.
All individuals gave informed consent and were informed of the risks inherent to their participation in the study. This study was approved by the Research Ethics Committee of the Brasília Armed Forces Hospital.
The subjects underwent bilateral pneumatic otoscopy and tympanometry to document healthy middle ears. Temporal bone CT scans were ordered for all patients.
Mastoid CT scans were taken with a 64-channel Lightspeed VCT (GE Healthcare, Milwaukee, WI, EUA) device, using a volume acquisition protocol with slices of 0.625 mm and slice intervals of 0.31 mm with a bone filter. Scans were produced in the axial view. Pixels measured 0.39 mm2.
The images were reprocessed on Osirix 64 with a reduced area of interest in slices of two millimeters, without excluding portions of the mastoid. All measurements were carried out in the same window, using a window level of 385 Hounsefield units (HU) and a window width of 3155 HU. Scans were saved on JPG format. Patient names were removed and the images were named after letters of the alphabet (A, B, C...) and categorized into right or left side scans.
A radiologist with 10 years of practical experience blinded for clinical data was called to assess the CT scans.
Surface and volume calculations were carried out using software package Image Pro Plus 6.0. The process used to analyze the scans included the following steps: tracing of the area of interest comprehended within the borders of the mastoid air cell system, including isolated cells and excluding the middle ear (the view showing the incudomalleolar joint was defined as the standard plane and the middle ear was considered to be located five planes below); stress poorly-defined borders of the air-bone gap when needed using tool Higauss (one use per slice); apply color mask on air cells to color them white and color bone or soft tissue black; calculate perimeter (cm) and area (cm2) of the region of interest for each slice; add the results from each slice per ear.
The area of each mastoid was calculated by multiplying the result of the summation of the perimeters of each slice by 0.2 cm (slice interval). The volume (cm3) of each mastoid was calculated by multiplying the result of the summation of the areas of each slice by 0.2 cm (slice interval). The analysis was carried out twice by the same researcher, who calculated the mean values found after two verifications of areas and volumes to use them as the final measurements. After the analysis was completed, the researcher was given the key to know the match between letters of the alphabet and patient data.
The procedure described above was also used in two previous studies to verify mastoid surface area and volume in adults8,10. As in the study published by Park et al.8, only normal mastoids were included.
Parametric statistical tests were used due to the normal distribution pattern of the data. Linear regression was used to determine the correlations between (1) right and left mastoid volumes, (2) right and left mastoid surface areas, and (3) mastoid surface areas and volumes.
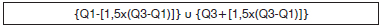
The database was built based on Excel®. Statistical analysis was carried out with software package SPSS 13® (Statistical Package for the Social Sciences, Chicago, IL) for Windows®. Initially, the distribution of surface area and volume data points for each ear was analyzed. Outliers were identified based on interquartile range. According to this criterion, outliers reside outside the range defined by the following formula:
Comparisons between mean values were carried out with Student's t-test for independent measurements (gender comparisons) or repeated measurements (right mastoid vs. left mastoid). Asymmetry analysis was based on the t-test for one sample, using zero as a test value (absence of asymmetry). Correlation tests (Pearson's) were carried out between variables measured through CT scans. The figures represent the values for each subject, the linear adjustment line, and the confidence intervals for the mean. Statistical significance was set at 5% (p < 0.05). All tests were two-tailed. Data was presented in the form of mean ± standard deviation (SD).
RESULTS
Twenty-eight patients, 20 males (71.4%) and eight females (28.6%), with a mean age of 53 years (17 to 78 years) were enrolled in the study. No statistically significant differences were seen between the ages of male and female subjects (mean difference = 5.35 years; p = 0.471).
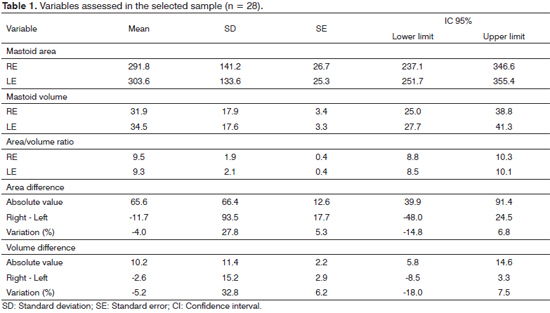
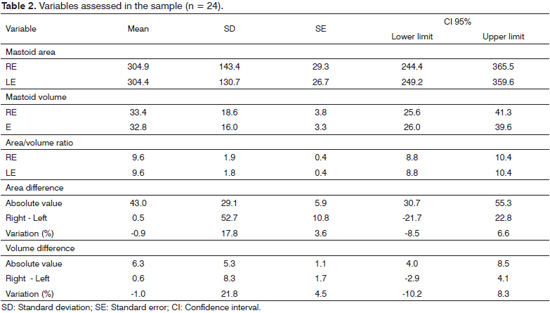
Four participants had two or more variables categorized as outliers. Tables 1 and 2 show the descriptive measurements of the variables analyzed in the study with the entire sample (n = 28) and with outliers excluded (n = 24). No difference was found between right and left mastoid surface areas or volumes.
When the entire sample was considered (n = 28), the right and left mastoid volumes were 31.9 ± 17.9 cm3 (5.5 to 72.4) and 34.5 ± 17.6 cm3 (6.2 to 68) respectively (p = 0.4; Student's t-test for paired samples). Right and left mastoid surface areas were 291.8 ± 141.2 cm2 (43.9 to 525.2) and 303.6 ± 133.6 cm2 (45 to 520.4) respectively (p = 0.56). The surface area-to-volume ratios for the right and left mastoids were 9.5 ± 1.9 cm-1 (6.8 to 13.7) and 9.3 ± 2.1 cm-1 (5 to 13.8) respectively (p = 0.32). The correlation ratios for surface area and volume for the left and right mastoids were 0.88 and 0.92 respectively, yielding a global ratio (all mastoids considered) of 0.9 (Table 1).
In the sample net of outliers (n = 24), the right and left mastoid volumes were 33.4 ± 18.6 cm3 (5.5-72.4) and 32.8 ± 16 cm3 (6.1 to 66.9) respectively (p = 0.71; Student's t-test for paired samples). Right and left mastoid surface areas were 304.9 ± 143.4 cm2 (43.9 to 525.2) and 304.4 ± 130.7 cm2 (44.9 to 469.8) respectively (p = 0.96). The surface area-to-volume ratios for the right and left mastoids were 9.6 ± 1.9 cm-1 (6.8 to 13.7) and 9.6 ± 1.8 cm-1 (6.9 to 13.8) respectively (p = 0.91). The correlation ratios for surface area and volume for the left and right mastoids were 0.9 and 0.92 respectively, yielding a global ratio (all mastoids considered) of 0.91 (Table 2).
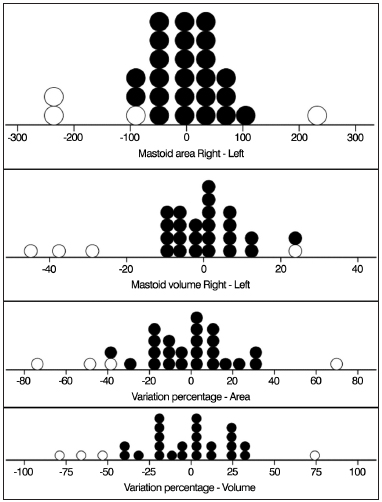
In order to better describe asymmetry measurements (differences of surface area and volume), Figure 1 shows individual values. Negative values mean greater values for left ears and positive values mean greater values for right ears. The mean difference between surface area or volume values for right and left mastoids was not significantly different from 0 (p > 0.376 in all cases). This analysis was carried out for the entire sample (n = 28) and for the sample with outliers excluded (n = 24).
Figure 1. Distribution of asymmetry values measured in the sample. Outliers are represented by open circles (n = 28).
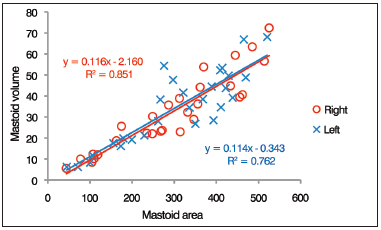
Figure 2 shows the surface areas of right and left mastoids as a function of their respective volumes (n = 28). A linear correlation was found between mastoid surface area and volume. For left and right ears, 76% and 85% of the variance in mastoid surface area was explained by the volume regressions respective of each ear.
Figure 2. Distribution of individual surface area-to-volume ratios. The lines represent the linear regression of the data for each ear as defined by the formula presented in the graph (n = 28).
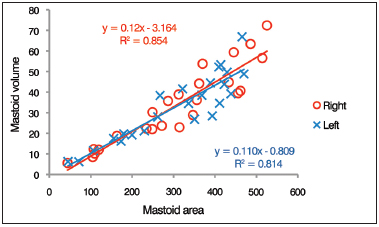
Figure 3 shows the surface areas of right and left mastoids as a function of their respective volumes (n = 24). A linear correlation was found between mastoid surface area and volume. For left and right ears, 81% and 85 % of the variance in mastoid surface area was explained by the volume regressions respective of each ear.
Figure 3. Distribution of individual surface area-to-volume ratios. The lines represent the linear regression of the data for each ear as defined by the formula presented in the graph (n = 24).
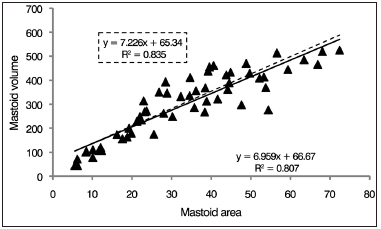
Figure 4 shows the surface areas of all mastoids as a function of their volumes. A linear correlation was found between mastoid surface area and volume. For all ears (n = 28), 80% of the variance in mastoid surface area was explained by volume regressions. In the sample net of outliers (n = 24), the value was 83%.
Figure 4. Distribution of individual surface area-to-volume ratios. The lines represent the linear regression of the data for each ear as defined by the formula presented in the graph. The traced line and the formula highlighted by the traced line represent the values calculated for the sample without outliers (n = 28).
DISCUSSION
The eustachian tube, the tympanic cavity, and the mastoid are part of a complex system in which various mechanisms are combined to ensure proper middle ear ventilation9. Measurements of surface area and volume are of great importance in the study of mastoid physiology and pathogenesis. The area used for gas exchange is directly related to the mucosal surface area. Nonetheless, mucosal surface may be underestimated, as CT scans cannot detect the numerous folds present in the mucosa of the mastoid5. Therefore, normal and altered (ossified or opacified) mastoids may have different gas exchange capabilities despite equal measurements of surface area and volume as inferred from CT scans.
Many authors have described correlations between poor mastoid pneumatization and diseases of the middle ear11,12. However, there is no consensus as to whether people with smaller mastoid volumes would be at greater risk of having middle ear disease, or if middle ear diseases could hamper the development of the mastoid air cell system13.
The main discussion regarding the role of the mastoid is centered on whether the mastoid works as a gas reservoir. Most authors believe the mastoid works as a gas reservoir, acting passively to counteract pressure fluctuations in the middle ear together with the eustachian tube1-4,14. Others have refuted this idea6,15,16. Some authors believe the mastoid has an active two-way role in gas and fluid exchange5,17, despite the lack of significant experimental evidence2. Many experimental models have been tried, limited by blood perfusion and gas diffusion, but their results have been contradictory14-16.
The degree of mastoid pneumatization has been assessed through various methods: immersion in fluid, Boyle's law, acoustics, and imaging18,19. Due to the difficulty accessing mastoid pneumatization directly, imaging has been the most frequently used method. Temporal bone CT scans provide more accurate assessments of mastoid volumes than temporal bone X-rays7,8.
Coulhon et al.20 found a good correlation between mastoid pneumatization estimated by X-rays using the planimetric approach and mastoid volume calculated from CT scans (r = 0.95). Conversely, Todd et al.7 found more modest correlation ratios between X-rays and CT scans (r = 0.57-0.74). Temporal bone X-rays are reliable when patients of similar ages are compared, but they cannot be used to assess actual or air mastoid volumes or surface areas9.
Only a few Brazilian authors have quantitatively looked into mastoid pneumatization21,22. Albernaz21 analyzed 100 pairs of temporal bones of mostly Brazilian individuals and assessed the value of the occipital position in the radiographic study of the mastoid. The author compared right and left mastoids and found identical pneumatization on both sides in 82 % of the pairs, relative agreement between both sides in 17%, and absolute disagreement in 1% of the cases. However, the author did not report absolute values of mastoid surface area. Bento et al.22 correlated mastoid pneumatization on X-rays to graft take in 80 patients with chronic otitis media submitted to type I tympanoplasty. The authors reported a mean mastoid surface area of 7.62 cm2 (1.82 to 27.4). We believe this is the first Brazilian study to report measurements of mastoid surface area and volume verified with CT.
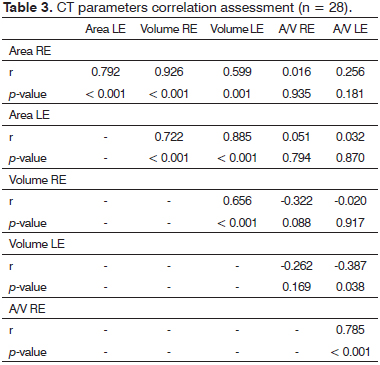
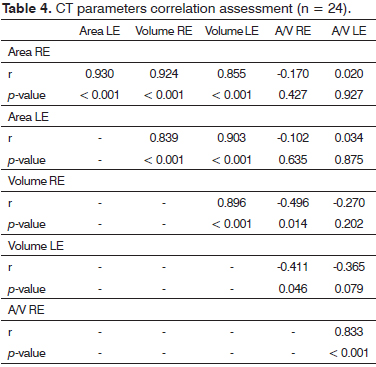
Strong correlations were found between the right and left mastoid volumes (r = 0.65), surface areas (r = 0.79), and surface area-to-volume ratios (r = 0.78) of the subjects included (n = 28) in this study (Table 3). The sample net of outliers (n = 24) revealed even stronger correlation coefficients: (r = 0.89), (r = 0.93), and (r = 0.83) respectively (Table 4). The low number of individuals included in this study (n = 28) makes it harder to tell whether the four patients with discrepant findings were true outliers or if they accounted for the normal variation within the studied population.
Swarts et al.10 reported correlation coefficients similar to the values found for the sample without outliers (n = 24) for right and left mastoid surface area and volume (r = 0.87 for surface area and volume). Considering the entire sample (n = 28), there was more asymmetry in the measurements of surface area and volume of right and left mastoids, particularly in volume (r = 0.65). Yet, symmetry prevailed. For bilateral structures, strong correlations between the measurements of each side (bilateral symmetry) indicate significant genetic contribution, whereas weak correlations between these measurements (bilateral asymmetry) are suggestive of predominantly environmental contribution to the assessed structure23. This fact reports back to two theories on mastoid development24,25. The theory of inheritance described by Diamant24 states that the degree of mastoid pneumatization is genetically determined, consequently yielding higher levels of symmetry. According to Wittmaack25, the degree of mastoid pneumatization is influenced by episodes of otitis media or tubal disorders during childhood, which could explain asymmetries. As the population included in this study was made up of adults with healthy ears without history of pediatric chronic otitis media, the reported degree of volume symmetry could be explained by the genetic theory described by Diamant24. However, reports of chronic otitis media occurred during childhood could be subject to memory bias and confound the analysis10. Other factors could affect genetically programmed expression and lead to various degrees of asymmetry13.
In the complete sample (n = 28) and in the sample without outliers (n = 24), the mean values found for surface area (297.7 cm2 and 304.6 cm2 respectively) and volume (33.2 cm3 and 33.1 cm3 respectively) for all ears were greater than the values reported in previous studies8,10. Conversely, the mean surface area-to-volume ratio was lower than previously reported for the complete sample (n = 28) and for the sample without outliers (n = 24) (9.4 cm-1 and 9.6 cm-1 respectively)8,10. Magnuson5 claimed gas exchange capacity was directly correlated with the surface area-to-volume ratio. However, recent studies have played down the importance of the surface area-to-volume ratio in gas exchange, as ratios appear to be somewhat constant13,16. Csakanyi et al.9 compared measurements of mastoid area and volume in children with and without otitis media with effusion (OME) and contradictorily reported greater surface area-to-volume ratios in children with OME. Therefore, more studies are required to clarify the actual meaning and significance of the surface area-to-volume ratio in mastoid physiology and pathogenesis.
Some specific factors may impact the extent of mastoid pneumatization. Reduced pneumatization of the temporal bone is evident in craniofacial disorders such as achondroplasia, Pierre Robin syndrome, and Crouzon syndrome. Cystic fibrosis results in increased temporal bone pneumatization26. In this study, none of the patients had specific syndromes or diseases to explain for the high mean surface areas and volumes reported.
CONCLUSION
The mastoid surface areas and volumes measured in adult Brazilians follow a linear correlation, as described in studies carried out in other countries. More studies with larger samples may provide clarification on whether the mean mastoid surface area and mean mastoid volume of the Brazilian population is higher than the mean values found for other populations.
REFERENCES
1. Ars B, Dirckx J, Ars-Piret N, Buytaert J. Insights in the physiology of the human mastoid: message to the surgeon. Int Adv Otol. 2012;8(2):296-310.
2. Doyle WJ. The mastoid as a functional rate-limiter of middle ear pressure change. Int J Pediatr Otorhinolaryngol. 2007;7(3):393-402. http://dx.doi.org/10.1016/j.ijporl.2006.11.004
3. Alper CM, Kitsko DJ, Swarts JD, Martin B, Yuksel S, Cullen Doyle BM, et al. Role of the mastoid in middle ear pressure regulation. Laryngoscope. 2011;121(2):404-8. http://dx.doi.org/10.1002/lary.21275
4. Gaihede M, Dirckx JJ, Jacobsen H, Aernouts J, Søvsø M, Tveterås K. Middle ear pressure regulation--complementary active actions of the mastoid and the Eustachian tube. Otol Neurotol. 2010;31(4):603-11.
5. Magnuson B. Functions of the mastoid cell system: auto-regulation of temperature and gas pressure. J Laryngol Otol. 2003;117(2):99-103. http://dx.doi.org/10.1258/002221503762624512
6. Alicandri-Ciufelli M, Gioacchini FM, Marchioni D, Genovese E, Monzani D, Presutti L. Mastoid: a vestigial function in humans? Med Hypotheses. 2012;78(3):364-6. http://dx.doi.org/10.1016/j.mehy.2011.12.006
7. Todd NW, Pitts RB, Braun IF, Heindel H. Mastoid size determined with lateral radiographs and computerized tomography. Acta Otolaryngol. 1987;103(5-6):226-31.
8. Park MS, Yoo SH, Lee DH. Measurement of surface area in human mastoid air cell system. J Laryngol Otol. 2000;114(2):93-6. http://dx.doi.org/10.1258/0022215001904969
9. Csakanyi Z, Katona G, Josvai E, Mohos F, Sziklai I. Volume and surface of the mastoid cell system in otitis media with effusion in children: a case-control study by three-dimensional reconstruction of computed tomographic images. Otol Neurotol. 2011;32(1):64-70. http://dx.doi.org/10.1097/MAO.0b013e3181fcec84
10. Swarts JD, Doyle BM, Doyle WJ. Relationship between surface area and volume of the mastoid air cell system in adult humans. J Laryngol Otol. 2011;125(6):580-4. http://dx.doi.org/10.1017/S0022215110002811
11. Sadé J, Fuchs C. Secretory otitis media in adults: I. The role of mastoid pneumatizationas a risk factor. Ann Otol Rhinol Laryngol. 1996;105(8):643-7.
12. Tos M, Stangerup SE. Mastoid pneumatization in secretory otitis. Further support for the environmental theory. Acta Otolaryngol. 1984;98(1-2):110-8. http://dx.doi.org/10.3109/00016488409107542
13. Swarts JD, Foley S, Alper CM, Doyle WJ. Mastoid geometry in a cross-section of humans from infancy through early adulthood with a confirmed history of otitis media. Int J Pediatr Otorhinolaryngol. 2012;76(1):137-41. http://dx.doi.org/10.1016/j.ijporl.2011.10.021
14. Cinamon U, Sadé J. Mastoid and tympanic membrane as pressure buffers: a quantitative study in a middle ear cleft model. Otol Neurotol. 2003;24(6):839-42. http://dx.doi.org/10.1097/00129492-200311000-00002
15. Doyle WJ. Experimental results do not support a gas reserve function for the mastoid. Int J Pediatr Otorhinolaryngol. 2000;52(3):229-38. http://dx.doi.org/10.1016/S0165-5876(00)00292-5
16. Swarts JD, Cullen Doyle BM, Alper CM, Doyle WJ. Surface area-volume relationships for the mastoid air cell system and tympanum in adult humans: Implications for mastoid function. Acta Otolaryngol. 2010;130(11):1230-6. http://dx.doi.org/10.3109/00016489.2010.480982
17. Koç A, Ekinci G, Bilgili AM, Akpinar IN, Yakut H, Han T. Evaluation of the mastoid air cell system by high resolution computed tomography: three-dimensional multiplanar volume rendering technique. J Laryngol Otol. 2003;117(8):595-8. http://dx.doi.org/10.1258/002221503768199906
18. Cinamon U. The growth rate and size of the mastoid air cell system and mastoid bone: a review and reference. Eur Arch Otorhinolaryngol. 2009;266(6):781-6. http://dx.doi.org/10.1007/s00405-009-0941-8
19. Lee DH, Jun BC, Kim DG, Jung MK, Yeo SW. Volume variation of mastoid pneumatization in different age groups: a study by three-dimensional reconstruction based on computed tomography images. Surg Radiol Anat. 2005;27(1):37-42. http://dx.doi.org/10.1007/s00276-004-0274-7
20. Colhoun EN, O'Neill G, Francis KR, Hayward C. A comparison between area and volume measurements of the mastoid air spaces in normal temporal bones. Clin Otolaryngol Allied Sci. 1988;13(1):59-63. http://dx.doi.org/10.1111/j.1365-2273.1988.tb00282.x
21. Mangabeira-Albernaz P. Contribuição ao estudo radiográfico da mastóide. Valor da posição occipital posterior (Worms-Bretton-Altschul). Rev Bras Otorrinolaringol. 1933;1(3):182-96.
22. Bento RF, Bogar P, Sennes LU, Ramos AHC, Marone SAM, Miniti A. Estudo da relação do tamanho da mastóide e resultados de miringoplastia. Rev Bras Otorrinolaringol. 1992;58(1):21-6.
23. Siegel MI, Doyle WJ. The differential effects of prenatal and postnatal audiogenic stress on fluctuating dental asymmetry. J Exp Zool. 1975;191(2):211-4. http://dx.doi.org/10.1002/jez.1401910208
24. Diamant M. Otitis and pneumatization of the mastoid bone. Acta Otolaryngol (Stockh). 1940;41(Suppl):1-149.
25. Wittmaack K. Über die normale und Pathologische Pneumatization des Schlafenbeins einschiesslich ihrer Beziehungen zu der Mittelohrerkrankungen. Jena: Fischer; 1918. p.1-64.
26. Hill CA. Ontogenetic change in temporal bone pneumatization in humans. Anat Rec (Hoboken). 2011;294(7):1103-15. http://dx.doi.org/10.1002/ar.21404
1. MD, ENT (MSc. Student, Graduate Program on Health Sciences of the University of Brasília, Brasília, Brazil).
2. PhD (MD, Radiologist, Advisor in the Graduate Program on Health Sciences of the University of Brasília, Brasília, Brazil).
3. PhD (MD, ENT, Head of the Hyperbaric Medicine Service, Armed Forces Hospital, Brasília, Brazil).
4. PhD (MD, ENT, Professor and Advisor in the Graduate Program on Health Sciences of the University of Brasília, Brasília, Brazil).
University of Brasília.
Send correspondence to:
Marco Antônio Rios Lima
S.M.T conjunto 16, casa 5
Taguatinga - DF. Brazil. CEP: 72023-480
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on January 7, 2013.
Accepted on April 17, 2013. cod. 10706.