Year: 2013 Vol. 79 Ed. 3 - (23º)
Relato de Caso
Pages: 403 to 403
Schwannoma of the nasal septum: evaluation of unilateral nasal mass
Author(s): Henrique Furlan Pauna1; Guilherme Machado de Carvalho2; Alexandre Caixeta Guimarães1; Rebecca Christina Kathleen Maunsell3; Eulália Sakano4
DOI: 10.5935/1808-8694.20130070
Keywords: nasal septum; neuroma acoustic; otorhinolaryngologic neoplasms.
![]()
INTRODUCTION
Schwannomas are benign tumors originated in the neural crests derived from Schwann cells. They are often encapsulated, well circumscribed, and connected to nerve tissue. In microscope examination they present a combination of two growth patterns, Antoni A and B, both with elongated cells and regular oval nuclei. Malignant schwannomas occur in only 2% of the cases, although local recurrence is common in cases of incomplete tumor resection1.
The vestibulocochlear nerve ranks first among involved sites, accounting for 80% of the cases. Only 4% of the tumors of the head and neck are found in the nose or sinuses2. Autonomic nerve fibers or the maxillary branch of the trigeminal nerve may originate in the nose2. Schwannomas are more commonly seen in the ethmoid sinus, followed by the maxillary sinus, nasal cavities, and sphenoidal sinus1. Unilateral or bilateral progressive nasal obstruction, accompanied or not by epistaxis, hyposmia, and headaches, are usually observed in schwannoma patients. Physical examination usually reveals a grayish vegetative polypoid highly vascularized bleeding tumor. Examination with a fiberscope and CT scans are required to assess the extent of tumor involvement and plan for surgery2.
CT scans of paranasal schwannomas usually show low-density areas in their center with contrast uptake in the borders3.
This paper described the evolution of a patient with a unilateral tumor diagnosed as a schwannoma of the nasal septum.
CASE REPORT
A 78-year-old male patient was referred to our service with progressive nasal obstruction evolving for two years.
Physical examination was normal and endoscopic examination of the nose revealed an exophytic grayish tumor with uneven borders, with a pedicle in the posterior septum region close to the upper corner of the right choana.
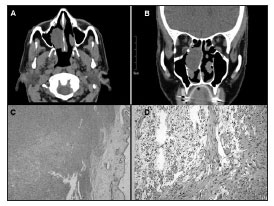
CT scans showed a nodular, low-density, well-delimited homogeneous tumor and some bone thinning in the medial wall of the right maxillary sinus (Figure 1).
Figure 1. A: CT scan (axial view) showing a tumor in the right nasal cavity inserted in the posterior nasal septum. B: CT scan (coronal view) showing the tumor inserted in the septum projecting into the lower turbinate. C: Histology slide showing a myxoid formation to the right of the respiratory epithelium in the central portion of the image (lower cell count) characteristically seen in Antoni B tissue; spindle-shaped cells seen in Antoni A tissue are shown on the upper left corner. (HE;26.5x). D: Antoni B tissue s shown on the left (scarce cytoplasm with intercellular hydrated material) and Antoni A on the right of the slide (elongated cells crossing each other in bundles, with nuclei resembling a palisade formation). (HE;64x).
The patient was submitted to endoscopic endonasal surgery. The tumor was removed with margins from the posterior septum periosteum. The procedure was uneventful.
Pathology tests showed proliferation of spindle-shaped cells arranged in a short fascicle pattern with oval wavy nuclei and acidophilic indistinct cytoplasm, characteristically seen in schwannomas (Figure 1).
DISCUSSION
The literature comprises approximately 70 case reports of nasal schwannoma. Most cases involve adults in their forties to sixties, with little difference between genders. Complaints usually revolve around nasal obstruction, anosmia, deformity of the nasal pyramid, and epistaxis2.
CT scans usually show lesions in the surrounding bone structures; erosion is more commonly seen in large schwannomas. MRI outperforms CT in differentiating tumors from inflammatory disorders and normal tissue, in addition to providing better information on tumor intracranial invasion3.
Differential diagnosis for unilateral tumors includes nasal polyps (22.2%), antrochoanal polyps (19%), chronic rhinosinusitis (12.7%), concha bullosa (11.1%), retention cysts (6.3%), mucocele (3.2%), and schwannomas in 1.6% of the cases4. Other diseases considered are carcinoma, sarcoma, lymphoma, juvenile angiofibroma, inverted papilloma, meningioma, neurofibroma, melanoma, and olfactory neuroblastoma (esthesioneuroblastoma). Immunohistochemistry aids in the diagnosis of controversial cases.
Unilateral tumors must be thoroughly investigated, ideally with biopsy, particularly to diagnose cases of malignancy4. Preoperative biopsy was not carried out in our patient because of his age and the benign aspect of his tumor.
Treatment is mostly curative and can be offered in the form of surgical removal by lateral rhinotomy or endoscopic endonasal surgery3. Radiation therapy is reserved for cases of nerve sheath malignant tumors. Patients with tumors confined to the paranasal sinuses have excellent prognosis5. Endoscopic surgery introduces less morbidity, patients are not left with visible surgical scars, and the hospital stay after surgery is shorter6.
CLOSING REMARKS
The diagnosis and management of patients with schwannoma can be challenging, as clinical and imaging findings of unilateral tumors may be deceiving. Schwannomas must be regarded as one of the possible diagnoses in such cases. Endoscopic endonasal surgery provides for a less invasive approach and offers an improved procedure to completely remove the tumor.
REFERENCES
1. Frosch MP, Anthony DC, De Girolami U. O Sistema Nervoso Central. Em: Kumar V, Abbas AK, Fausto N, Robbins SL, Cotran RS. Patologia: Bases Patológicas das Doenças. 7a ed. Rio de Janeiro: Elsevier; 2005. p.1479-80.
2. Luchi GER, Magalhães MR, Lanzelotti SM, Jorge Júnior JJ, Mendonça EASF, Magalhães SLB. Nasal schwannoma. Braz J Otorhinolaryngol. 2006;72(5):714.
3. Fujiyoshi F, Kajiya Y, Nakajo M. CT and MR imaging of nasoethmoid schwannoma with intracranial extension. AJR Am J Roentgenol. 1997;169(6):1754-5. http://dx.doi.org/10.2214/ajr.169.6.9393211 PMid:9393211
4. Habesoglu TE, Habesoglu M, Surmeli M, Uresin T, Egeli E. Unilateral sinonasal symptoms. J Craniofac Surg. 2010;21(6):2019-22. http://dx.doi.org/10.1097/SCS.0b013e3181f5389a PMid:21119491
5. Gillman G, Bryson PC. Ethmoid schwannoma. Otolaryngol Head Neck Surg. 2005;132(2):334-5. http://dx.doi.org/10.1016/j.otohns.2004.04.027 PMid:15692551
6. Küpper DS, Demarco RC, Resende R, Anselmo-Lima WT, Valera FCP Moribe I. Endoscopic nasal dacryocystorhinostomy: results and advantages over the external approach. Braz J Otorhinolaryngol. 2005;71(3):356-60. PMid:16446941
1. MD (ENT Resident Physician at UNICAMP).
2. MSc in Medicine (MD, ENT (otology fellow at UNICAMP)).
3. MSc in Medical Sciences (MD, ENT at the Otorhinolaryngology Service in the Sumaré State Hospital, ENT-HNS Course, UNICAMP).
4. PhD in Medical Sciences (MD, ENT, Head of the Rhinology Service, ENT-HNS Course, UNICAMP).
Otorhinolaryngology and Head and Neck Program - University Hospital - Medical School of the State University of Campinas (UNICAMP), SP, Brazil.
Send correspondence to:
Henrique Furlan Pauna
Rua Aldo de Oliveira Barbosa, n 170. Parque das Universidades
Campinas - SP. Brazil. CEP: 13086-030
E-mail: h_pauna@hotmail.com
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on April 21, 2012.
Accepted on October 20, 2012. cod. 9165.
All rights reserved - 1933 /
2025
© - Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico Facial