Year: 2013 Vol. 79 Ed. 3 - (16º)
Artigo Original
Pages: 359 to 365
Amplification by bone conduction in congenital malformations: patient benefits and satisfaction
Author(s): Elaine Cristina Moreto Paccola1; João Cândido Fernandes2; Maria Fernanda Capoani Garcia Mondelli3
DOI: 10.5935/1808-8694.20130063
Keywords: bone conduction; congenital abnormalities; hearing aids; patient satisfaction; questionnaires.
Abstract:
Hearing loss is one of the most common clinical findings in subjects with malformations of the ear. Treatment consists of surgery and/or adapt a hearing aid amplification by bone (HA VO). Early intervention is critical to auditory stimulation and development of speech and language.
OBJECTIVE: To characterize the audiological profile of subjects with congenital malformation of the external ear and/or middle and evaluate the benefit and satisfaction of using HA VO.
METHOD: A descriptive study, subjects with bilateral congenital malformations of the external ear and/or middle, conductive or mixed hearing loss, moderate or severe and HA VO users. Evaluation of the benefit test using sentence recognition in noise and measures of functional gain and satisfaction assessment questionnaire using international IQ - HA.
RESULTS: 13 subjects were evaluated, 61% were male and 80% with moderate conductive hearing loss or severe. There was better performance in the evaluation proposal, provided with HA when compared to the condition without HA.
CONCLUSION: HA VO showed advantages for the population studied and should be considered as an option for intervention. Satisfaction was confirmed by elevated scores obtained in IQ - HA.
![]()
INTRODUCTION
Ear malformations occur during embryo development and may affect the outer, middle and inner ear. The more common congenital ear anomalies affect the pinna and the ear canal, involving one or both ears. Hearing loss is one of the most common findings in individuals with ear malformations and may occur in varying degrees and types, depending on the level of involvement1.
Treatment consists of surgery and/or fitting patients with hearing aids. Early fitting of hearing aids favors auditory stimulation and the development of speech and language acquisition. Surgery is not indicated in all cases, and is usually performed in subjects aged at least six or seven years2.
Conventional hearing aids cannot be offered to patients with ear agenesis or ear canal stenosis, given the impossibility of using air conduction to stimulate hearing3. In these cases, bone conduction hearing aids represent the best option.
Bone conduction hearing aids are designed to bypass the defective middle ear to stimulate the structures inside the cochlea. The output transducer is a bone oscillator. The vibrations of the bone oscillator must be effectively transmitted to the skull. In order to achieve proper transmission, the bone oscillator is usually mounted on one side of the head, attached to an elastic band to keep it pressed against the skull. The hearing aid may be located in the other end of the headband, or close to the user's body as in conventional hearing aids4.
Research indicates that the amplification provided by bone conduction hearing aids, the headaches produced by the pressure applied by the headband against the mastoid, and the adverse psychosocial impact felt by users are some of the issues associated with wearing these devices. Complaints of headache caused by the headband and dissatisfaction with the visibility of the hearing aids are common in pre-teens and teenagers. These factors combined lead to reduced usage of hearing aids5.
Bone-anchored hearing aids (BAHA) are an advantageous alternative to conventional bone conduction hearing aids. BAHA have been studied for over two decades and their use is well established in Europe and the USA. More than 20,000 patients have been implanted with BAHA in the world6.
The decision on the choice of hearing aids to be offered must be made together with the patient and his/her family. Bone conduction hearing aids are a practical, non-invasive option available at some public health care services.
This study aims to characterize the audiological profile of individuals with congenital malformations of the ear and/or middle ear and assess the benefits and level of satisfaction achieved with bone conduction hearing aids.
METHOD
This study was approved by the Ethics Committee for Research with Human Beings and granted permit #018/2006. Subjects were advised of the nature of the study and asked to sign an informed consent term.
The following enrollment criteria were adopted:The hearing aids worn by the individuals enrolled in this study were the Unitron UE12 PPL and the SiemensTM Phoenix 213, coupled to a metal rod, a wire, and a bone oscillator of the same brand as the device.Age between six and 40 years; Bilateral congenital malformation involving the ear and/or middle ear; Bilateral moderate to severe conductive or mixed hearing loss7; Experience wearing retroauricular bone conduction hearing aids for at least three months; No cognitive disorders.
Speech recognition tests, functional gain measurements, and the IOI - HA questionnaire were used to assess the subjects.
Speech recognition in noise
A two-channel audiometer was used in these tests, as dictated by the standards published by the American National Standards Institute (ANSI 1991, 1996). A CD player, a stereo amplifier, and two loudspeakers (one playing speech and the other noise) were connected to the audiometer.
The material8 used in the tests was made up of seven lists of sentences of everyday conversation and babble noise from the commercially available CD List of Sentences in Portuguese.
The lists comprised ten short, easily repeatable affirmative sentences ranging between four and seven words in length. The sentences in the list were similar in terms of phonetic content and structure. The lists contained 48 to 54 words and 202 to 214 characters each. The sentences were recorded by a male professional announcer.
The first sentence in each list was presented at an intensity of 65 dBA to assess speech recognition thresholds in noise (SRTN). The individuals in the sample had the hearing thresholds required to perceive speech at such intensity. Noise was played at 65 dBA, in a way to start the test with a signal to noise ratio of 0 dB, as suggested by the author. When the subjects were able to correctly recognize the spoken sentence and repeat it using the same phonologic pattern, the next sentence would be played at an intensity of 4 dB less than the previous sentence. In the event of a mistake, the signal was increased in steps of 2 dB, until the individual got it right. Steps of two decibels would then be applied upwards in the event of other mistakes and downwards when the individual was successful, until all ten sentences were played.
The subjects were positioned one meter away from the loudspeakers at an angle of incidence from the noise and speech source of zero degrees azimuth.
Measurements of functional gain
The functional gain provided by hearing aids is defined by the difference in decibels between the free-field audiometry thresholds assessed with the subjects with and without hearing aids under equal testing conditions.
The minimum intensity was 30 dB NPS with and without the use of hearing aids, as this is the minimum level of intensity allowed by the equipment used in the test sessions.
Hearing thresholds at 6000 and 8000 Hz were not acquired, as the hearing aids worn by the subjects in this study provided less gain in these frequencies.
The limit psychometric method was used to acquire hearing thresholds. The intensity of the sound stimuli was gradually reduced in steps of 10 dB until the patients could no longer respond. Then, the intensity was increased in steps of 5 dB until the subjects were able to respond again. The threshold was defined as the intensity at which patients were able to respond to 50% of the sentences presented.
Satisfaction evaluation
The Brazilian Portuguese version of the International Outcome Inventory for Hearing Aids (IOI - HA)9 was used to assess patient satisfaction.
The questionnaire contains seven questions with five possible answers each and is used to assess subject adaptation to hearing aids considering the following issues: 1 - Hearing aid daily use; 2 - Benefit; 3 - Residual activity limitations; 4 - Satisfaction; 5 - Residual participation restrictions; 6 - Impact on others; 7 - Quality of life.
The questionnaire offers five possible answers graded from left to right, in a way that the first option refers to poor performance corresponding to a score of one, and the last option reflects top performance and a score of five. Caretakers/guardians were advised along with the patients to choose only one answer to characterize how well adapted the subjects were to their hearing aids.
The analysis of the IOI - HA questionnaire was based on the answers provided to each question individually and as a group. The scores on each question, the total score considering the seven questions, and the scores considering factors 1 and 2 in the questionnaire9 were taken into account. Factor 1 comprised questions 1, 2, 4, and 7 and intended to describe the interaction between the user and the hearing aids. Factor 2 considered questions 3, 5, and 6 and depicted the relationship between the user and the environment.
Each of the seven questions have a minimum possible score of one and a maximum possible score of five. The total score refers to the sum of the scores given to each answer and may range from seven to 35. Scores on factor 1 may range from four to 20 points, while factor 2 can vary between three and 15 points. Higher scores indicate better outcome in regards to adaptation to hearing aids.
Student's t-test for paired samples was used to compare measurements with and without hearing aids. Student's t-test was used to estimate the mean scores on the questionnaire.
RESULTS
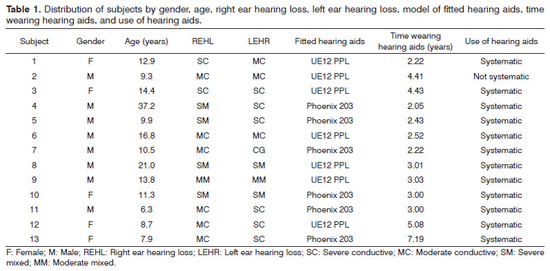
Thirteen individuals (eight males and five females) wearing hearing aids for a mean of three years were included in the study. Their ages ranged between six and 37 years (mean of 14 years of age) (Table 1).
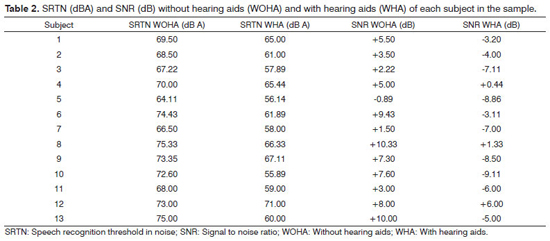
Descriptive and inferential statistical analysis (95% confidence interval) of the results derived from the assessment of the 13 subjects with and without hearing aids, in tests to assess speech recognition thresholds in noise (SRTN) at 65 dB A and signal to noise ratios (SNR) are presented on Table 2.
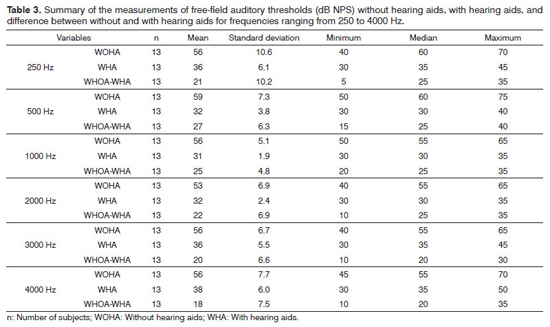
Comparisons between the test outcomes of the 13 individuals with and without hearing aids, in terms of free-field audiometry hearing thresholds (dB NPS) at 250 to 4000 Hz, along with the measurements of functional gain in each of the tested frequencies are presented on Table 3.
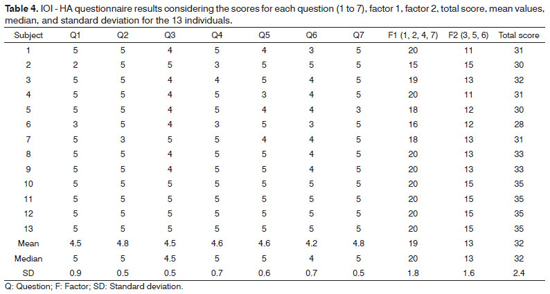
Table 4 shows the results from the IOI - HA questionnaire, the scores for each question (1 to 7), factor 1, factor 2, total scores, mean values, medians, and standard deviations observed for the 13 included individuals.
DISCUSSION
Eight of the 13 included subjects were males (Table 1). The literature reports similar gender incidence rates10-12. The estimated male to female ratio of occurrence of malformations is 2.5:1 13.
All patients included in this study had bilateral malformation, contrary to what other authors have observed. According to them, unilateral malformations were more prevalent10,11,13,14. Our data was in agreement with a study12 that found similar prevalences for bilateral and unilateral malformations.
Table 1 shows that moderate conductive hearing loss was the most common type of hearing loss found in our patients, followed by severe conductive hearing loss, and severe mixed hearing loss. Authors15 have reported that congenital aural atresia causes, at best, moderate conductive hearing loss.
Congenital stenosis or atresia of the ear canal may be partial or complete, and is frequently accompanied by malformations of the pinna, ossicles, middle ear cavity, and otic capsule, resulting in a vast array of types of hearing loss, ranging from moderate conductive to severe mixed hearing loss16.
The subjects included in this study claimed to be systematic users of hearing aids (Table 1). Authors14 have indicated that in cases of pediatric bilateral congenital aural atresia with preserved cochlear function the patients should be offered bone conduction hearing aids until a decision is made about surgery, before they are sent to school. The authors have noted that hearing aids should be offered as soon as possible to promote early auditory stimulation and the development of speech and language acquisition.
A study carried out with 20 children with ear malformations found that 36% of the subjects with unilateral malformations rarely used bone conduction hearing aids, and that 44% of the children with bilateral malformation always had them on. It is possible that the latter group wore hearing aids more frequently as a result of their bilateral involvement1.
Table 2 shows better SRTN at 65 dBA when patients wore bone conduction hearing aids than when they did not wear them.
Signal to noise ratios may be presented in the form of positive or negative numbers, and are expressed in decibels (dB)17. When the intensity of speech is higher than the intensity of noise, the SNR is positive, making it easier for the listener to understand what is being said. However, when the intensity of speech is lower than the intensity of noise, speech recognition is impaired. Subjects able to perform well in the presence of negative signal to noise ratios are deemed to have better hearing function.
Many studies have looked into speech recognition in noise tests to compare individuals wearing conventional bone conduction hearing aids and bone-anchored hearing aids. Some authors have reported better results for BAHA users18-25, while others failed to observe such difference26,27.
A study conducted with 122 subjects on speech recognition in noise at an SNR of + 6 dB found a mean improvement in speech recognition of 35.5% when subjects wore bone conduction hearing aids and a mean improvement of 41.8% when they wore BAHA, when compared to subjects without hearing aids. The 6.3% difference between BAHA and conventional bone conduction hearing aids was statistically significant25.
In Brazil, studies on the fitting of hearing aids in individuals with ear malformations are scarce. A study was carried out on two individuals with craniofacial malformations and bilateral moderate conductive hearing loss wearing conventional bone conduction hearing aids and BAHA. The author looked into free field tone thresholds and speech recognition in noise using the staggered spondaic word test, with the subjects not wearing hearing aids, with conventional bone conduction hearing aids on, and with BAHA on, to conclude that both devices yielded satisfactory levels of hearing gain. In regards to speech recognition, the BAHA outperformed the other devices, but failed to show evidences of improvement when compared to monaural and binaural fittings of the two types of hearing aids analyzed28.
According to a study carried out at a high complexity care center1, bone conduction hearing aids have improved the speech recognition skills of children with bilateral ear malformations.
Table 3 shows a homogeneous distribution of the data, revealing that all patients in the study improved their hearing thresholds at all analyzed frequencies when they were wearing hearing aids.
The IOI - HA is a sensitive tool that can be used to detect individuals with negative experiences while wearing hearing aids9.
Table 4 shows positive mean scores, considering that the maximum possible score is five for each question. Consequently, the analyses of factor 1, factor 2, and total score were also positive, and indicated a good level of subjective satisfaction with the hearing aids.
These results have shown that the individuals included in this study were happy with their hearing aids, contrary to what was observed in other papers21,23,25,26,29, in which bone conduction hearing aids were linked with discomfort caused by the pressure the headband applied on the mastoid, skin irritation, acoustic feedback, poor acoustic properties because of the attenuation introduced by the skin and soft tissues in the interaction between the transmitter and the bone, and poor compliance for cosmetic reasons.
CONCLUSION
Patients showed improved functional gain and reported they were happy with their bone conduction hearing aids, thus showing the benefits provided to the studied population by this type of hearing aids.
REFERENCES
1. Dell'Aringa AHB, Castiquini EAT. Adaptação do Aparelho de Amplificação Sonora Individual por Via Óssea em Crianças Portadoras de Malformação de Orelha Externa e Média. Arq Int Otorrinolaringol. 2005;9(2):310-6.
2. Fetterman BL, Luxford WM. The rehabilitation of conductive hearing impairment. Otolaryngol Clin North Am. 1997;30(5):783-801. PMid:9295254
3. Wazen JJ, Caruso M, Tjellstrom A. Long-term results with the titanium bone-anchored hearing aid: the U.S. experience. Am J Otol. 1998;19(6):737-41. PMid:9831146
4. Dillon H. Hearing aids. Sydney: Boomerang Press; 2001.
5. Habal M, Frans N, Zelski R, Scheuerle J. Percutaneous bone-anchored hearing aid. J Craniofac Surg. 2003;14(5):637-42. http://dx.doi.org/10.1097/00001665-200309000-00007 PMid:14501321
6. Priwin C, Stenfelt S, Granström G, Tjellström A, Håkansson B. Bilateral bone-anchored hearing aids (BAHAs): an audiometric evaluation. Laryngoscope. 2004;114(1):77-84. http://dx.doi.org/10.1097/00005537-200401000-00013 PMid:14709999
7. WHO. World Health Organization. Grades of Hearing impairment, 2007 [acesso em 26 de fevereiro de 2010]. Disponível em: http://www.who.int/pbd/desfness/hearing_impairment_grades/en/index.html.
8. Santos SN, Daniel RC, Costa MJ. Estudo da equivalência entre as listas de sentenças em português. Rev CEFAC. 2009;11(4):673-80. http://dx.doi.org/10.1590/S1516-18462009000800016
9. Cox RM, Alexander GC. The International Outcome Inventory for Hearing Aids (IOI-HA): psychometric properties of the English version. Int J Audiol. 2002;41(1):30-5. http://dx.doi.org/10.3109/14992020209101309
10. De la Cruz A, Linthicum FH Jr, Luxford WM. Congenital atresia of the external auditory canal. Laryngoscope. 1985;95(4):421-7. http://dx.doi.org/10.1288/00005537-198504000-00010 PMid:3884941
11. Hayes D, Northern JL. Infants and hearing. San Diego: Singular Publishing Group; 1996.
12. Castiquini EAT, Silveira TS, Shayeb DR, Meyer ASA. Avaliação audiológica de indivíduos portadores de malformação de orelha. Arq Int Otorrinolaringol. 2006;10:98-103.
13. Park SS, Chi DH. External ear, aural atresia. e-Medicine [online] 2007 Jan 25 [consultado em 26 jun 2007]; [19 telas]. Disponível em: http://www.emedicine.com/ent/topic329.htm
14. Ng M, Horlbeck DM. Aural atresia. e-Medicine [online] 2007. Jan 29 [consultado em 26 jun 2007]; [14 telas]. Disponível em: http://www.emedicine.com/ent/topic141.htm
15. Kaga K, Setou M, Nakamura M. Bone-conducted sound lateralization of interaural time difference and interaural intensity difference in children and a young adult with bilateral microtia and atresia of the ears. Acta Otolaryngol. 2001;121(2):274-7. http://dx.doi.org/10.1080/000164801300043820 PMid:11349795
16. Goebel J, Valente M, Valente M. Fitting strategies for patients with conductive or mixed hearing loss. In: Valente M, editor. Strategies for selecting and verifying hearing aid fittings. 2nd ed. New York: Thieme; 2002.
17. Agnew J. Challenges and some solutions for understanding speech in noise. In S Kochkin & KE Strom's (eds.) High Performance Hearing Solutions, Vol. 3, Hearing in Noise. 1999;Hear Rev;6(Suppl 1):4-9.
18. Carlsson P, Håkansson B, Rosenhall U, Tjellström A. A speech-to-noise ratio test with the bone-anchored hearing aid: a comparative study. Otolaryngol Head Neck Surg. 1986;94(4):421-6. PMid:3086800
19. Håkansson B, Lidén G, Tjellström A, Ringdahl A, Jacobsson M, Carlsson P, et al. Ten years of experience with the Swedish bone-anchored hearing system. Ann Otol Rhinol Laryngol Suppl. 1990;151:1-16. PMid:2121086
20. Hamann C, Manach Y, Roulleau P. Bone anchored hearing aid. Results of bilateral applications. Rev Laryngol Otol Rhinol (Bord). 1991;112(4):297-300.
21. Mylanus EA, Snik AF, Jorritsma FF, Cremers CW. Audiologic results for the bone-anchored hearing aid HC220. Ear Hear. 1994;15(1):87-92. http://dx.doi.org/10.1097/00003446-199402000-00010 PMid:8194683
22. Snik AF, Mylanus EA, Cremers CW. Speech recognition with the bone-anchored hearing aid determined objectively and subjectively. Ear Nose Throat J. 1994;73(2):115-7. PMid:8168444
23. Snik AF, Mylanus EA, Cremers CW. The bone-anchored hearing aid compared with conventional hearing aids. Audiologic results and the patients' opinions. Otolaryngol Clin North Am. 1995;28(1):73-83. PMid:7739870
24. Snik AF, Dreschler WA, Tange RA, Cremers CW. Short- and long-term results with implantable transcutaneous and percutaneous bone-conduction devices. Arch Otolaryngol Head Neck Surg. 1998;124(3):265-8. PMid:9525509
25. Tjellström A, Håkansson B. The bone-anchored hearing aid. Design principles, indications, and long-term clinical results. Otolaryngol Clin North Am. 1995;28(1):53-72. PMid:7739869
26. Håkansson B, Tjellström A, Rosenhall U, Carlsson P. The bone-anchored hearing aid. Principal design and a psychoacoustical evaluation. Acta Otolaryngol. 1985;100(3-4):229-39. http://dx.doi.org/10.3109/00016488509104785 PMid:4061073
27. Bonding P, Jønsson MH, Salomon G, Ahlgren P. The bone-anchored hearing aid. Osseointegration and audiological effect. Acta Otolaryngol Suppl. 1992;492:42-5. http://dx.doi.org/10.3109/00016489209136807 PMid:1632249
28. Agra SER. Estudo clínico: utilização do aparelho auditivo ancorado ao osso (BAHA) em deficiente auditivo [Dissertação de Mestrado]. São Paulo: Pontifícia Universidade Católica de São Paulo; 1996. 141p. PMid:9004443
29. Habal M, Frans N, Zelski R, Scheuerle J. Percutaneous bone-anchored hearing aid. J Craniofac Surg. 2003;14(5):637-42. http://dx.doi.org/10.1097/00001665-200309000-00007 PMid:14501321
1. MSc in Rehabilitation Sciences at the Craniofacial Rehabilitation Hospital - University of São Paulo (Speech and Hearing Therapist at the Craniofacial Rehabilitation Hospital - University of São Paulo).
2. Professor in the Department of Mechanical Engineering of the Julio de Mesquita Filho Paulista State University.
3. PhD in Rehabilitation Sciences at the Craniofacial Rehabilitation Hospital - University of São Paulo (Professor in the Bauru Dentistry School - USP).
Craniofacial Rehabilitation Hospital - University of São Paulo.
Send correspondence to:
Maria Fernanda Capoani Garcia Mondelli
Al. Octávio Pinheiro Brizola, nº 9-75. Vila Universitária
Bauru - SP. Brasil. CEP: 17012-901
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on October 2, 2012.
Accepted on February 23, 2012. cod. 10498.