Year: 2013 Vol. 79 Ed. 1 - (23º)
Relato de Caso
Pages: 122 to 122
Tympanic membrane perforation caused by traumatic asphyxia
Author(s):
Fernando Luiz Westphal1; Renato Telles de Sousa2; Luiz Carlos Nadaf de Lima3; Luís Carlos de Lima4; Márcia dos Santos da Silva5
DOI: 10.5935/1808-8694.20130023
Keywords: hearing loss; thoracic injuries; tinnitus; tympanic membrane perforation.
![]()
INTRODUCTION
Tympanic membrane (TM) trauma may be caused by excessive pressure in the middle ear, thermal or chemical burns, direct penetrating trauma, or barotrauma. Increased pressure outside the ear is, by far, the most frequent mechanism by which TM trauma occurs1. This paper describes an unusual case of TM perforation caused by increased venous pressure in the head and neck area after acute chest trauma.
CASE PRESENTATIONA 31-year-old male subject had his chest compressed by a mechanical arm while he was working at an industrial plant. The subject lost his consciousness temporarily at the time of the accident and was sent to an Intensive Care Unit complaining of dyspnea, intense chest pain, and bilateral otalgia and tinnitus.
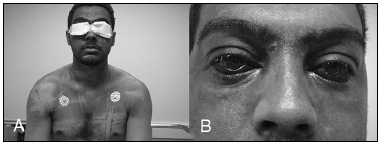
Physical examination: cyanosis of the face, upper third of the chest, and anterior and posterior portion of the chest (Figure 1A); bilateral otorrhagia and epistaxis, and subconjunctival hemorrhage (Figure 1B). Consciousness, respiratory and heart rates were normal. Cardiopulmonary auscultation, abdomen and lower limb examination did not reveal alterations. Otoscopic examination: bilateral TM perforation; perforation located centrally and affecting approximately 25% of the TM area on both sides.
Figure 1. A: Cyanosis of the upper third of the chest extending to the neck and head. B: Bilateral subconjunctival hemorrhage.
Complementary tests: echocardiogram was normal; chest CT scans showed minor left pleural effusion and two fractured costal arches. Lab tests revealed CPK-MB of 2540 IU and normal troponin levels. Audiometry tests were not available at admission.
The patient remained in the ICU for five days and for an additional six in the infirmary. He progressed well and his symptoms gradually subsided. Audiometry tests were carried out eight days after admission and the patient was found to have mild left conductive hearing loss and auditory thresholds within normal range in his right ear. Otoscopic examination was performed 20 days after the accident and showed signs of formation of a new tympanic membrane on the sites where the TM had been bilaterally perforated. Another audiometric examination was carried out 30 days after the trauma and showed normal thresholds on both ears.
DISCUSSION
Traumatic asphyxia (TA), also known as ecchymotic mask or Perthes syndrome, is a rare condition characterized by head and neck cyanosis, subconjunctival hemorrhage, and head and neck petechiae2. In order for the syndrome to occur, subjects have to undergo chest or chest and abdomen compression after inhaling with the glottis closed3. The sharp increase in intrathoracic pressure forces the blood on the right side of the heart and large chest veins to be ejected abruptly towards the head, producing blood stasis and rupturing capillaries. Thus, in addition to classic symptoms, there may also be varying degrees of mouth, ear, and nose bleeds, accompanied by tinnitus and transient hearing loss4. In the presented case, venous hypertension reached levels high enough to induce the rupturing of the TM. The patient complained of otalgia and tinnitus - symptoms compatible with his clinical status - but had no hypacusis.
It has been established that most traumatic TM perforations heal spontaneously. In large centers, patients in such condition are placed under observation. Factors such as secondary infection, pre-existing tympanosclerosis, and size and site of perforation are the main prognostic factor for healing5. Surgery is indicated only if the TM does not heal within three to six months. Studies suggest that 70% of central perforations, as observed in this patient, heal spontaneously6. The patient evolved satisfactorily. His TM was completely healed after 30 days and he had no signs of remaining hearing loss.
CLOSING REMARKS
Many are the etiologies of traumatic TM perforation, and unusual cases may occur as reported in this case. Victims of compression trauma who develop Perthes syndrome require ENT care to avoid the late complications associated with TM perforation.
REFERENCES
1. Afolabi OA, Aremu SK, Alabi BS, Segun-Busari S. Traumatic tympanic membrane perforation: an aetiological profile. BMC Res Notes. 2009;2:232.
2. Gösling T, Schmidt U, Herzog T, Tscherne H. Perthes syndrome. The classical symptom triad as a rarity in trauma surgery practice. Unfallchirurg. 2001;104(2):191-4.
3. Lee MC, Wong SS, Chu JJ, Chang JP, Lin PJ, Shieh MJ, et al. Traumatic asphyxia. Ann Thorac Surg. 1991;51(1):86-8.
4. Esme H, Solak O, Yurumez Y, Ermis S, Yaman M, Fidan F. Perthes syndrome associated with bilateral optic disc edema. Can J Ophthalmol. 2006;41(6):780-2.
5. Lou ZC, Tang YM, Yang J. A prospective study evaluating spontaneous healing of aetiology, size and type-different groups of traumatic tympanic membrane perforation. Clin Otolaryngol. 2011;36(5):450-60.
6. Bogar P, Sennes LU, Busch GHC, Marone SAM, Miriti A, Bento RF. Perfurações traumáticas de membrana timpânica. Rev Bras Otorrinolaringol. 1993;59(4):276-8.
1. Post-doctoral degree in Thoracic Surgery (Coordinator of Education and Research at the Getúlio Vargas University Hospital).
2. MSc in ENT (Head of the ENT Service at the Getúlio Vargas University Hospital).
3. MSc in ENT (Assistant Physician at the Getúlio Vargas University Hospital).
4. PhD in Heart Surgery (Head of the Thoracic Surgery Service at the Getúlio Vargas University Hospital).
5. ENT Resident Physician (Fist-year ENT Resident Physician).
Getúlio Vargas University Hospital.
Send correspondence to:
Fernando Luiz Westphal
Hospital Universitário Getúlio Vargas, Coordenação de Ensino e Pesquisa
Av. Aripuanã, nº 04, Praça 14 de Janeiro
Manaus - AM. Brazil. CEP: 69020-170
E-mail: f.l.westphal@uol.com.br
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on February 22, 2012.
Accepted on June 7, 2012. cod. 9056.
All rights reserved - 1933 /
2025
© - Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico Facial