Year: 2012 Vol. 78 Ed. 6 - (13º)
Artigo Original
Pages: 77 to 80
Thyroid papillary carcinoma associated to Hashimoto's thyroiditis
Author(s): Luiz Alexandre Albuquerque Freixo Campos1; Sílvia Miguéis Picado2; André Vicente Guimarães3; Daniel Araki Ribeiro4; Rogério Aparecido Dedivitis5
DOI: 10.5935/1808-8694.20120037
Keywords: carcinoma, papillary, thyroid neoplasms, thyroiditis, autoimmune.
Abstract:
There is controversy in the literature regarding the association between papillary thyroid carcinoma (PTC) and Hashimoto's thyroiditis (HT) and as to what would be the etiological relationship between them.
OBJECTIVE: To establish the proportion of cases among patients with TH and CPT, correlating it with histomorphological aspects.
METHOD: A retrospective study of patients undergoing partial or total thyroidectomy for PTC between 2007 and 2009, a total of 41 cases.
RESULTS: Regarding the association of HT and CPT, we found 11 cases (26.8%), all females, but without statistical significance. The mean age was 44.9 years among the patients with coexistent TH and CPT, whereas it was 49.1 years without that association. The average size of tumors in those without TH was 20.53 mm and for those with TH it was 12.72 mm (p = 0.4). Regarding pathology staging, the ratiosbetween those with and those without TH were kept in T1a, T1b and T3. In T2, there were no cases of coexistence of HT and PTC.
CONCLUSION: There is a rate of 26.8% of patients with association between TH and CPT, but without differences in relation to tumor size.
![]()
INTRODUCTION
Papillary thyroid carcinoma (PTC) is the most prevalent and the one with the best prognosis among all malignant thyroid neoplasias1,2. Hashimoto's thyroiditis (HT) is a chronic lymphocytic thyroiditis, and the most common cause of hypothyroidism in areas with proper amounts of iodine3. In 1955, Dailey et al.4 proposed, for the first time, the association between PTC and HT, also suggested by numerous other authors5-11.
However, there are authors who disagree from such association12-14 in studies which were not clear as to the association, after following up patients with HT. One of the bases for discussion is the etiology, and it is not clear whether thyroiditis predisposes to cancer or if it is later induced by the neoplasia5.
There are studies which show the expression of RET/PTC-1 and RET/PTC-3 oncogenes in patients with HT, confirmed by phenotyping15,16, which could prove HT as a pre-neoplastic lesion. There was also a study which showed the concurrent p63 expression, a p53-homologous protein which regulate squamous cells in HT-suggestive cells without concurrent neoplasia and in typical PTC cells; present in high rates (around 80%) in these two groups and without significant expression in other thyroid involvements17.
Our paper aims at studying the possible significant association between these two entities and whether or not there are differences in the PTC presentation in patients with HT and those without. The goal is to find the incidence of HT cases in patients with PTC, correlating histomorphometric aspects.
METHOD
The present study was approved by the Ethics in Research Committee of the institution where it was carried out, under protocol # 013/2011.
We carried out a retrospective study based on data collected from the files of the hospital where the study was carried out, as well as from the charts of patients submitted to total or partial thyroidectomies, because of PTC in histopathology specimens, between the years of 2007 and 2009, making up a total of 41 cases. We consecutively selected all the PTC cases, regardless of age or gender, with or without HT. We also investigated the incidence of Hashimoto's thyroiditis in the remaining cases submitted to partial or total thyroidectomies for other reasons. We took off the study those patients with incomplete data in their charts.
The study was based on data collected from the patients' charts, such as age, gender, tumor size and pathology staging after surgery.
The statistical analysis was carried out after preparing the data base. We then analyzed all the variables, investigating the statistical significance among the data, using the Fisher's exact test.
RESULTS
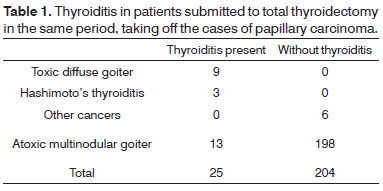
In the time frame between 2007 and 2009, there were 315 thyroidectomies, 41 due to thyroid papillary carcinoma and 274 for other reasons. Of these 274 procedures, 45 were partial thyroidectomies because of nodular goiter and, in none of them the pathologist found chronic thyroiditis. Among the cases submitted to total thyroidectomy (n = 229), chronic thyroiditis was seen in 12.25%; if we consider only those patients operated because of atoxic multinodular goiter in this group, the incidence of thyroiditis drops down to 6.65% (Table 1).
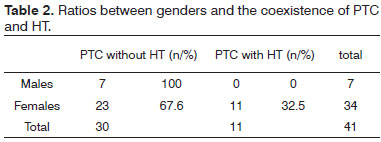
Thus, there were 41 total or partial thyroidectomies due to papillary carcinoma of the thyroid. Of these, 11 had concurrent HT (26.8%), while 30 did not have it (72.1%) - Table 2.
Thus, we found 11 cases of HT in 41 patients with papillary carcinoma (26.8%) and 13 cases of HT in 198 patients with multinodular goiter (6.65%), with statistical significance considering the Fisher's Exact Test (p = 0.005823).
Considering the demographic data from the 41 patients, 34 (82.93%) were females, while seven (17.07%) were males.
Concerning the HT-PTC association, there were 11 cases, all females, but without statistical significance. The mean age of the PTC cases was 48 years. In those cases of PTC concurrent with HT, the mean age was 44.9 years and without the association this value was 49.1 years. The minimum age among the patients was 20 years and the maximum was 91.
The mean tumor size among those without thyroiditis was 20.53 mm and for those with thyroiditis it was 12.72 mm, nevertheless, without statistical significance - p = 0.4.
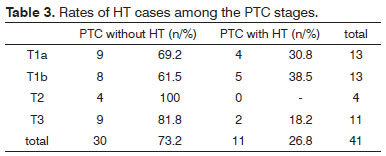
As to the pathology staging, the ratios between those with HT and those who did not have it were maintained in T1a, T1b and T3. In T2, there were no cases of coexistence between HT and PTC (Table 3).
DISCUSSION
HT was first described in 1912 18 as an autoimmune disease, affecting 5% of the general population and involving the diffuse infiltration of the thyroid by lymphocytes, fibrosis and gland parenchyma atrophy.
Since 1955 4, there are questions concerning the association between HT and PTC, with studies corroborating and studies disproving such association. This association has been reported by many authors, although showing different indices, probably due not only to different genetic factors and different environments, but also the numerous pathology definitions used in the many studies7.
A metanalysis showed that the HT incidence is 2.77 higher in patients with PTC when compared to patients with benign thyroid diseases. In addition, in patients with thyroid carcinoma, the association of HT is 1.99 times higher among those with PTC than in patients with other pathological types of thyroid cancer11. Indirectly, these findings my suggest a predisposition of HT patients to the development of PTC. In our series we found 26.8% of HT in 41 cases of papillary carcinoma and 6.65% in 198 patients with multinodular goiter (p = 0.005823). Notwithstanding, in the present series there were 45 patients submitted to less-than-total thyroidectomy because of nodular goiter, therefore a benign disease, and in none of them we found thyroiditis, which is explained by the fact that we carried out total thyroidectomy as a routine in cases of nodular disease associated with HT. Thus, these 45 cases could not be included in this statistical analysis.
Therefore, the RET/PTC, which is a RET rearrangement, a gene which codes a tyrosine-kinase receptor, is described as one of the mechanisms responsible for the association of HT and PTC19. This oncogene was found in the large majority of tissues with HT and without detectable PTC, which may show a progression to cancer from chronic thyroiditis15,20. The presence of RET/PTC must not be synonymous with cancer, but rather a molecular mechanisms of carcinogenesis21.
Another mechanism described is the p63 expression, a tumor-suppression protein homologous to the p53, which is found in about 81% of the HT and PTC, and it is not found in normal thyroid tissues, Graves disease or other thyroid tumors17.
In the present study, 26.8% of the cases showed both HT and PTC, which may suggest a correlation, even without control groups for a proper statistical analysis; however, consistent with literature data, reporting that it may vary between 20% and 37.5% 3,22,23.
The predominance of females in this study, in both groups of patients, namely those associated with HT and those without such association, is in agreement with the literature3,5,8,11, an epidemiology matching PTC. It is known that thyroid autoimmune diseases are more commonly expressed in women when compared to men, and such trend is even more obvious in the post-menopausal period. However, our study did not yield statistically significant differences as far as gender is concerned, which may have been caused by the low number of men among the patients. The same can be inferred in relation to the mean age of those involved, there were no differences between the two groups, which is in agreement with the literature, with higher prevalence in individuals around 50 years of age1,2,4.
Among the different stages of the disease, there were no statistically significant differences between the presence and absence of concurrent HT, which is also in agreement with the literature24. Some authors suggest a less aggressive course of the disease when there is association between HT and PTC3,23, with tendency towards a smaller tumor size, less lymph node involvement and longer survival25. A population study did not find statistically significant difference based on the presence of HT, despite a tendency towards a better survival in cases of concurrent diseases11. The metanalysis of three studies, involving 2,552 patients, carried out in the same publication, suggested a better disease-free survival among patients with PTC associated with HT. similarly, the global survival was also higher in this group in four of five studies which analyzed this parameter. The precise reason for such difference is still unclear.
The ultimate confirmation of a causal association between HT and PTC would require a longitudinal prospective study of patients with HT. Right now, the best approach for patients with HT, especially those with the nodular variant of the disease, is a careful follow up, clinically as well as with cytopathological study of the nodules. The surgical approach should be the total thyroidectomy, since the cases of concurrent diseases are more frequently multicentric (93%) when compared to cases without the association (50%)26.
CONCLUSION
There is a rate of 26.8% of patients with the HT-PTC association, however without statistical significance vis-à-vis tumor size. More studies are needed in order to assess the higher development of neoplasia in patients with HT and assess the possible factors which may trigger the carcinogenesis, thus contributing to prevention, early diagnosis and target treatment.
REFERENCES
1. Camandaroba MPG, Mata LS, Almeida LB, Miranda JS, Neves MP. Carcinoma papilífero da tireoide associado à tireoidite de Hashimoto: uma série de casos. Rev Bras Cancerol. 2009;55(3):255-61.
2. Coeli CM, Brito AS, Barbosa FS, Ribeiro MG, Sieiro APAV, Vaisman M. Incidence and mortality from thyroid cancer in Brazil. Arq Bras Endocrinol Metabol. 2005;49(4):503-9.
3. Camboim DC, Figueirôa VMSM, Lima DNO, Abreu-e-Lima P, Abreu-e-Lima MCC. Carcinoma papilífero da tireóide associado à tireoidite de Hashimoto: frequência e aspectos histopatológicos. J Bras Patol Med Lab. 2009;45(1):75-82.
4. Dailey ME, Lindsay S, Skahen R. Relation of thyroid neoplasms to Hashimoto disease of the thyroid gland. AMA Arch Surg. 1955;70(2):291-7.
5. Loh KC, Greenspan FS, Dong F, Miller TR, Yeo PP. Influence of lymphocytic thyroiditis on the prognostic outcome of patients with papillary thyroid carcinoma. J Clin Endocrinol Metab. 1999;84(2):458-63.
6. Kashima K, Yokoyama S, Noguchi S, Murakami N, Yamashita H, Watanabe S, et al. Chronic thyroiditis as a favorable prognostic factor in papillary thyroid carcinoma. Thyroid. 1998;8(3):197-202.
7. Cipolla C, Sandonato L, Graceffa G, Fricano S, Torcivia A, Vieni S, et al. Hashimoto thyroiditis coexistent with papillary thyroid carcinoma. Am Surg. 2005;71(10):874-8.
8. Kebebew E, Treseler PA, Ituarte PH, Clark OH. Coexisting chronic lymphocytic thyroiditis and papillary thyroid cancer revisited. World J Surg. 2001;25(5):632-7.
9. Repplinger D, Bargren A, Zhang YW, Adler JT, Haymart M, Chen H. Is Hashimoto's thyroiditis a risk factor for papillary thyroid cancer? J Surg Res. 2007;150(1):49-52.
10. Sclafani AP, Valdes M, Cho H. Hashimoto's thyroiditis and carcinoma of the thyroid: optimal management. Laryngoscope. 1993;103(8):845-9.
11. Singh B, Shaha AR, Trivedi H, Carew JF, Poluri A, Shah JP. Coexistent Hashimoto's thyroiditis with papillary thyroid carcinoma: impact on presentation, management, and outcome. Surgery. 1999;126(6):1070-6.
12. Crile G Jr, Hazard JB. Incidence of cancer in struma lymphomatosa. Surg Gynecol Obstet. 1962;115:101-3.
13. Crile G Jr. Struma lymphomatosa and carcinoma of the thyroid. Surg Gynecol Obstet. 1978;147(3):350-2.
14. Holm LE, Blomgren H, Löwhagen T. Cancer risks in patients with chronic lymphocytic thyroiditis. N Engl J Med. 1985;312(10):601-4.
15. Wirtschafter A, Schmidt R, Rosen D, Kundu N, Santoro M, Fusco A, et al. Expression of the RET/PTC fusion gene as a marker for papillary carcinoma in Hashimoto's thyroiditis. Laryngoscope. 1997;107(1):95-100.
16. Di Pasquale M, Rothstein JL, Palazzo JP. Pathologic features of Hashimoto's-associated papillary thyroid carcinomas. Hum Pathol. 2001;32(1):24-30.
17. Unger P, Ewart M, Wang BY, Gan L, Kohtz DS, Burstein DE. Expression of p63 in papillary thyroid carcinoma and in Hashimoto's thyroiditis: a pathobiologic link? Hum Pathol. 2003;34(8):764-9.
18. Hashimoto H. Zur Kenntiss der lymphomatosen veranderung der Schilddrusse struma lymphomatosa. Arch Klein Chir. 1912;97:218-48.
19. Zhu Z, Ciampi R, Nikiforova MN, Gandhi M, Nikiforov YE. Prevalence of RET/PTC rearrangements in thyroid papillary carcinomas: effects of the detection methods and genetic heterogeneity. J Clin Endocrinol Metab. 2006;91(9):3603-10.
20. Arif S, Blanes A, Diaz-Cano SJ. Hashimoto's thyroiditis shares features with early papillary thyroid carcinoma. Histopathology. 2002;41(4):357-62.
21. Rhoden KJ, Unger K, Salvatore G, Yilmaz Y, Vovk V, Chiappetta G et al. RET/papillary thyroid cancer rearrangement in nonneoplastic thyrocytes: follicular cells of Hashimoto's thyroiditis share low-level recombination events with a subset of papillary carcinoma. J Clin Endocrinol Metab. 2006;91(6):2414-23.
22. Mazokopakis EE, Tzortzinis AA, Dalieraki-Ott EI, Tsartsalis AN, Syros PK, Karefilakis CM, et al. Coexistence of Hashimoto's thyroiditis with papillary thyroid carcinoma. A retrospective study. Hormones (Athens). 2010;9(4):312-17.
23. Ahn D, Heo SJ, Park JH, Kim JH, Sohn JH, Park JY, et al. Clinical relationship between Hashimoto's thyroiditis and papillary thyroid cancer. Acta Oncol. 2011;50(8):1228-34.
24. Kim SK, Song KH, Lim SD, Lim YC, Yoo YB, Kim JS, et al. Clinical and pathological features and the BRAF(V600E) mutation in patients with papillary thyroid carcinoma with and without concurrent Hashimoto thyroiditis. Thyroid. 2009;19(2):137-41.
25. Huang BY, Hseuh C, Chao TC, Lin KJ, Lin JD. Well-differentiated thyroid carcinoma with concomitant Hashimoto's thyroiditis present with less aggressive clinical stage and low recurrence. Endocr Pathol. 2011;22(3):144-9.
26. Asanuma K, Sugenoya A, Kasuga Y, Itoh N, Kobayashi S, Amano J. The relationship between multiple intrathyroidal involvement in papillary thyroid carcinoma and chronic non-specific thyroiditis. Cancer Lett. 1998;122(1-2):177-80.
1. General Practice Resident Physician at Hospital Ana Costa, Santos.
2. Resident Physician at Hospital Regional do Vale do Paraíba, Taubaté.
3. PhD - Department of Surgery - Medical School of the University of São Paulo. Assistant Physician - Head and Neck Surgery Department at Hospital Ana Costa, Santos.
4. Adjunct Professor and Researcher - Department of Biosciences - Pathology Program - Federal University of São Paulo.
5. MD. Senior Associate Professor - Fundação Lusíada UNILUS.
Department of Head and Neck Surgery - Ana Clara Hospital - Santos.
Send correspondence to:
Rogério A. Dedivitis
Rua Dr. Olinto Rodrigues Dantas, nº 343, conj. 92. Encruzilhada
Santos - SP. CEP: 11050-220
E-mail: dedivitis@usp.br
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on February 4, 2012.
Accepted on August 4, 2012. cod. 9026.