Year: 2012 Vol. 78 Ed. 5 - (21º)
Relato de Caso
Pages: 135 to 135
Clear cell sarcoma of the parotid region
Author(s): Evandro Maccarini Manoel1; Rafael Reiser2; Fábio Brodskyn3; Marcello Franco4; Márcio Abrahão5; Onivaldo Cervantes6
DOI: 10.5935/1808-8694.20120021
Keywords: head and neck neoplasms, neoplasm recurrence, local, parotid region, sarcoma, clear cell.
![]()
INTRODUCTION
Clear cell sarcoma (CCS), also referred to as malignant melanoma of the soft parts, is a rare aggressive tumor that accounts for less than 1% of all soft tissue sarcomas1. It occurs typically as a deep lesion that arises in connection to tendons and aponeuroses, involving the skin only in advanced cases2. It is observed more frequently in adolescents and young adults of both genders, and preferentially affects the lower extremities2. It is rarely seen in the head or neck3.
CASE PRESENTATION
A 43-year-old Caucasian female came to our service complaining of a lump that had been growing in her right parotid region for a year and four months. She had no other symptoms. The patient had well-managed systemic high blood pressure and asthma. Physical examination revealed a tumor in her right parotid region with a diameter of five centimeters. The tumor was hard, barely mobile, ulcerated, hyperemic, and painless to palpation.
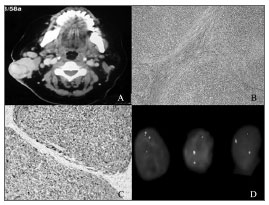
Fine-needle aspiration (FNA) revealed a basaloid neoplasm with low rates of cell proliferation. Head and neck CT scans showed a tumor located in the patient's right parotid region (Figure 1A).
Figure 1. A: Head and neck CT scan showing a heterogeneous tumor with five centimeters in its greater diameter enhanced with contrast in the patient's right parotid region. B: optic microscope; H&E stained slide (magnification 100x). C: Immunohistochemistry assay with diffuse positive result for protein S-100 (magnification 200x). D: FISH test showing rearrangement in gene EWSR1 resulting from translocation t(12;22) (q13;12).
The patient was referred to surgery and underwent a superficial parotidectomy with neck clearance on level II; the accessory nerve was removed as it had been involved by the tumor. Histopathology tests showed the tumor was an undifferentiated malignant neoplasm with a multilobular growth pattern and cells with little amounts of pale cytoplasm, vesicular nuclei, and occasionally prominent nucleoli (Figure 1B). Cell morphology initially indicated malignant melanoma metastasis, but immunohistochemistry revealed diffuse positive results only for protein S-100 (Figure 1C), and negative results for malignant melanoma markers HMB45, Melan-A, MART-1 and MITF. A FISH (fluorescence in-situ hybridization) test showed translocation t(12;22) (q13;q12) (Figure 1D) and changed the diagnosis to CCS.
Eight months after surgery the neck tumor recurred, and the patient was submitted to a radical neck clearance procedure and adjuvant radiotherapy (6600 cGy). The patient has been followed for six months since, and no relapsing tumors have been found.
DISCUSSION
Clear cell sarcoma was first described in 1965 2, and has been known as malignant melanoma of the soft parts because of the histological and immunohistochemical similarities it bears with melanomas1. However, molecular analysis revealed they are distinct tumors, as CCS presents translocation t(12;22)(q13;q12) that results in chimeric gene EWSR1/ATF1, which is not seen in melanomas1. This alteration is also seen in hyalinizing clear cell carcinomas of the salivary glands, angiomatoid fibrous histiocytomas, and in few cases of the recently described gastrointestinal subtype of CCS4. In this case, morphology and absence of melanocytic markers match the diagnosis of this variant2.
Only 1.2% of the approximately 500 reported cases2 of CCS involved the head or neck5. The parotid region was compromised in only three cases reported in the literature3,5,6. CCS generally evolves slowly and painlessly, and is diagnosed while measuring under five centimeters2. It presents high local recurrence and late metastasis rates2 and, contrary to most sarcomas, its metastases appear preferentially in regional lymph nodes. Five and ten-year survival rates are approximately 47% and 36% respectively1. Tumors larger than five centimeters and presence of tumor necrosis mean worse prognosis6. The better therapy appears to be broad excision of the tumor followed by adjuvant radiotherapy2. Given the limited number of reported cases, the role of the neck clearance procedure and systemic adjuvant therapy are still uncertain.
CLOSING REMARKS
Even though they are rare, clear cell sarcomas may involve the head and the neck and are frequently mistaken for malignant melanomas.
ACKNOWLEDGEMENTS
The authors would like to thank Prof. Christopher D. M. Fletcher, pathologist at the Brigham and Women's Hospital (Boston, USA), for his invaluable aid in diagnosing this case.
REFERENCES
1. Kawai A, Hosono A, Nakayama R, Matsumine A, Matsumoto S, Ueda T, et al. Clear cell sarcoma of tendons and aponeuroses: a study of 75 patients. Cancer. 2007;109(1):109-15.
2. Kosemehmetoglu K, Folpe AL. Clear cell sarcoma of tendons and aponeuroses, and osteoclast-rich tumour of the gastrointestinal tract with features resembling clear cell sarcoma of soft parts: a review and update. J Clin Pathol. 2010;63(5):416-23.
3. Poigmonec S, Lamas G, Homsi T, Auriol M, De Saint Maur PP, Castro DJ, et al. Clear cell sarcoma of the preparotid region: an initial case report. Acta Otorhinolaryngol Belg. 1994;48(4):369-73.
4. Antonescu CR, Katabi N, Zhang L, Sung YS, Seethala RR, Jordan RC, et al. EWSR1-ATF1 fusion is a novel and consistent finding in hyalinizing clear-cell carcinoma of salivary gland. Genes, Chromosomes Cancer. 2011;50(7):559-70.
5. Bisceglia M, Carosi I, Lelli G, Pasquinelli G, Martinelli GN. Clear cell sarcoma of soft tissues. Clinico-pathological and ultrastructural analysis of a case in the head-neck region and a literature review. Pathologica. 1998;90(4):391-6.
6. Lucas DR, Nascimento AG, Sim FH. Clear cell sarcoma of soft tissues: Mayo Clinic experience with 35 cases. Am J Surg Pathol. 1992;16(12):1197-204.
1. MD (Resident ENT Physician at EPM-UNIFESP).
2. MD, Head and Neck Surgeon (MD, Head and Neck Surgeon at EPM-UNIFESP).
3. MD, ENT, Head and Neck Surgeon (MD, ENT, Head and Neck Surgeon at EPM - UNIFESP).
4. MSc on Pathology at EPM-UNIFESP (Professor in the Department of Pathology at EPM-UNIFESP).
5. Adjunct Professor in the Department of Otorhinolaryngology and Head and Neck Surgery at EPM-UNIFESP (Vice-head of the Head and Neck Surgery Course at EPM-UNIFESP).
6. Adjunct Professor in the Department of Otorhinolaryngology and Head and Neck Surgery at EPM-UNIFESP (Head of the Head and Neck Surgery Course at EPM-UNIFESP and Chairman of the Brazilian Association of Head and Neck Surgery).
Universidade Federal de São Paulo (EPM-UNIFESP).
Send corresponce to:
Evandro Maccarini Manoel
Rua Dr. Diogo de Faria, nº 539, apto. 67. Vila Clementino
São Paulo - SP. CEP: 04037-001
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on June 6, 2011.
Accepted on June 3, 2012. cod. 8058.
All rights reserved - 1933 /
2025
© - Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico Facial