Year: 2012 Vol. 78 Ed. 4 - (25º)
Relato de Caso
Pages: 134 to 134
Exuberant pyogenic granuloma in extragingival site
Author(s): Fábio Wildson Gurgel Costa1; Ana Thayssa Tomaz Lima2; Roberta Barroso Cavalcante3; Karuza Maria Alves Pereira4
Keywords: granuloma, mouth, pyogenic, tongue.
![]()
INTRODUCTION
Non-neoplastic proliferative processes are a group of disorders relatively common in the oral cavity. Among them we stress the pyogenic granuloma (PG) because of its occurrence, typical classical characteristic presentation and distribution in gingival sites in over 80% of the cases1-7. Nonetheless, when extragingival lesions appear, a rare condition listed in the literature, diagnosis may be late1-7. Thus, this paper aims at reporting a case of exuberant pyogenic granuloma in a non-gingival site.
CASE REPORT
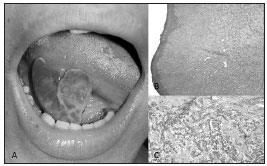
16-year old female black patient came to the stomatology ward of the University Hospital at the Federal University of Ceará, Campus Sobral, complaining of a "growth in her tongue" with pain, bleeding upon touch, perceived two months after an accident. Upon intraoral physical exam (Figure 1A), we spotted a reddish exophytic lesion was seen, with an ulcerated surface, bleeding upon minimum manipulation, soft, measuring approximately 3.0cm in its longest diameter, and located in the posterior region of the right tongue border. Upon extraoral exam, nothing important was noticed. Having that, the main diagnostic considered was that of a pyogenic granuloma. Considering the medical interview and the clinical findings, treatment was based on complete lesion exeresis. In an outpatient ward and under local anesthesia, the material was harvested and sent to histopathology, which matched clinical findings. During surgery, clinical maneuvers were used to minimize bleeding, as a good anesthesia on the basis of the lesion and continuous suture. Upon microscopic examination (Figure 1B-C), they found a thin para-keratinized stratified squamous epithelium with connective tissue, with numerous blood vessels of varied gauges, and these areas were, sometimes, interspersed by inflammatory cells. The patient has been under clinical follow up for 8 months, without signs of recurrence.
Figure 1. A: Clinical view of the exuberant lesion on the tongue; B-C: Microphotography showing thin para-keratinized stratified squamous epithelium with numerous blood vessels (Hematoxylin-eosin, 200x).
DISCUSSION
Granuloma pyogenic development is usually associated with an exuberant response to chronic irritative local factors of low intensity, or trauma, with hormonal factors impacting and, therefore, very often found among pregnant women. It is more prevalent among women in their second to fourth decades of life, and it may involve the skin, lips, tongue, cheek mucosa and palate, being more common in the anterior teeth gingiva.
We carefully reviewed the literature1-7 with comparative purposes, taking as bases the main series of cases published by 2010, making up a total of 1,127 cases and, among these, there were only 79 on the tongue - 7% of the cases. As far as the etiology is concerned, it has been reported that 80% of the patients with extragingival oral pyogenic granuloma responded positively on local injuries where the lesions appeared. The main age range was within the second and third decades of life and females were the most affected in 100% of the cases studied - which corroborated the case hereby reported. The lesion exeresis, as per carried out in the present case, is according to the literature, the best treatment approach for these pyogenic granulomas.
Regarding the low occurrence of PG in extragingival sites, it is pertaining to emphasize the importance of the correct diagnosis of these lesions, distinguishing them from other entities which have similar characteristics, so as to obtain a proper treatment approach. In this paper, we stress the importance of professionals who work with the oral cavity, notably dentists and otorhinolaryngologists, in recognizing hyperplastic reactive lesions, even when located in unusual sites, aiming at an early treatment, without harming the patient.
REFERENCES
1. Zain RB, Khoo SP, Yeo JF. Oral pyogenic granuloma (excluding pregnancy tumour): a clinical analysis of 304 cases. Singapore Dent J. 1995;20(1):8-10.
2. Lawoyin JO, Arotiba JT, Dosumu OO. Oral pyogenic granuloma: a review of 38 cases from Ibadan, Nigeria. Br J Oral Maxillofac Surg. 1997;35(3):185-9.
3. Al-Khateeb T, Ababneh K. Oral pyogenic granuloma in Jordanians: a retrospective analysis of 108 cases. J Oral Maxillofac Surg. 2003;61(11):1285-8.
4. Epivatianos A, Antoniades D, Zaraboukas T, Zairi E, Poulopoulos A, Kiziridou A, et al. Pyogenic granuloma of the oral cavity: comparative study of its clinicopathological and immunohistochemical features. Pathol Int. 2005;55(7):391-7.
5. Avelar RL, Antunes AA, Carvalho RWF, Santos TS, Oliveira Neto PJ, Andrade ESS. Granuloma piogênico oral: um estudo epidemiológico de 191 casos. RGO. 2008;56(2):131-5.
6. Saravana GH. Oral pyogenic granuloma: a review of 137 cases. Br J Oral Maxillofac Surg. 2009;47(4):318-9.
7. Gordón-Núñez MA, de Vasconcelos Carvalho M, Benevenuto TG, Lopes MF, Silva LM, Galvão HC. Oral pyogenic granuloma: a retrospective analysis of 293 cases in a Brazilian population. J Oral Maxillofac Surg. 2010;68(9):2185-8.
1. PhD student of dentistry - UFC (Assistant Professor I - UFC Campus Sobral Dentistry Program).
2. Professor of Dentistry - UFC Campus Sobral.
3. PhD in Oral Pathology - UFRN (Professor of Dentistry - University of Fortaleza (UNIFOR)).
4. PhD in Oral Pathology - UFRN (Adjunct Professor of Dentistry - UFC Campus Sobral).
Federal University of Ceará Campus Sobral.
Send correspondence to:
Fábio Wildson Gurgel Costa
Rua João Sorongo 1016, apto. 205, Jardim América
Fortaleza - CE. Brazil. CEP: 60416-000
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on January 28, 2011.
Accepted on July 23, 2011. cod. 7544.
All rights reserved - 1933 /
2025
© - Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico Facial