Year: 2002 Vol. 68 Ed. 3 - (17º)
Artigo Original
Pages: 405 to 410
Cryptolysis via coagulation with co2 laser for chronic caseous tonsillitis: conservatory technique and results
Author(s):
Cândida Ap. da C. Passos (1),
Flávia M.Z. Olveira (2),
Jorge H. Nicola (3),
Ester M. D. Nicola (4)
Keywords: cryptolysis, CO2 laser, chronic tonsillitis, caseous
Abstract:
Introduction: Conventional cryptolysis with CO2 laser has been performed with success and in this case, a considerable volume of tissue is removed without warring about possible reduction of the immunological function of the tonsils. In the present paper we propose an alternative cryptolysis method with CO2 laser for chronic causeous tonsillitis. In this way, the desired effect is obtained by coagulation with laser and not by the volatilization of the tissues. The preservation of tissues is optimized. Method of study: Clinical prospective. Objectives: To present a modified cryptolysis technique with CO2 laser, which inhibits the retention of the caseous and preserves the tonsilar parenchyma. Material and Method: The cryptolysis were performed on a group of thirty-one individuals with chronic causeous tonsillitis, with great elimination of caseous and other associated symptoms. The patients were selected from the ORL HC-UNICAMP ambulatory. We used 6W CO2 laser in continuous mode, unfocused, and Swiftlase around the opening of the crypts, and, afterwards over the entire tonsilar surface producing only a superficial coagulation. To eradicate the symptoms we performed on average seven applications, repeated every three weeks. Results: The proposed technique was effective in 87% of the cases. For the remaining 13%, it was also necessary to volatize the regions adjacent to the crypts. There was a two-year follow-up without evidence of complications. Conclusion: We conclude this to be a safe and efficient method, able to be performed in the ambulatory under topic anesthesia; therefore, permitting to the patients immediate return to their activities.
![]()
INTRODUCTION
Chronic caseous tonsillitis, which is reported by patients as a discomfort or constant throat irritation, is characterized by isolated elimination of caseous or associated with other symptoms such as halitosis, foreign body sensation on the throat or recurrent tonsillitis. Still, these symptoms may be followed by palatine tonsils hyperemia and hypertrophy, with no hyperthermia, and generally disappear after caseous elimination. This disease may occur at any age, including individuals that never had tonsillar symptoms. It generates discomfort and lack of self-confidence at work and in social life, since the caseous elimination and halitosis may occur at any time. Still, chronic caseous tonsillitis appears in any kind and type of tonsil, uni or bilaterally, and may be mistaken with other neck diseases that have symptoms such as pain or unilateral discomfort of unknown etiology.
The effective treatment indication for chronic caseous tonsillitis is still quite controversial 4,22,29, since the only objective complaint of this disease is caseous deposit that many times is not present in the crypt surface during oroscopy.
Currently, the proposed treatments are: clinical 27,29, with use of antiinflammatory drugs, rinsing the throat by gargling with saline and antiseptic solutions; or surgical, with tonsillectomies, and conventional or laser-assisted tonsillectomies14,16,18,19,25.
Although tonsillectomies are part of routine surgery in ENT, they are not risk free, both on the anesthetic and surgical point of view, and especially they are not free from bleedings. 4,17. In certain cases, it may even be contraindicated due to patients' clinical conditions17,23,24.
Palatine tonsil is the only lymphoid organ directly in contact with the environment 5,15,20,27, and increasingly more individuals are exposed to a growing number of pollutants, viruses, bacteria etc. They are covered by stratified squamous epithelium, which continues down into deep crypts20,21,27. The epithelium lined with crypts is reticular and forms a mechanical barrier against infection dissemination 2,6,15,20,27. Its cells allow antigens transportation and contact with lymphocytes located less than 1mm away from crypt lumen in the extra follicular region of the tonsils. Local production of five classes of immunoglobulins is another defense mechanism of palatine tonsils14,15,23. The most produced one is secretory IgA, which was described by Hanson in 1961 as having the function to decrease bacteria adherence to tonsillar surface without inducing an inflammatory process5,7. The importance of palatine tonsils is widely accepted and acknowledged, however, the age and factors that would lead to changes in tonsils morphology and function are still under discussion6,15,20,21,27.
Figure 1 shows a micrograph (132 times magnification), evidencing the structure of the crypts and the germinal centers of normal tonsils. Thus, the acknowledgement of the architecture of palatine tonsils, primarily the crypts, as a three-dimensional lymphoepithelial organ, with clear immunology function 2,6,19,20 that in principle should be spared , made us look for a an effective therapy to treat chronic tonsils, which was more conservative than those described in literature and used so far.
The effect of CO2 laser in live biological tissue is essentially thermal, and is typically classified into: volatilization- when there is tissue lost caused by its fast heating by relatively high laser power density. In this case, the temperatures achieved are higher than 1000 C, in relatively short time. Coagulation - it is achieved with moderate power densities of CO2 laser, per intervals of seconds, reaching temperatures from 50 to 100oC in the tissue with subsequent dehydration, bleaching and contraction of tissues by protein and collagen denaturation. Hyperthermia - is obtained by keeping temperatures from 41 to 44oC in the tissue for several minutes, resulting in cellular death caused by enzymatic changes. This process can only be achieved by using very low power densities of CO2 laser 9,10,11,12,13.
CO2 laser has been used in tonsillectomy for more than twenty years 3,11,26, however, even in the particular case of cryptolysis, the procedures described are performed by tonsil's volatilization to the extent of the anterior pillar line, with significant parenchyma reduction. In such cases, CO2 laser is used continuously, focused and with relatively high power of up to 18 W14,16.
References on the use of the CO2 laser on coagulation basis, for the treatment of chronic caseous tonsillitis, as proposed in this paper, were not found in the literature review.
OBJECTIVE
To present and assess the outcomes of a cryptolysis method using coagulation process by CO2 laser to find a more conservative outcome that preserve tonsillar parenchyma and is effective in opening the crypts and treating the symptoms, in other words, caseous deposit and elimination.
MATERIAL AND METHODS
Sampling: A prospect study was carried out in thirty (31) adults (13 male and 18 female) with chronic caseous tonsillitis, with constant caseous elimination as the main symptom and mean age of 28 years. This study was evaluated by the Ethics Committee of FCM/ UNICAMP.
Equipment: CO2 laser (Sharplan 40C), rated power (40 W), coupled to hinged arm knife-pen and scanning device (Swiftlase). Smoke aspirator with biological filter, protection goggles for the patient and the surgery staff. Photophore to illuminate the oropharynx.
Method: Patients were selected for this study according to the following criteria:
· Comprehensive and specific otorhinolaryngological evaluation for previous diagnosis and treatment of the diseases of the aerodigestive tract, such as allergies and gastroesophageal reflux, which may mask the diagnosis of chronic caseous tonsillitis.
· Diagnosis of chronic caseous tonsillitis for more than one year, with caseous elimination as major symptom, that could be isolated or followed by other symptoms such as halitosis, foreign body sensation in the tonsils /or tonsillitis episodes.
Patients received outpatient care in the Multidisciplinary Care Unit of Laser Medicine (UMML) of HC/UNICAMP, procedure was conducted with application of two or three sprays of topical anesthetic (Lidocaine spray 10%) over palatine tonsils' surface. No previous medicine was prescribed before the application.
Coagulation technique with CO2 laser always consisted of laser applications in scanning mode with 6W power, continuous, unfocused, initially applied adjacent to the crypts, following their opening format and subsequently applied over all tonsillar surface still in the scanning mode. The tip of the pen did not touch palatine tonsils, and was kept aligned with labial commissure.
This procedure was repeated every three weeks, always under the same conditions after symptoms disappeared. After applications, patients were instructed to avoid ingestion of acid, spicy or hard food during the first two days. Patients were evaluated before each laser coagulation procedure on tonsils' symptoms and appearance. Photographic documentation was standardized for light, approximation and type of film and was always performed between the first and third application and the final treatment, constituting a key element to follow up treatment outcome. Photographic documentation enabled the assessment of parameters such as tonsil size, surface appearance, changes in the crypts and caseous presence. Clinical criterion for discharge was based on improvement of symptoms. All patients were examined every three months after discharge for at least two years. Figures 2 and 3 show the appearance of tonsils that were observed before and immediately after laser coagulation procedure.
Photo 1.
Photo 2.
Photo 3.
Photo 4.
Photo 5.
Photo 6.
Photo 7.
Photo 8.
RESULTS
The analysis of sampling data enabled the recording of some facts related to major complaint. Besides caseous elimination, constant in all patients, other symptoms may be present, and are part of chronic caseous tonsillitis such as halitosis (h), sensation of foreign body in the throat (c.e.) and tonsillitis (t), as plotted in Graph 1.
The occurrence of caseous associated with two or three of the symptoms mentioned above, according to Graph 2, is common. The association of caseous with other two symptoms is the most frequent one and was distributed as follows:
· tonsillitis sensation of foreign body (7 patients),
· tonsillitis and halitosis (5 patients) and,
· halitosis and sensation of foreign body (1 patient)
Symptom elimination by using the method proposed in this study, more specifically caseous deposit, required an average of (06) six laser applications, as shown in Graph 3.
At the end of the treatment with CO 2 laser coagulation the surface of the tonsils presented the following macroscopic aspects:
· opened crypts, with initial architecture sustained and absence of caseous deposit (Figure 4);
· Regular tonsillar surface, with apparent reduction of the number of crypts due to their larger opening and flattening. Absence of caseous deposit (Figure 5);
· Smooth tonsillary surface, with great reduction in the total number of crypts and appearance of a large crypt, generally located in the upper pole, known as "pocket" (Figure 6);
Another important aspect found during the treatment was the decrease in size of tonsils, (25 patients (80,7%), ( see Figure 7 and 8). The most frequent reduction rate was grade 1 (one), according to Graph 4, considering "grade 1" those tonsils within the boundaries of the tonsillar site behind the pillars; "grade 2", tonsils surpass anterior pillar; "grade 3", tonsils occupy the space between anterior pillar and the uvula, and "grade 4", tonsils are near or are touching the uvula.
Figure 1.
Graph 1.
Graph 2.
Graph 3.
Graph 4.
DISCUSSION
The treatment method of chronic caseous tonsillitis, developed in this study, took into account the wish to preserve palatine tonsils, since they are the primary defense barriers of our organism 2,5,6,8,15,20,21. In this technique, which is more conservative than conventional CO2, laser technique, the interaction laser-tissue occurs only superficially, as explained before, leading to minimal changes in germinal center lymphocytes or even in the 3D architecture of the tonsils1.
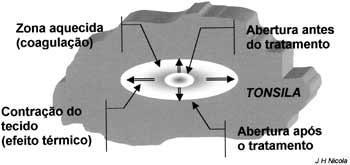
Upon treating tonsils with 6 W powers, unfocused laser beam or scanning mode, we ensure coagulation9,10,12, as previously described, and not tissue volatilization as is the case of conventional CO2 laser procedures14,16,25. Tissue volume was immediately preserved from laser action, which had only a superficial thermal effect of low penetration but enough to cause contraction along the surface and subsequent mechanical opening of treated crypts (see Figure 1). The procedure facilitates elimination of internal crypt desquamation and other residues, preventing caseous deposit formation and retention. Still to facilitate even more the procedure above-described, it begins with repeated and longer laser applications directly to the edge of the treated crypt with the purpose of increasing tissue fragility, taking care not to cauterize it. In this case, cauterization is undesirable since it could lead to healing process and subsequent fibrosis around the crypt surface, preventing its opening. During two-year follow-up, it was found that after CO2 laser application using this technique, treated palatine tonsil behaved against external stimuli similarly to normal tonsils.
The absence of trauma, exerted by caseous deposit on crypt walls, contributes to remission of palatine tonsil inflammation, which could explain their decrease in size.
In palatine tonsils, crypts with different depth are interconnected through microcrypts forming an actual three-dimensional network of channels1,6. In some particular cases, several crypts may open into a single concavity forming what is known as pocket, having as major characteristic a large caseous deposit16. In the sample studied, the presence of such structures was found in 7 cases, three of them already had it in the beginning of the treatment and coagulation technique was equally effective in such cases. In the other four cases, the "pocket" was found during treatment. Certainly, there should be a predisposition for it owing to the closeness of several crypt openings, which coalesced due to changes in tonsils tensile surface caused by the thermal effect of CO2 laser volatilizing tonsil parenchyma16. These four "pocket" cases presented difficulties during the coagulation technique, requiring higher density power laser application volatilizing small regions of their lateral wall. In terms of percentage, these four cases accounted for 13% of total cases treated.
Still, different results were found between two tonsils of the same individual, both in number of applications and in final appearance of the tonsils, evidencing each organ uniqueness.
The use of analgesic drugs was left at patients discretion, and was not used in most cases.
During the follow-up period after the final treatment, no cases of peritonsillar or tonsillar abscess were reported. The symptoms of chronic caseous tonsillitis lessened considerably, with no reports of recurrence.
CONCLUSION
The use of CO2 laser, with the technique and power described in this study, constituted a new effective approach to treat chronic caseous tonsillitis ceasing caseous deposit and preserving palatine tonsils functions. It is an excellent alternative treatment for patients whose indication for tonsillectomy represents risk and increased morbidity for them. It is easy to perform, but its success depends on precise indication and expertise of the surgeon operating the laser equipment.
Hospital discharge, specific anesthetic use, as well as symptomatic medication after the procedure and the likelihood of immediately resuming professional activities are inherent advantages of this treatment, which surpass the inconvenient multiple CO2 laser applications.
REFERENCES
1. Abbey K, Kanabata I. Computerized three-dimensional reconstruction of the crypt system of the palatine tonsil. Acta Otolalaryngol (Stöckh) 1988;454:39-42.
2. Altemani A, Endo LH, Chone C, Idagawa E. Histopathological concept of chronic tonsillitis in children. Acta Otolaryngol (Stöckh) 1996;523:14-16.
3. Aronoff BL. Lasers: reflections on their evolution. J Surg Oncol 1997;64:84-92.
4. Bluestone CD. Current indications for tonsillectomy and adenoidectomy. Ann Otol Rhinol Laryngol 1992;155:58-64.
5. Cruz OLM, Costa SS. Imunofisiologia do anel linfático de Waldeyer. In: Costa SS, Cruz OLM, Oliveira JA de; et col. Otorrinolaringologia - Princípios e Prática. 1a. ed. Porto Alegre: Artes Médicas, 1994. p.381-3.
6. Endo LH; Vassalo J. Amigdalite Crônica. Acta AWHO 1990;9:124-132.
7. Hanson LA. Comparative immunological studies of the immune globulins of human milk and of blood serum. Arch Allergy Appl Imunol 1961;18:241.
8. Betti ET, Lopes Fo O. Anginas - Indicação Cirúrgica de Adenoidectomia e Amigdalectomia. In: Lopes Fo O, Campos CAH. Tratado de Otorrinolaringologia. 1a ed. São Paulo: Roca; 1994. p.169-179.
9. Nicola EMD. Caracterização de Microlesões Produzidas por Laser de CO2, na Mucosa Oral de Cães, em Função da Variação de Parâmetros Intrínsecos do Equipamento. [Tese de Doutorado- Universidade Estadual de Campinas]. Campinas, SP; 1984.
10. Nicola EMD, Coutinho AA, Nicola JH, Metze K. Comparative Histologic Study of Alterations in Rat Skeletal Muscle due to Carbon Dioxide Laser with Varying Power but Constant Energy. Laser - Tissue Interaction, Tissue Optics and Laser Welding III. 1998; vol.3195:306-13.
11. Nicola EMD, Coutinho AA, Nicola JH. Minimal invasive method to treat hemangiomas of the oral cavity with a CO2 laser. Lasers in Dentistry III. 1997;Vol 2973:189-196.
12. Nicola EMD, Nicola JH. Low Power CO2 Laser in the Treatment of Chronic Pharyngitis: a five year experience. Laser Surgery: Advanced Characterization, Therapeutics, and Systems IV.1994;Vol.2128:85-7.
13. Nicola EMD, Coutinho AA, Nicola JH, Gusmão RJ. Symptomatic Hemangioma of Oral Cavity Treated with CO2 Laser. Laser in Surgery: Advanced Characterization, Therapeutics and Systems V. 1995;Vol.2395:189-95.
14. Kamami YV. Laser CO2 for snoring, preliminary results. Acta Otorhinolaryngol BELG; 1990:451-6.
15. Kempen MJP Van, Rijkers GT, Cauwenberge PB Van. The immune response in adenoids and tonsils. Int Arch Allergy Immunol 2000;122:8-19.
16. Krespi YP. Tonsil cryptolysis using CO2 Swift Laser. Operative techniques in Otolaryngology - Head Neck Surg 1994;5:294-297.
17. Molina FD, Maniglia JV, Magalhães FP, Dafico SR, Rezende R. A eficácia de subgalato de bismuto em tonsilectomias como agente hemostático. Rev Bras ORL 2000;6:194-7.
18. Oas RE Jr, Bartels JP. KTP-532 Laser tonsillectomy: a comparison with standard technique. Laryngoscope 1990;100:385-8.
19. Patrocínio LG, Patrocínio JA, Coelho SR, Amaral PM, Patrocínio TG. Amigdalectomia a laser de CO2. Rev Bras ORL 2001;67:327-31.
20. Perry M, Whyte A. Immunology of the tonsils. Immunology Today 1998;19:414-21.
21. Perry ME, Jones MM, Mustafa Y. Structure of the crypt epithelium in human palatine tonsils. Acta Otolalaryngol (Stöckh). 1988;454:53-59.
22. Pirana S, Bento RF, Camara J. Consensos e controversas nas indicações de adenoamigdalectomia entre pediatras e otorrinolaringologistas (indicações de adenoamigdalectomia). Rev Bras ORL 1999;65:308-15.
23. Roitt I, Brostoff J, Male D. Sistema linfóide. In: Imunologia. 1a.ed. São Paulo: Manole; 1999. p.31-41.
24. Sant'anna GD, Mauri M, Silva BD, Junior HC. Dor pós- tonsilectomia: comparação entre pacientes com diferentes idades. Rev Bras ORL 2000;66:123-7.
25. Supiyaphun P, Siricharoesang S. Treatment of tonsillar crypt infection with CO2 laser: a preliminary report. J Med Assoc Thai 1996;79:132-6.
26. Takac S, Stojanovac S. Characteristics of laser light. Med Pregl 1999;52:29-34.
27. Weckx LL, Teixeira MS; Hirata H. Amigdalites agudas e crônicas. Rev Bras Med 1996;53:9-19.
28. Weckx LL,Yin L. "Como Diagnosticar e Tratar" adenoidite amigdalite faringite. Rev Bras Med 1993;40(09).
29. Yoshida A, Okamoto K. Indications of tonsillectomy for recurrent tonsillitis. Acta Otoryngol (Stöckh). 1988;454:305-312.
[1] Otorhinolaryngologist, Master studies under course in Medical Sciences, FCM / UNICAMP.
[2] Resident physician, Department of. Ophthalmology and Otorhinolaryngology, FCM / UNICAMP.
[3] Ph.D. in Physics, Guest Researcher and Head of the Laboratory of Anemometer Laser-Doppler, Nucleus of Medicine and Experimental Surgery, FCM/ UNICAMP.
[4] Ph.D. in Medicine, Professor, Department of Ophthalmology and Otorhinolaryngology, Coordinator of the Multidisciplinary Unit of Laser Medicine, HC / UNICAMP; Head of the Laser Laboratory and Nucleus of Medicine and Experimental Surgery - FCM / UNICAMP.
Multidisciplinary Unit of Laser Medicine HC-UNICAMP, Discipline of Otorhinolaryngology, Dept OFT/ORL, FCM, Universidade Estadual de Campinas - UNICAMP, Campinas, SP, Brazil
E-mail: enicola@fcm.unicamp.br
Preliminary draft presented as poster at 35º Congresso Brasileiro de Otorrinolaringologia, held in Natal, RN, October 16 - 20, 2000.